Abstract
Aims: This study aimed to compare air (AIR) and ground transport (GRD) of STEMI patients bound for primary percutaneous coronary intervention (pPCI).
Methods and results: This was a prospective, controlled, observational study, including patients in whom STEMI was suspected outside a 30-minute driving distance from the PCI centre. AIR patients in a 12-month period (May 1, 2010, to April 30, 2011) were compared with GRD patients in a 16-month period (January 1, 2010, to April 30, 2011). The primary endpoint was time from ECG consistent with STEMI to arrival in the cardiac catheterisation laboratory. We included 450 patients, 114 AIR and 336 GRD patients. The median (5-95% range) transport distance was 97 (62-162) vs. 94 (64-172) kilometres, respectively (p=0.01). Time from ECG to cardiac catheterisation laboratory arrival was significantly lower in the AIR group (median 84 minutes (60-160) vs.104 minutes [63-225], p<0.01). Time from ECG to balloon was 114 (78-221) minutes vs.132 (84-262) (p<0.01), respectively. The 30-day mortality was 2.2% (2/91) for AIR and 6.9% (18/262) for GRD patients (p=0.10). One-year mortality was 6.7%, (6/90) vs. 9.9% (26/262) (p=0.35), respectively.
Conclusions: Air transport seemed superior to ground transportation in reducing time from ECG diagnosis to arrival in the catheterisation laboratory for STEMI patients outside a 30-minute driving distance to the PCI centre.
Introduction
Early reperfusion in patients with ST-segment elevation myocardial infarction (STEMI) is essential1. Although primary percutaneous coronary intervention (pPCI) is the preferred revascularisation technique2, it often involves a longer primary transportation or secondary inter-hospital transfers and thus longer system delay3. Guidelines state that optimally PCI should be performed within 120 minutes from first medical contact4, and reducing delay to PCI improves functional outcome and reduces long-term mortality5. Regionalisation of PCI treatment challenges the pre-hospital treatment, triage and transport of STEMI patients, and the emergency medical services (EMS) play an important role. Air transportation by helicopter is integrated in transport of STEMI patients from emergency departments in various parts of the world and is well accepted when distances are long and road conditions unfavourable6. The role of helicopters in direct referral from closer pre-hospital locations is, however, uncertain, and the actual advantages over ground transportation are sparsely documented7,8.
This study aimed to compare air (AIR) versus ground transport (GRD) of STEMI patients on time to arrival in the PCI centre after implementation of a physician-staffed helicopter in a highly developed regional STEMI network. We hypothesised that transport by AIR would reduce time from ECG diagnosis (indicating STEMI) to arrival at cardiac catheterisation laboratory (CCL) compared to GRD, even in a rather small region. Furthermore, we aimed to assess whether the use of AIR transport had an impact on short- and long-term mortality for patients who had pPCI.
Methods
This was a single-centre, prospective, controlled, observational study conducted between January 1, 2010, and April 30, 2011, on STEMI patients transported to our PCI centre. We decided to include GRD patients as soon as the trial period with the physician-staffed helicopter was announced. This was done in order to increase the number of GRD patients and allowed us to assess the 24-hour ground ambulance system before the helicopter entered the system.
THE STUDY POPULATION
We included patients arriving at the PCI centre of Copenhagen University Hospital, Rigshospitalet, who: 1) were diagnosed with STEMI and had coronary angiography; and 2a) had an actual ground transport time of at least 30 minutes; or 2b) were transported by AIR. Transport time used for inclusion of GRD patients was calculated from “departure from scene” to “arrival at Copenhagen University Hospital” as recorded by the ground ambulance staff. We compared patients transported by AIR in a 12-month period (May 1, 2010, until April 30, 2011) with patients transported by GRD in a 16-month period (January 1, 2010, until April 30, 2011). We collected data on demographics, comorbidity, driving distance, time of symptom onset, diagnostic ECG, and pre-hospital, in-hospital and procedure-specific time intervals, pre-procedural clinical status and relevant procedural characteristics. The patients included were divided into two groups: “field triaged” and inter-hospital transfers. If an ECG showing STEMI was recorded by EMS out-of-hospital and the patient had been triaged for transport to the PCI centre, the patient was registered as field triaged. If the ambulance had a rendezvous with a physician-manned mobile emergency care unit (rapid response car) or a medical transport team at the nearest emergency department, the stopover time was included in the outcome measure. If the ECG showing STEMI was recorded in-hospital, then the patient was registered as an inter-hospital transfer.
