Abstract
Aims: We aimed to investigate why many patients with ST-segment elevation myocardial infarction (STEMI) initially present to non-primary percutaneous coronary intervention (PPCI) equipped hospitals in a region that offers a 24-hour direct access Heart Attack Centre.
Methods and results: A retrospective stratified consecutive case analysis was performed for 180 inter-hospital transfer (IHT) and 201 direct access PPCI patients. IHT and direct patients had similar age (61±1.8 years vs. 62±1.9 years, p=0.42), gender (76% vs. 78% male, p=0.64), and cardiovascular risk profile (hypertension 53% vs. 46%, p=0.18; hypercholesterolaemia 32% vs. 25%, p=0.22; and smoking 38% vs. 35%, p=0.56), though there were more diabetic patients in the IHT group (15% vs. 8%, p<0.05). The IHT group had longer symptom-call times 104 mins (42 mins-195 mins) vs. 46 mins (19 mins-114 mins), p<0.0001), lower ECG ST-elevation scores (3.0 mm [1.0-6.0] vs. 5.0 mm [3.0-9.0], p<0.0001), and more protocol negative ECGs at presentation (31.6% vs. 9.4%, p<0.0001). Peak CK was similar for the two groups (628 IU/L [191-1,144] vs. 603 IU/L [280-1,238], p=0.61), as was in-hospital (1.7% vs. 1.5%, p=0.89) and 30-day mortality (2.8% vs. 2.0%, p=0.61).
Conclusions: This study suggests that reperfusion delays in PPCI due to IHT are not always simply “system failures”. IHT patients appear to be a different patient cohort in which symptoms and early ECG changes may be less clear. In many cases, initial triage to a non-PPCI centre may be justifiable due to diagnostic uncertainty, and guideline time metrics should be amended appropriately.
Introduction
Primary percutaneous coronary intervention (PPCI) is the preferred strategy for revascularisation in ST-segment elevation myocardial infarction (STEMI) and is recommended by international guidelines (AHA/ESC)1-3. A pharmacoinvasive strategy with initial thrombolysis has a role in health jurisdictions with longer transfer distances, when there is an expectation that target PPCI reperfusion times cannot be met4-6. In our healthcare system, PPCI is delivered by a network of Heart Attack Centres designed to provide 24-hour rapid access PPCI within defined catchment areas. The heart attack team work at their best from a logistic standpoint when patients call for help: the paramedic crew arrives quickly, makes a rapid diagnosis in the field, goes directly to the cardiac catheter laboratory, and the PPCI procedure is performed promptly.
Unfortunately, a significant number of STEMI patients do not present in this manner. These patients fall into two main categories: those who self-present to their local emergency department with either an immediate or subsequent diagnosis of STEMI, and those whom the paramedic crew do not identify as having a clinically overt STEMI at presentation. In either scenario, patients can end up at a hospital that is not equipped to perform PPCI and require immediate inter-hospital transfer (IHT) to the regional Heart Attack Centre.
This scenario has been the subject of a number of randomised trials, which overall support IHT for PPCI over local thrombolysis, even with the attendant delays7. These cases are a logistical challenge and often breach guidelines for reperfusion delays. Following concerns in audit and governance meetings locally and regionally about reperfusion time guideline breaches for inter-hospital transfer PPCI patients, a formal service evaluation of such patients was undertaken. We aimed to test the hypothesis that less clear-cut symptoms and ST-segment elevation on presenting ECGs may explain why many IHT cases occur in networks where direct access PPCI is available.
Methods
STUDY DESIGN
The study was performed in the setting of a regional 24/7 PPCI service using a “hub and spoke” model covering a combined suburban/metropolitan region close to London in the United Kingdom, as previously described8. All patients were brought to the Heart Attack Centre by ambulance. A retrospective analysis of clinical and detailed ECG characteristics was performed on 381 stratified consecutive patients (180 IHT, 201 direct) undergoing PPCI. Patients transferred for “rescue PCI” after unsuccessful local thrombolysis were not included in this study.
HEART ATTACK CENTRE AND NETWORK
The ambulance services have an emergency response target of eight minutes from the call for help to arrival on scene. The ambulance crew paramedical staff are trained and empowered to make a diagnosis of STEMI autonomously, characterised by chest pain <12 hours and ST-elevation ≥1 mm in two contiguous leads on the 12-lead ECG or left bundle branch block believed new, and to follow a defined protocol taking the patient directly to the PPCI centre. Paramedics are registered with the UK Health Care Professions Council9, and have undergone a specific PPCI training programme, including logistical training and the recording of a 12-lead ECG, identification of STEMI, and scenarios mimicking STEMI such as pacing and pericarditis.
