Abstract
Aims: To characterise the clinical course of patients who had incidental findings on the CT aortogram (CTA) done as a transcatheter aortic valve implantation (TAVI) work-up investigation.
Methods and results: All patients who underwent CTA as a work-up investigation for TAVI were retrospectively recruited (n=295, 83±6.7 years) to identify those with an incidental finding. A total of 323 incidental findings were identified in 201 (68.1%) patients. Of those with incidental findings, 87 (43.3%) had at least one of immediate clinical significance. Within this group, fewer (52.9%) eventually had TAVI compared to those without incidental findings (63%). In patients going on to have TAVI, the time between CTA and TAVI was longer in those with incidental findings (median 96 vs. 81 days). At follow-up, overall mortality in those with incidental findings was higher than in those without (49.4% vs. 37.5%). In patients who underwent TAVI, there was a trend to increased mortality in those with incidental findings (34.8% vs. 21.4%, p=0.07).
Conclusions: Incidental findings were associated with a longer time to TAVI procedure, lower chance of eventually receiving TAVI as definitive therapy and a worse overall outcome. Such findings are clearly important and should be taken into account when delivering a contemporary TAVI service.
Introduction
The computed tomography aortogram (CTA) has become an essential investigative tool for the assessment of patients with severe aortic stenosis undergoing work-up investigation for transcatheter aortic valve implantation (TAVI)1-3. Invaluable information regarding the anatomy of the aortic annulus is obtained from the CTA, as well as additional information about the size, tortuosity and calcification of the iliofemoral arteries4,5. Coincidentally, CTA identifies pathologies that are not directly relevant to the TAVI procedure, but which may have an important impact on the decision-making process. These “incidental findings” can range from subtle benign pathologies to malignant or prognostically important non-cardiac disease and are increasingly identified due to the increased resolution of the scanners available in most centres. These findings are common in the patient group referred for TAVI, which comprises patients who are older with multiple comorbidities. In reality, incidental findings are frequent topics of the multidisciplinary “Heart Team” discussion and often complicate otherwise straightforward case review. We aimed to characterise the clinical course and outcome of patients who had incidental CTA findings and to compare them to those patients in whom no such findings were apparent.
Methods
PATIENTS
The TAVI programme at King’s College Hospital in London started in August 2007. This involves a “Heart Team” approach to assess patients’ suitability for TAVI and to manage their pre- and post-operative care. CTA is performed in all patients who undergo TAVI assessment, although the use of radiopaque contrast agents is limited in patients with significant renal impairment. We retrospectively analysed all patients who underwent CTA as part of their assessment for TAVI from August 2007 to October 2012.
CT PROTOCOL
A non-ECG-gated contrast-enhanced multidetector CT (GE LightSpeed VCT 64 slice scanner; GE Healthcare, Little Chalfont, Bucks, United Kingdom) scan was used for image acquisition. To assess iliofemoral vessels, aorta and root angulation, volume-rendered three-dimensional (3D) reconstruction was performed. A total volume of 80 ml contrast agent (Omnipaque™ [iohexol] injection; GE Healthcare, Bangalore, India) was administered through an intravenous line at a flow rate of 4 ml/s. For optimal contrasting, a bolus tracking technique was applied.
DEFINITIONS
All incidental findings were documented for individual patients and divided into those which were of “immediate clinical significance” (ICS) and those which were of “non-immediate clinical significance” (NICS). The ICS incidental findings were categorised as those which needed to be assessed and investigated further, referred on to another specialist or at least discussed with another specialty before making the decision about TAVI. The NICS incidental findings were those that were identified, but were not deemed by the Heart Team to require immediate action before TAVI.
FOLLOW-UP
All patients who underwent TAVI are followed up in our centre at one, three and six months post TAVI with annual review thereafter. Mortality data for all patients (including those who did not have a TAVI) were obtained from the NHS spine summary care record (SCR) database, which is a centralised database that is updated on a weekly basis and provides 100% mortality tracking. This was obtained using automatic flagging for the date of death with the unique NHS number (available for all patients in the UK).