Mortality data were recorded using the daily updated Danish Civil Registration System, where all patients are identified by the unique 10-digit identification number that all Danish citizens are assigned at birth or immigration9.
OUTCOME MEASURES
We chose the specific “time interval” presumed modifiable by the AIR transport for both field and inter-hospital transports as outcome measure. Hence, the primary endpoint was time from first ECG consistent with STEMI to arrival in the cardiac catheterisation laboratory. Secondary endpoints were PCI-related delay (defined as time from ECG diagnosis to balloon), 30-day, and one-year mortality for those who underwent pPCI.
THE REGIONAL STEMI NETWORK
Denmark is a North European country with a population of 5.5 million. A physician-staffed helicopter (AIR) was implemented as the first civilian helicopter-based EMS (HEMS) in Denmark from May 1st 2010 onwards as a supplement to the existing pre-hospital system. The intervention period was fixed to one year beforehand. The helicopter operated in daylight hours (mean 11.3 hours per day) and was staffed with a consultant anaesthesiologist experienced in pre-hospital emergency medicine, a paramedic (HEMS crew member) and a pilot. It operated in Eastern Denmark covering an area of 8,400 km2, with a maximum distance to the PCI centre by road of 185 km, and an eligible population of approximately 1.1 million (Figure 1).
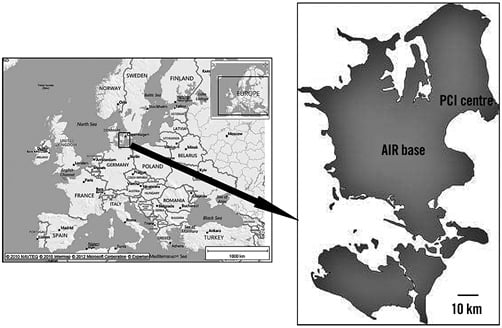
Figure 1. Map of Europe and map of Eastern Denmark (right) with base of physician-staffed helicopter (AIR) and location of PCI centre.
The national reperfusion strategy in Denmark states that all patients having STEMI should be transported directly to a PCI centre for acute coronary angiography and primary PCI if indicated10,11. Fibrinolytic therapy is seldom used, even if the PCI-related delay exceeds 120 minutes. The regional PCI centre covers a total population of 2.5 million, has a 24/7 available catheterisation laboratory team, and performs approximately 2,400 PCI per year, including 1,000 pPCI.
When STEMI was suspected by EMS providers or hospital staff the 12-lead ECG was transmitted to the attending triaging cardiologist at the PCI centre. All ambulances in Denmark are capable of recording 12-lead ECGs and transmitting them to the PCI centre from the field. If the patient was accepted for transport to the PCI centre, the dispatch centre was contacted in order to coordinate transportation. Prior to implementation, programme directors developed a dispatch protocol stating that AIR transport could be secondarily dispatched to STEMI patients if the dispatch centre, based on location and condition, expected a ground transport time exceeding 30 minutes. This meant that the AIR transport was not sent as “first responder” to patients in whom myocardial infarction was suspected. Thus, if helicopter transport was indicated, a rendezvous with the ground ambulance already attending the patient was arranged.
There were seven referring non-PCI hospitals in the AIR uptake area; only two had a helicopter platform at the hospital. At the other hospitals, the patient was taken by ground to a rendezvous site nearby.
STATISTICS
Continuous data are reported as median with 5-95% percentiles and we compared groups using the Mann-Whitney test. Categorical data were presented as numbers and percentages, and groups were compared using χ2 test, or Fisher’s exact test where appropriate.
We considered a 30-minute difference in time from ECG to arrival in the CCL to be clinically relevant. We assumed the standard deviation to be 18 minutes and anticipated 350 patients would be enrolled in the study. With a significance level of 0.05, we calculated the power to be more than 95%. P-values below 0.05 were considered significant.
ETHICS
Prior to data collection and analyses we received approval from the Danish Data Protection Agency (j. nr: 2009-41-4122) and the National Board of Health (j. nr: 7-604-04-2/128/HKR). This study did not require approval from the ethics committee according to Danish law, nor did it require informed patient consent.