For direct admission PPCI, the maximum distance from the patient pick-up point to the PPCI centre is 24 miles (38.3 km). ECGs are not telemetered to the PPCI centre and the cases are not discussed with a physician or other staff. The ambulance control centre alerts the PPCI centre advising that the patient is en route and giving an estimated arrival time.
IHT patients are referred by telephone from the emergency department of the local non-PPCI hospital to the Heart Attack Centre. The criteria for referral for PPCI are the same as for the direct admission pre-hospital protocol. Ambulance transfer is facilitated by a dedicated “critical care” transfer protocol.
DATA COLLECTION
Data were collected from a dedicated in-house database in accordance with the Myocardial Ischaemia National Audit Project (MINAP)10 and British Cardiac Intervention Society (BCIS)11 requirements for all UK PPCI centres. Baseline clinical characteristics, cardiovascular risk factors, reperfusion times, ECG ST-elevation score, ECG “protocol positive”, peak CK, in-hospital and 30-day mortality were recorded for all patients.
Reperfusion times were defined as: “symptom”=time of symptoms onset; “call”=time of patient call to the emergency services; “balloon”=time first device deployed after the coronary guidewire (usually a thrombus aspiration catheter).
ECG ANALYSIS
ECG ST-elevation scores were calculated using the ECG driving initial management, i.e., the first available ECG. Standard 12-lead ECGs were used with a paper speed of 25 mm/s and at amplification of 10 mm/mV. The isoelectric line was defined as the preceding T-P segment. The extent of ST-elevation was measured 20 ms after the J-point in every lead. ST-elevation score was manually calculated as the sum of ST-segment elevation in all leads using previously validated algorithms as the sum of elevation in V1-V6, I, aVL for anterior infarction, and as the sum of elevation in leads II, III, aVF, V5 and V6 for non-anterior infarction12. ECGs were also categorised as “protocol positive” or “protocol negative” for STEMI according to our regional primary angioplasty protocols. ECGs were analysed blinded and independently of knowledge of the mode of transfer by AM and JT.
STATISTICAL ANALYSIS
Qualitative data are presented as percentages and comparisons made using the chi-squared or Fisher’s exact test. Quantitative data are presented as mean (SD) or median (IQR) and comparisons made using the two-sample independent t-test or the Wilcoxon rank sum test. Logistic multivariable regression analysis was performed to determine the relationship between clinical characteristics and ECG infarct territories and likelihood of protocol negative ECG on presentation. A p-value of <0.05 was considered statistically significant. Data were analysed using Stata 12 statistical software (StataCorp LP, College Station, TX, USA).