STATISTICS
Continuous data are presented as mean±standard deviation unless stated otherwise, and categorical data are presented as categories with percentages. Fisher’s exact test was used to compare categorical data and the Mann-Whitney U test was used to compare continuous data. Kaplan-Meier methods were used to assess the survival at follow-up; comparisons were made with the log-rank test. A two-tailed p-value of <0.05 was considered significant. Cox proportional hazard survival analysis was performed to identify the predictors of all-cause mortality with the following covariates in the model: age, gender, TAVI and the presence of ICS. All statistical analyses were performed on SPSS version 20 (IBM Corp., Armonk, NY, USA).
Results
During the study period, 295 patients (mean age 83±6.7 years, range 53 to 97 years) with severe aortic stenosis (peak pressure gradient [PPG] 81±24 mmHg, mean pressure gradient [MPG] 46±15 and aortic valve area [AVA] of 0.7±0.2 cm2) underwent CTA for TAVI assessment in our centre. A total of 323 incidental findings were identified in 201 (68.1%) patients (95 male). The most common incidental finding was pulmonary in nature (Table 1). Figure 1 shows the flow chart of patients who underwent CTA and the findings. Of the 201 patients who had incidental findings, 87 (43.3%) had at least one incidental finding of ICS and, of these, 46 (22.9%) went on to have a TAVI procedure after further assessment and/or investigation. Among the remaining 41 patients (20.4%) who had ICS incidental findings (who did not undergo TAVI), 30 (14.9%) patients were deemed not suitable for TAVI due to the incidental finding itself, whilst in the 11 others (5.5%) there were other reasons not to perform the TAVI procedure. Of these 11 patients, four patients had surgical AVR and seven were considered unsuitable for TAVI (four due to anatomical reasons and three for medical reasons). Those patients who had an incidental finding of ICS were less likely to go on to have a TAVI (Figure 2).
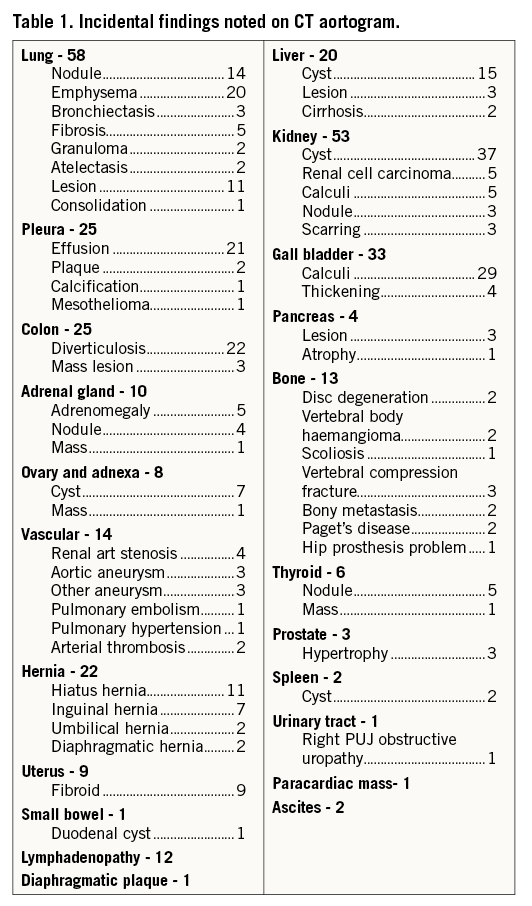
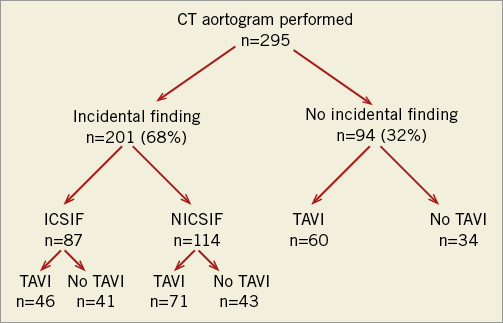
Figure 1. Chart showing the flow of patients who underwent CT and their outcome. ICSIF: immediate clinical significance incidental finding; NICSIF: non-immediate clinical significance incidental finding; TAVI: transcatheter aortic valve implantation
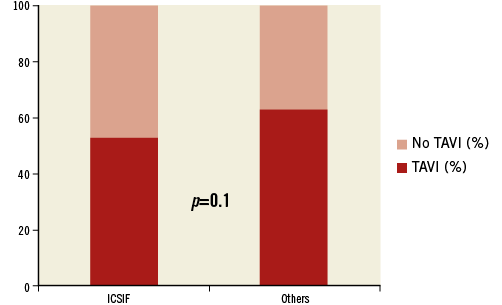
Figure 2. Bar chart showing patients who had TAVI and those who did not have a TAVI procedure in both groups. ICSIF: immediate clinical significance incidental finding
In those patients who did not have any incidental finding on their CTA (n=94), 34 (36.2%) did not undergo a TAVI procedure: three had surgical AVR, seven were found to have only moderate aortic stenosis, six patients had accompanying severe mitral valvular disease, 14 patients were considered unsuitable for TAVI (four for anatomical reasons, ten for other medical reasons), two patients had percutaneous coronary intervention due to severe coronary artery disease leading to symptom improvement, and two patients declined the procedure.