Results
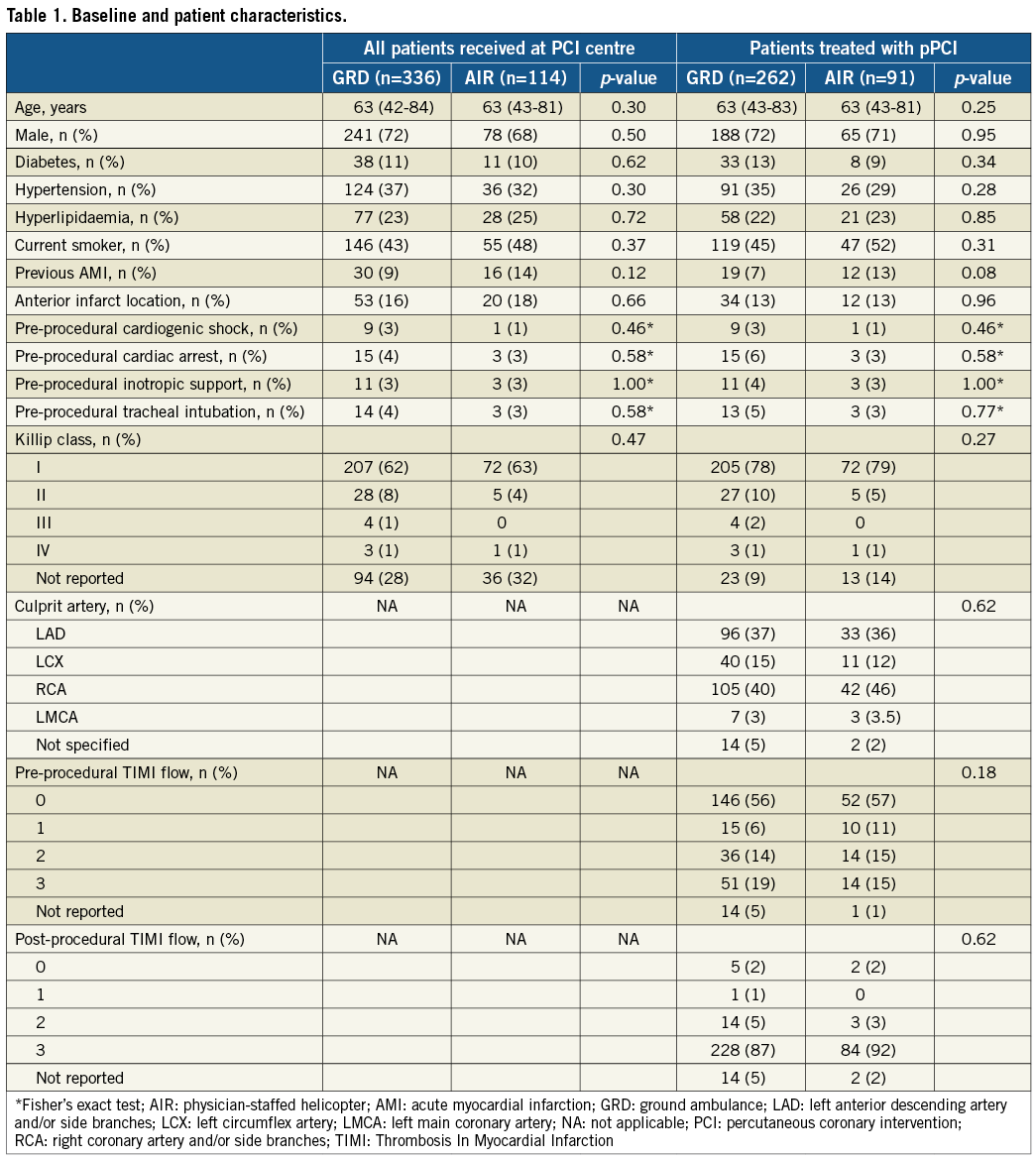
We included 450 patients, 114 transported by AIR and 336 transported by GRD (Figure 2). There were no significant differences in baseline or procedural characteristics between the groups (Table 1). Also, the proportion of patients undergoing acute pPCI was similar: 80% (91/114) vs. 78% (262/336) (p=0.68) for AIR and GRD, respectively.