Results
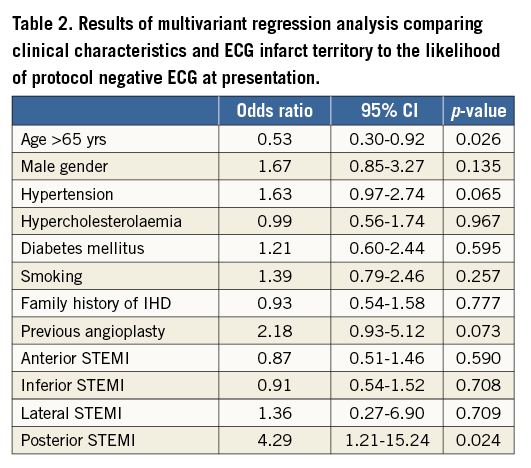
The clinical characteristics of the two groups are summarised in Table 1. IHT and direct access patients had similar age (61±1.8 yrs vs. 62±1.9 yrs, p=0.42), gender (76% vs. 78% male, p=0.64), hypertension (53% vs. 46%, p=0.18), hypercholesterolaemia (32% vs. 25%, p=0.22), significant family history (54% vs. 52%, p=0.57) and smoking (38% vs. 35%, p=0.56). There were, however, significantly more diabetic patients in the IHT than in the direct group (15% vs. 8%, p<0.05). Symptom-call time was significantly longer in the IHT than in the direct group, 104 mins (42 mins-195 mins) vs. 46 mins (19 mins-114 mins), p<0.0001 (Figure 1). Call-balloon time was also longer in the IHT than in the direct group, 105 mins (75 mins-160 mins) vs. 86 mins (73 min-97 mins), p<0.0001 (Figure 2). ECG ST-elevation score was lower for the IHT than for the direct group, 3.0 (1.0-6.0) vs. 5.0 (3.0-9.0), p<0.0001 (Figure 3). The frequency of anterior myocardial infarction was similar for the two groups (IHT 42.5% vs. 48.9%, p=0.22). A histogram of presenting ECG ST-elevation scores indicates a significant left skew for the IHT patients compared with the direct cases (Figure 4). There were more protocol negative ECGs at presentation in the IHT than in the direct group (31.6% vs. 9.4%, p<0.0001). Multivariant regression analysis showed that age >65 yrs (odds ratio 0.53, 95% CI: 0.30-0.92, p<0.05) and posterior STEMI (odds ratio 4.29, 95% CI: 1.21-15.24, p<0.05) were related to the likelihood of protocol negative ECG at presentation; there were no other significant findings (Table 2). In the IHT group 10.6% of patients presented with cardiac arrest vs. 6.5% in the direct group, p=0.15. Peak CK was similar for the two groups, 628 IU/L (191-1,144) vs. 603 IU/L (280-1,238), p=0.61, as was in-hospital (1.7% vs. 1.5%, p=0.89) and 30-day mortality (2.8% vs. 2.0%, p=0.61).
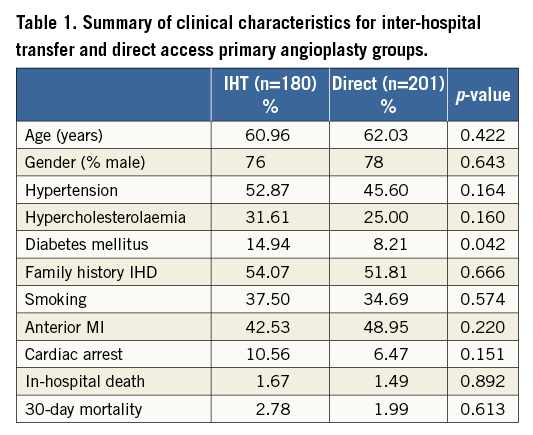
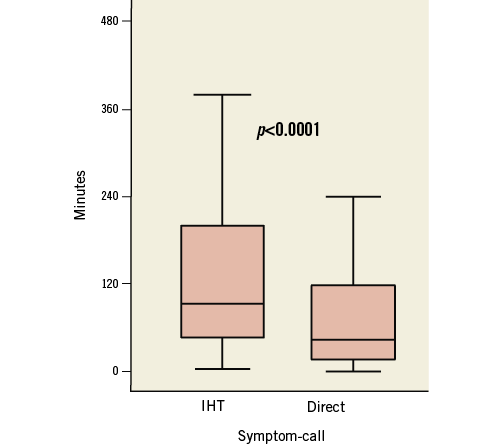
Figure 1. Symptom-call time is significantly increased for inter-hospital transfer vs. direct access primary angioplasty cases.
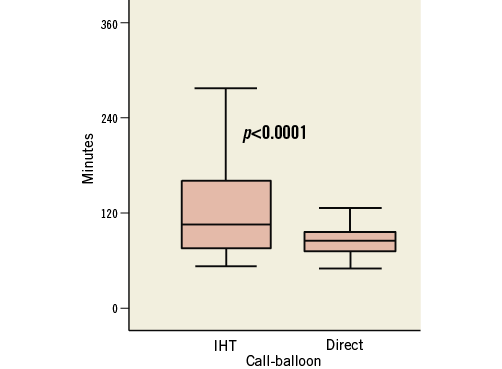
Figure 2. Inter-hospital transfer is associated with significantly longer call-balloon times compared to direct access for primary angioplasty.
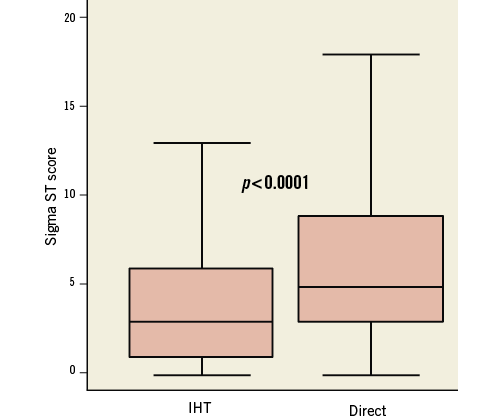
Figure 3. Sigma ST-elevation ECG score at presentation is significantly lower for inter-hospital transfer vs. direct access primary angioplasty cases.