At one year, the mortality rate for patients who had ICS incidental findings was higher at 37.9% (33/87) when compared to the mortality rate of 27.4% (57/208) in all other patients who underwent CTA, but this did not reach statistical significance (p=0.1). Over the whole follow-up period (median 21 months, IQR 10:36 months), patients with an incidental finding of ICS had a significantly higher mortality, as shown in Figure 3. On Cox regression analysis of all patients, ICS was independently associated with an increased risk of all-cause mortality (HR 1.5, 95% CI: 1.0 to 2.2, p=0.04) after correcting for treatment (TAVI), age and gender. TAVI was associated with improved survival (HR 0.3, 95% CI: 0.2 to 0.4, p=0.0001).
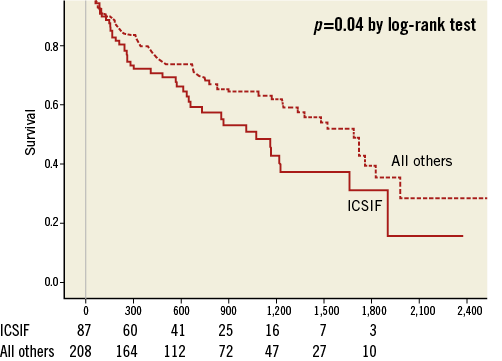
Figure 3. Kaplan-Meier survival curve comparing patients who had ICS incidental finding with others. ICSIF: immediate clinical significance incidental finding
Out of the total cohort of 295 patients, 177 (60%) went on to have a TAVI procedure. The mortality rate was significantly higher in patients who did not undergo TAVI when compared to those who underwent the procedure, both at one year (46.6% vs. 19.8%, p<0.0001) and at the latest follow-up (65.3% vs. 24.9%, p<0.0001). This is most likely to be due to appropriate clinical case selection. Also, in patients with ICS (n=87), the mortality was significantly higher in patients who did not undergo TAVI (27/41, 65.9%) when compared to those who had a TAVI (16/46, 34.8%), p=0.005.
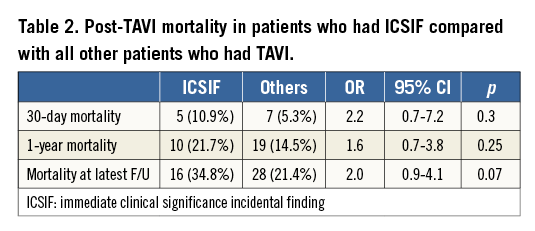
In patients who underwent TAVI, the time interval between CTA and the TAVI procedure was longer (median 96 days) in those who had an ICS incidental finding when compared to the others who underwent TAVI (median 81 days) (Figure 4). The one-year mortality was similar in both groups (21.7% vs. 14.5%, respectively, p=0.25). However, at the latest median follow-up period of 21 months, there was a trend towards increased mortality in patients who had an ICS incidental finding who underwent TAVI (after further assessment) when compared to all others who underwent TAVI (34.8% vs. 21.4%, p=0.07) (Table 2).