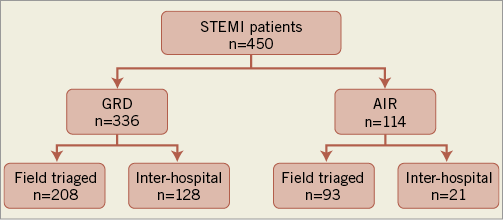
Figure 2. Transport mode and referral site for included STEMI patients. AIR: physician-staffed helicopter; GRD: ground transport; STEMI: ST-elevation myocardial infarction
Time from ECG to CCL arrival was significantly lower in the AIR group, with a median of 84 minutes (60-160) vs.104 minutes (63-225) in the GRD group (p<0.01), despite a significantly longer transport distance in the AIR group (97 [64-162] vs. 94 [65-172] km; p<0.01) (Table 2). Inter-hospital referral was less frequent in the AIR group with 18% (21/114) vs. 38% (128/336) in the GRD group (p<0.01). For the subgroup of patients who were directly referred (field triaged) to the PCI centre from an out-of-hospital location, the time interval from ECG to CCL was 83 (56-145) minutes for patients transported by AIR vs. 97 (60-169) minutes in the GRD group (p<0.01). There were no significant differences in distance to PCI centre in this subgroup. AIR transport was faster than GRD for field triaged patients with a transport distance to PCI centre exceeding 70-90 kilometres (Figure 3). For inter-hospital transport, the advantage of AIR transport seemed even more pronounced. No significant difference in inter-hospital transport distance was observed (Table 2).
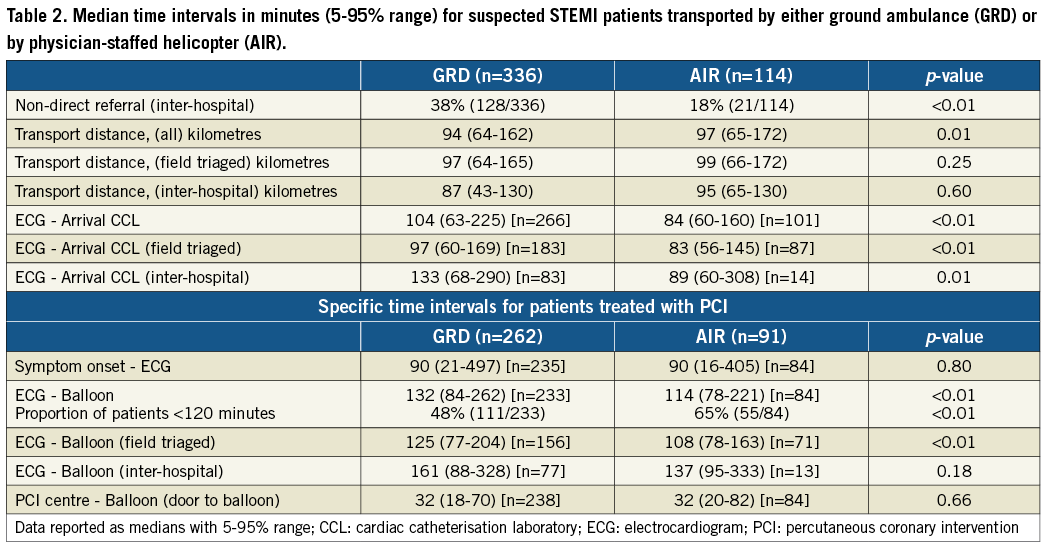
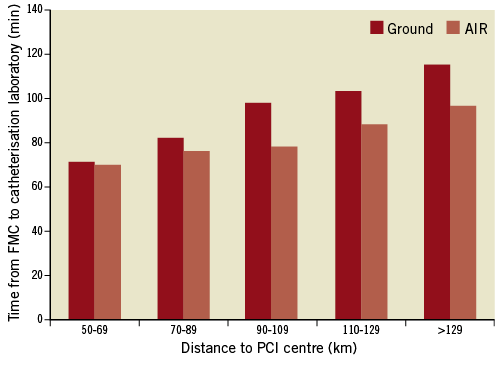
Figure 3. Relationship between distance (km=kilometre) to percutaneous coronary intervention (PCI) centre (X-axis) and time from electrocardiogram (ECG) to cardiac catheterisation laboratory (Y-axis) for field triaged patients transported by either ground ambulance or AIR (physician-staffed helicopter).
We did not record any difference in median door-to-balloon time, which was 32 minutes for both groups (Table 2).