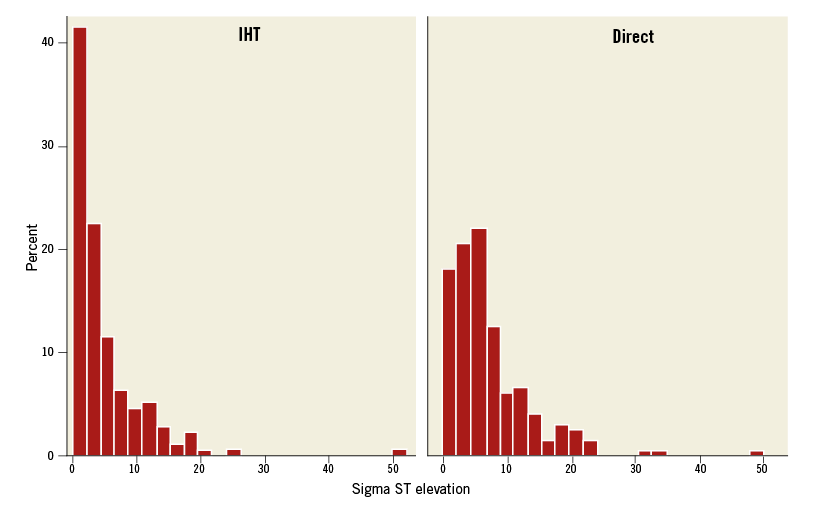
Figure 4. Histogram of Sigma ST-elevation ECG score at presentation showing significant left skew for the inter-hospital transfer patients compared with the direct cases.
Discussion
TARGET PERFORMANCE METRICS FOR PPCI
Overall reperfusion time is correlated with outcome in the treatment of STEMI13. Not surprisingly, associations between both call (or first professional contact)-balloon14 and door-balloon times and mortality have been observed15. From an overall reperfusion time standpoint, however, there needs to be focus on the total symptom-balloon time such that the overall reperfusion time is kept as low as possible. Reducing the symptom-call time is largely a matter for public education and is difficult16, though substantial efforts are ongoing and there is now evidence of patients seeking help at an earlier stage17.
The benefit of PPCI over thrombolysis falls with time18, although the relationship between reperfusion delay and mortality appears to be stronger for thrombolysis than PPCI19. The acceptable delay attributable to PPCI over thrombolysis whereby PPCI remains the preferred therapy is very dependent on the patient risk profile20 and may range from approximately 80 to 120 minutes21. However, when applying these targets to decision making for IHT, the problem is that the patient cohort is very heterogeneous with many cases not representing clinically overt STEMI at the “clock start” time of call/first professional contact-balloon time performance metric.
Current guidelines for time-to-reperfusion metrics rightly take into account the overall system delay rather than simply the call-door or door-balloon in isolation. Such an approach is appropriate as a measure of the efficacy of the service when dealing with STEMI that is clinically overt at presentation (that is to say with a convincing history of pain, and clear ECG changes). However, this approach is less relevant for patients with unclear symptoms or indeed those with initially non-diagnostic ECGs, as observed in nearly one third of the IHT group in this study, where it may be potentially misleading and inappropriate.
THE ROLE OF INTER-HOSPITAL TRANSFER WITHIN A REGIONAL PPCI NETWORK
When IHT occurs in a regional network where 24-hour direct access PPCI is available, one has to ask why the patient was transferred to a non-PPCI hospital in the first place. Some patients may be misdiagnosed by the paramedic crew and inappropriately taken to the wrong hospital. Introduction of ECG telemetry systems that allow involvement of the on-call cardiologist at the receiving Heart Attack Centre in the pre-hospital diagnosis process may reduce such errors. However, this study suggests that for many patients the diagnosis is not clear-cut at presentation. We observed longer symptom-call times and lower ST-elevation ECG scores, with a much higher proportion of protocol negative ECGs at presentation for the IHT group. This may indicate that, for many IHT patients, less severe symptoms and borderline or “protocol-negative” ECGs at presentation could have led to diagnostic uncertainty in the minds both of the patient and of the medical staff causing delay. Interestingly, the proportion of diabetic patients was also higher in the IHT group, and these patients may have presented with atypical or less clinically overt symptoms. In such circumstances, reperfusion delays are not simply systems failure.