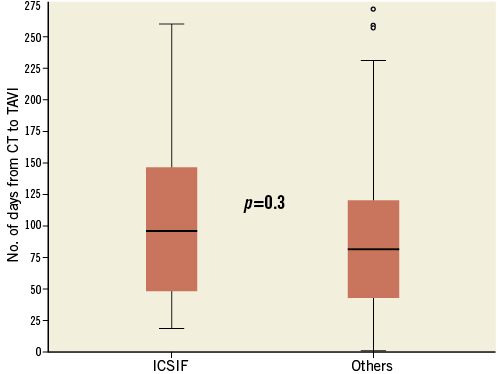
Figure 4. Bar chart showing number of days from CT scan to TAVI procedure in patients who had an ICS incidental finding and others. ICSIF: immediate clinical significance incidental finding
Discussion
This study indicates that the majority of patients who undergo CTA in the work-up for TAVI are found to have incidental findings. This is the first study to report the rate and nature of incidental findings from CTAs in patients undergoing TAVI work-up, thus highlighting an important clinical and resource issue.
Previous studies have been published reporting incidental findings from CT scans in various patient populations, including trauma patients6-8, those assessed for renal colic9 or breast cancer10, those presenting in the emergency department11, and children with head injury12. The rate of incidental findings ranged from 7% to 45% in these studies. There have also been studies to assess the rate of incidental findings in patients undergoing coronary CT angiography. In symptomatic patients with known or suspected coronary artery disease, incidental findings were noted in 58% of patients who underwent contrast-enhanced cardiac CT13 while, in asymptomatic patients undergoing non-contrast chest CT for the detection of coronary artery calcium, the rate of such findings was only 8%14. In a separate study, non-coronary findings were seen in 45% of patients undergoing coronary CT15. The rate of such findings was lower in all these studies compared to our findings, probably because of the increased age of our patient group.
Our study was underpowered to detect the clinical impact of incidental findings on outcome. There was a slight delay between CT scan and TAVI procedure in patients who had ICS incidental findings when compared to others who went on to undergo TAVI. At one year, there was no mortality difference between these groups, but at the latest follow-up there was a trend to increased mortality in ICS patients who eventually underwent TAVI. It is difficult to interpret whether the time delay is in any way responsible for the increased mortality noted in patients who had ICS incidental findings and then went on to have TAVI, although a delay in the treatment of critical, symptomatic aortic stenosis is likely to affect mortality if it is long enough. Interpretation is only hypothetical on the basis of these data.
It is also important to note that 35% of patients who had ICS incidental findings (30 out of 87) were deemed not suitable for TAVI due to the finding itself. These patients’ symptoms did not relate to the finding prior to undergoing the scan, and the diagnosis would not have been made unless they had had their TAVI work-up investigations.
The higher mortality in the ICS incidental finding group is likely to be due to natural and appropriate clinical selection, with the poor prognosis either being due to the finding itself or to the fact that the finding resulted in lack of treatment of critical aortic stenosis.
Limitations
This is a small, single-centre observational study and therefore subject to all the limitations inherent in this kind of report. Interpretation of the observations is therefore restricted to conjecture and hypothesis generation. However, it highlights an important “real-world” clinical scenario which will resonate with many TAVI-practising clinicians. These observations have implications for both clinical management and case selection as well as resource/cost-effectiveness analysis.
Conclusion
Incidental findings of immediate clinical significance appear to be associated with: a) a longer time to a TAVI procedure; b) a lower chance of eventually receiving a TAVI as a definitive therapy; and c) a worse overall outcome. Such findings are clearly important for case selection and “Heart Team” discussion and should be taken into account when designing, supervising and auditing a contemporary TAVI service.
| Impact on daily practice Incidental findings on CT scans in patients undergoing TAVI work-up have never been reported before. Significant numbers of patients were found to have an incidental finding (IF) on their CT scan in our study. Those patients who had an IF of immediate clinical significance were found to have a lesser chance of having TAVI, a longer time delay to the TAVI procedure as a definitive therapy, and worse overall outcomes. |
Conflict of interest statement
The authors have no conflicts of interest to declare.