The time from ECG to CCL for GRD patients in the first four months of the study period, where the AIR was not implemented, was 99 (63-176) minutes. This was not significantly different from the GRD time during the 12 months following implementation (105 [63-263] minutes) (p=0.27). During evening and night-time (between 8 pm and 8 am), where AIR transport was not available, the GRD transportation time was 102 (60-260) minutes. During the day (from 8 am to 8 pm) the time was 105 (65-223) minutes (p=0.41). The median time from ECG to dispatch of the AIR transport was 17 minutes. No significant differences were found in either 30-day (2.6% [3/114] vs. 6.3% [21/336], p=0.14) or one-year mortality (8.0% [9/113] vs. 9.8% [33/336], p=0.56), for patients transported by AIR and GRD, respectively. The 30-day mortality for patients who had PCI was 2.2% (2/91) for AIR and 6.9% (18/262) for GRD patients (p=0.10). Mortality at one year was 6.7% (6/90) vs. 9.9% (26/262) (p=0.35). One patient in the AIR group was lost to follow-up.
Discussion
The key result in this study was that time from ECG STEMI diagnosis to arrival at the cardiac catheterisation laboratory was significantly reduced for patients transported by a physician-staffed helicopter compared to conventional ground ambulance.
Patients enrolled in this study all came from the same region, and this population-based design provides the results with high external validity and illustrates the actual “real life” impact of implementing a physician-staffed helicopter as a supplement to the existing STEMI network. We decided to include all STEMI patients instead of only PCI patients, as the primary endpoint was an analysis of transportation mode, and therefore relevant for all those transported with the “intention to treat” (undergo PCI). The primary outcome measure determination was based on printed ECG times and catheterisation laboratory time registration, which minimised the potential patient recall and EMS measurement bias to which other reported time endpoints, such as “treatment delay” or “system delay”, can be vulnerable (Figure 4).
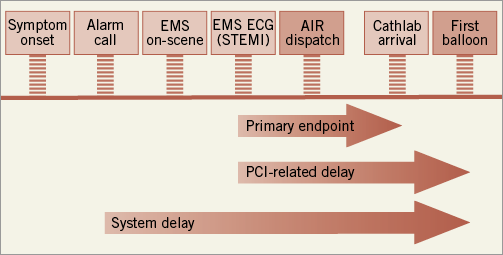
Figure 4. Time intervals in managing pre-hospital triaged STEMI patients. EMS: emergency medical services; ECG: electrocardiogram; STEMI: ST-elevation myocardial infarction; Cathlab: catheterisation laboratory; PCI: percutaneous coronary intervention
Being a non-randomised observational trial, this study has an inherent risk of selection bias. Due to the “daylight only” AIR group and different observation periods between groups, potential diurnal and seasonal selection were present. At present, however, we have not found data to support this assumption.
Few studies have assessed the impact of transport mode on field to PCI centre time. Balerdi et al gathered a small case series on air transported patients with an estimated driving distance >30 minutes, and found a physician-manned helicopter to be faster compared to a virtual estimated ground transport time12. A controlled Japanese study, which included daylight STEMI patients within a 50-kilometre driving radius from the PCI centre, found similar transport times, but 30-minute shorter “dispatch to catheterisation laboratory times”, for patients transported by helicopter13. Despite limitations related to the study design, these results are consistent with our findings, even though they did not quantify the impact of air transport over longer distances.
Several regional STEMI networks in the USA have published protocols in which air transport plays a central role in inter-hospital transfers to PCI centres6. However, one retrospective study of inter-facility helicopter transfers reported difficulties in achieving the goal set in reperfusion guidelines, and it was concluded that inter-hospital helicopter transfer after diagnosis is a source of delay. The authors called for studies similar to ours, where helicopter transport is requested by ground EMS on scene by the use of out-of-hospital ECGs7.
Despite significant overall longer transport distances, we found that the AIR was faster than GRD. According to the dispatch protocol for out-of-hospital patients (field triaged), the AIR was launched after approval from the PCI centre. The time from ECG indicating STEMI to AIR launch was 17 minutes (median), indicating that there was a delay in the communication between GRD on scene and the triaging cardiologist at the PCI centre. A dispatch protocol where the GRD or a physician on scene, based on the pre-printed ECG diagnosis, requests air transport before approval from the PCI centre, could potentially further reduce PCI-related delay for AIR patients. Although GRD and AIR were dispatched simultaneously in our study, when transferring patients from other hospitals there might be delays due to ground transport from the emergency department to the helicopter landing site and loading onto the helicopter. This delay could be resolved by having hospital helicopter platforms.