Thus, whilst contemporary emphasis in STEMI treatment is rightly focused on speed of reperfusion, in less clear clinical scenarios it can sometimes be appropriate clinical care to assess the situation further with serial ECGs and other investigations. Indeed, the denominator of patients who present with chest pain, epigastric pain or breathlessness who ultimately turn out to have an alternative diagnosis is large and hard to quantify. Certainly many of these patients would not be served well by an emergency transfer to the cardiac catheter laboratory.
WHEN SHOULD THE CLOCK START FOR IHT PATIENTS?
The AHA/ACC recommend that the first professional contact-balloon target reperfusion time be applied to both direct and IHT cases22. It may, however, be inappropriate to judge cases that are clinically overt or high risk at presentation, which appear to get transferred faster23,24, by the same standards as those that are not.
One approach to overcome this problem is to use the time of the “first diagnostic ECG” or the “ECG driving treatment” as the “call” time. This would provide a more accurate and universally applicable assessment, by eliminating the period of diagnostic uncertainty when either the patient’s symptoms or ECG were not sufficient to warrant immediate transfer for PPCI. However, during the evolution of ECG changes, the precise time at which the ECG becomes “protocol positive” may be a matter of individual judgement and hard to define. Furthermore, the first ECG will inevitably be after the call time, making comparison of such a metric with call-balloon times for direct patients difficult. This is less of an issue when using the first professional contact clock start time which should be very close to the first ECG in most cases. Nonetheless, a clock start time at the first diagnostic ECG may be a reasonable compromise.
Study limitations
This is a single-centre series based on a PPCI network using field diagnosis and “open access” referral. The conclusions cannot therefore necessarily be generalised to networks using other referral protocols. Although we postulated that longer symptom-call times in the IHT group were due to less clear-cut initial symptoms, we did not specifically collect data regarding the nature of initial symptoms, as this is subjective and difficult to compare. Further studies would be needed to prove this relationship. In addition, the study does not take account of the very large and difficult to measure denominator of patients with borderline ECG changes who are not referred to the PPCI programme.
Conclusions
IHT for PPCI increases time to reperfusion for patients with STEMI who initially present to a non-PPCI hospital. However, in a real-life series this group of patients is not the same as the direct access PPCI cohort. As a group, they have longer symptom-call times and less clear-cut, often normal (or near normal) ECGs at presentation, which often would not fulfil criteria for thrombolysis, making a binary decision between immediate local thrombolysis and transfer for emergency angiography (±PPCI) extremely difficult, given the limited evidence from randomised trials and current guidelines. Furthermore, for IHT patients presenting with a non-diagnostic ECG, the time at which the ECG becomes “diagnostic” may be difficult to define during a “grey area” of diagnostic uncertainty.
As a result, the application of simple call-balloon metrics across the board for this complex group may not be valid, and our findings further support the recent conclusions of Miedema et al23. This study reinforces the concept that, in patients with a likely significant delay for IHT PPCI, an individually tailored approach is best both for clinical care, and guidelines. This of course must not detract from the need for rapid delivery of reperfusion when appropriate. However, if the same call or first professional contact-balloon target is going to be applied to IHT as direct PPCI patients, it needs to be restricted to those that are clinically overt at presentation, or corrected for the time of the first “diagnostic” ECG, both of which are a challenge. Guideline time metrics may need to be amended appropriately for such patients.
| Impact on daily practice In daily clinical practice, many patients with a diagnosis of STEMI undergo inter-hospital transfer for PPCI, ostensibly causing delays compared to those triaged directly to the cardiac catheterisation laboratory. Often the receiving cardiologist will refer to the time of symptom onset when judging the benefit of transfer for PPCI over local treatment, a general approach supported by current guidelines. However, this study shows that in certain patient populations the manifestation of diagnostic clinical symptoms and ST-segment elevation can be slow to evolve, necessitating an appropriate period of evaluation while the diagnosis is uncertain. In this scenario, a reasonable compromise for guideline metrics, systems evaluation and indeed clinical decision-making pathways may be to consider using the first diagnostic ECG as the clock start time. |
Acknowledgements
This project was supported by the NIHR Cardiovascular Biomedical Research Unit at the Royal Brompton and Harefield NHS Foundation Trust and Imperial College London.
Conflict of interest statement
The authors have no conflicts of interest to declare.