Abstract
Aims: This study sought to evaluate the impact of a direct transfer strategy on treatment times and prognosis of patients with ST-segment elevation acute myocardial infarction (STEMI) undergoing primary percutaneous intervention (PPCI).
Methods and results: We conducted a cohort study of 1,194 patients who underwent PPCI in our centre between May 2005 and December 2008. We studied the role of direct transfer on time to treatment and door-to-balloon delays and its effect on 30-day mortality adjusted by risk profile on admission. During this period, 255 patients (21%) experienced direct transfer (DT) from the field to the catheterisation laboratory. Patients referred directly for PPCI experienced lower median door-to-balloon delay (102 minutes vs. 125 minutes, p<0.0001) and lower time to treatment (median 189 minutes vs. 259 minutes, p<0.0001) when compared with those referred from emergency departments (ED). These differences were consistent, with respect to door-to-balloon delay and time to treatment interval, in patients from our catchment area: median 88 vs. 98 minutes, (p=0.003) and 174 vs. 219 minutes (p<0.0001) respectively, and from long-distance transfer: 110 vs. 169 minutes (p<0.0001) and 197 minutes vs. 342 minutes (p<0.0001) respectively. Patients in the DT group experienced lower 30-day mortality than patients transferred from the ED (2.7% vs. 6.8%, p=0.017). In a multivariable analysis, DT strategy was independently associated with better short-term prognosis (OR 0.33, CI95% 0.12 – 0.92).
Conclusions: Direct transfer reduces time delays and improves prognosis of patients with STEMI undergoing PPCI.
Introduction
Primary percutaneous coronary intervention (PPCI) has emerged as the preferred reperfusion strategy for patients with ST-elevation myocardial infarction (STEMI) at institutions with both appropriate interventional facilities and experience. PCI decreases rates of mortality, reinfarction, stroke and haemorrhagic complications compared with thrombolytic therapy, as was demonstrated in recent pooled analyses1,2. Nonetheless, its widespread use is restricted by a lack of properly equipped hospitals and experienced staff. To overcome this drawback, strategies to transfer patients with STEMI to interventional hospitals have been developed. This protocol is safe, feasible and has yielded better results than on-site thrombolysis3-7.
However, delays related to the transfer have emerged as the main concern of this strategy. Door-to-balloon delay correlates with adverse outcomes in patients with STEMI referred for PPCI8,9. Two studies and one meta-analysis have also shown that a shorter time-to-treatment interval is also correlated with a better prognosis10-13. Current guidelines stress that door-to-balloon delay must be inferior to 90 minutes, but very few centres meet this target in everyday practice14,15 and recently, several strategies have been proposed to reduce these time intervals16. Moreover, it has been demonstrated that as the door-to-balloon/door-to-needle difference increases, the benefit of PPCI is reduced when compared with thrombolytic therapy17,18. Thus, strategies to reduce these time intervals emerge as a crucial topic.
The objective of this study is to investigate whether direct transfer to the catheterisation laboratory from the field by the emergency ambulance service in a region with a heterogeneously distributed population is associated with lower symptom onset-reperfusion and door-to-balloon delays when compared with referral from hospital emergency departments (ED) and the impact of this strategy on short-term mortality.
Methods
PPCI program design. The PROGALIAM
Galicia is a mainly rural region (although with some moderate-sized cities) located in the Northwest of Spain. Characteristic of Galicia is a highly scattered population, with nearly 32,000 small villages and 315 health departments. The CHUAC is the interventional hospital in the north of Galicia, an area of about one million people (Figure 1).
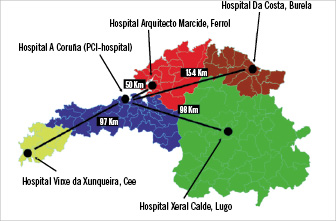
Figure 1. PCI-hospital and associated non-PCI hospitals included in the program.