Surprisingly, we observed that the median time from ECG to PCI centre for field triaged GRD patients was 97 minutes, even though the median distance was only 97 kilometres. This is a considerable delay for a relatively short distance and, since door-to-balloon is often close to 30 minutes, it seems difficult to achieve an acceptable PCI-related delay of 120 minutes. This could be due to triage delay (long decision time at the PCI centre) or because transport with STEMI patients is not just taking the patient from one place to another. A delay may be caused by “driving in the wrong direction” for picking up a transportation team, or having a rendezvous with a (physician- or nurse-manned) mobile emergency care unit when there is a need for help with diagnostics, treatment, transportation or triage. A higher proportion of patients in the GRD group underwent transfer from other hospitals, which might have caused prolonged PCI-related delay compared to direct triage from the field14. However, the subgroup analyses revealed that AIR is faster regardless of referral site.
The goal for system performance is often to assess the proportion of patients fulfilling the international recommendations. We found that two thirds of all of the AIR patients had a PCI-related delay shorter than the one accepted in the ESC guidelines. This was a significantly higher proportion than in the GRD group, where the guidelines were only adhered to in half of the cases. Nevertheless, there was still a significant proportion of patients in both groups in whom the guidelines were not met. Future studies need to address actions that could improve this situation15. We found no significant difference in short- or long-term mortality, but the study was not powered to detect a relevant 30-day mortality difference, as the 3% (AIR) vs. 6% (GRD) observed in the presented data. Cardiogenic shock prior to the procedure tended to be more common in the GRD group but a larger-scale study is needed to clarify potential differences. Accordingly, it is difficult to quantify the clinically relevant benefit from the observed time gain, but a study by De Luca et al16 concluded that the mortality benefit by performing PCI vs. fibrinolysis is reduced for every 10 minutes. Furthermore, Danish registry studies have shown that a prolonged “system delay” (time from EMS dispatch to balloon) is associated with higher long-term mortality, readmission rate, and development of heart failure17,18. These studies indicate that the AIR group would benefit from shorter reperfusion delay, in terms of reduced mortality and morbidity, but further studies are warranted to assess these important issues. Helicopter transport is expensive, but this study does not address whether the benefits outweigh the extra costs.
The helicopter was staffed by an experienced anaesthesiologist with competencies that Danish EMS providers do not have. These include advanced airway management, external cardiac pacing, use of anti-arrhythmogenic drugs and large dose opioids. However, this study was not designed to estimate the effect of this higher level of medical competence, thus information on pre-hospital medical procedures and adherence to standard operational procedures was not systematically gathered. Moreover, we did not include patients who had non-STEMI or resuscitated cardiac arrest patients. They may be transported by AIR to the PCI centre, with the purpose of having an acute cardiac catheterisation. This population might also benefit from early assessment by a trained physician and faster transport to definitive care provided by AIR19.
It is uncertain to what extent the favourable results for the daylight-based AIR transport system in this study can be applied to night operations. Due to flight regulations in Denmark, it is not permitted to land outside designated landing/rendezvous sites during the hours of darkness, resulting in ground transport from the scene to the landing site and an additional loading time.
The results presented in this study are from a PCI centre located in the city centre and congested traffic might have influenced ground transport time. Thus, the results depended on local geography, making generalisation to other systems difficult. On the other hand, the median GRD transport during daylight hours was comparable to night-time where traffic intensity is low.
This study shows benefits of AIR transport. However, it is important to do a case-to-case evaluation comparing the potential clinical benefits to the extra risk for crew and the patient when flying in borderline weather conditions, where the time gained can be offset by even minor delays or deficits in logistics. Consistently, we observed cases where the inability to provide air transport was related to technical problems, crew problems, low visibility and other specific issues regarding the weather.
Despite these limitations, we believe that this study shows that air transport in the described setting is superior to ground transport, even in a relatively confined, flat geographical area, and this information could be valuable to decision and policy makers.
In conclusion, transport of STEMI patients by a physician-staffed helicopter reduced time from ECG to arrival at the cardiac catheterisation laboratory compared to conventional transport by ground ambulance.
Funding
The work was supported by grants from the TrygFoundation (Copenhagen, Denmark).
Conflict of interest statement
J. Steinmetz received consultancy fees from the Medicines Company (Euromax steering committee); P. Clemmensen received payment for speakers’ bureaus from Eli Lilly, Daiichi Sankyo, AstraZeneca, honoraria from Philips, Medtronic, Pfizer, Boehringer Ingelheim, BMS, and has consulted for Medtronic, Eli Lilly, Daiichi Sankyo, AstraZeneca, Bayer, Pfizer. The other authors have no conflicts of interest to declare.