Our catheterisation laboratory provides round-the-clock service for PPCI for patients from our catchment area (short transfer distances) and for patients from four other non-PCI hospitals (long transfer distances). Since 2005 the Galician Health Service (SERGAS) has developed an active program to offer PPCI to the majority of the population. According to this program, the PROGALIAM, all patients directly admitted to hospitals with interventional facilities are offered PPCI as the preferred reperfusion strategy and patients arriving to hospitals without on-site PPCI are rapidly transferred to interventional hospitals to undergo the same procedure19. Transport of the patients is mostly carried out by the Emergency Assistance Ambulances Service-061 (EAS-061), although a significant proportion of patients reached the hospital by their own means. EAS-061 has two types of ambulances: transport ambulances managed by paramedics with the capability to mobilise patients and provide basic life support, and emergency care ambulances, managed by medical staff with training in intensive care medicine and capable of delivering advanced life support. Ambulances can collect patients directly from the secondary hospitals or from primary care points. Emergency care ambulances have the capability to activate the interventional team directly, as long as a trained medical staff can provide an accurate interpretation to the 12-lead ECG. This activation is strongly recommended when patients’ first contact is EAS-061, directly or through the primary care physician.
In non-PCI hospitals, patients suitable for PPCI according to the recommendations established in the current guidelines14,20 are transferred to the interventional hospital by the EAS-061. The transfer is strongly recommended for patients with a delay from the beginning of symptoms > 2 hours, patients presenting in the first two hours who can be safely transferred to the catheterisation laboratory in <110 minutes and patients with symptoms and signs of heart failure, cardiogenic shock or contraindications to thrombolytic therapy19. Our hospital accepts transfers from four non-PCI hospitals located between 50 and 154 km from the hub centre (Figure 1). The protocol was designed and performed in accordance with the regulations of the institutional ethical committee. All patients gave written informed consent.
Patient population
All patients presenting typical chest pain lasting > 30 minutes with ST-segment elevation ≥1 mm in ≥2 contiguous leads (or reciprocal ST depression ≥1 mm in leads V1 or V2), or left bundle branch block in the first 12 hours after the beginning of symptoms were eligible for PPCI. Information with regard to cardiovascular risk factors, previous medical history or use of cardiovascular drugs was recorded from the patient directly or from the medical records if necessary. Patients with symptoms lasting >12 hours, with absence of vital signs or with an unconfirmed diagnosis of STEMI were excluded from the program. Patients transferred for rescue PCI or those who were not intended for angioplasty were excluded from the analysis. There was no restriction policy based on age, sex, clinical status or co-morbidities. However, whereas in the PCI-hospital all patients who met the aforementioned criteria underwent PPCI, in the non-PCI hospitals the decision to transfer patients or initiate fibrinolytic treatment is left to the discretion of the medical staff taking into account the profile of the patient and the expected delays.
Treatment protocol
Patients received at least 250 mg of aspirin at the moment of diagnosis. An intravenous IIb/IIIa inhibitor (Abciximab, loading dose of 0.25 mg/kg followed by a continuous infusion of 0.125 µg/Kg/min for 12 hours) administered in the emergency department or during transport was strongly recommended. A loading dose of 300 mg of clopidogrel was administered in the emergency department or in the EAS-061. After the procedure, a maintenance dose of 75 mg/day of clopidogrel was recommended for one month if a bare metal stent was implanted and for 12 months if it was a drug-eluting stent. Other treatments were at the discretion of the attending physician.
Endpoint definitions and follow-up
Time-to-contact was defined as the time between symptoms onset and first contact with the medical system. Time-to-treatment was defined as the time that had elapsed between symptoms onset and mechanical reperfusion. Contact-to-balloon delay was the time between the first medical contact (ED of PCI or non-PCI hospitals or EAS-061 ambulances in case of DT) and the restoration of coronary blood flow and this interval was considered as the door-to-balloon delay. Time from contact to activation was defined as the interval between the first medical contact and the call to the interventional team, and PCI-hospital to balloon delay was defined as the time elapsed between the arrival at the interventional hospital and the first balloon inflation.
Thirty-day mortality was defined as mortality by any cause within this period and this information was obtained from medical records or telephone call if required.
Statistical analysis
Results are presented as mean ±1 standard deviation (S.D.) for continuous normally-distributed variables, as median (interquartile range) for continuous non-normally-distributed data, and as percentages for categorical data. Analysis of normality was performed with the Kolmogorov–Smirnov and Shapiro-Wilk test. Categorical data and proportions were compared using χ2-test or Fisher’s exact test as required. Comparisons of continuous variables were analysed using unpaired t-test and the Mann–Whitney U-test as appropriate. Logistic regression analysis adjusted by age, sex, baseline cardiovascular risk factors, previous history of myocardial infarction or unstable angina, abciximab use, cardiogenic shock on admission, anterior wall myocardial infarction, systolic blood pressure and time from symptom onset to medical contact was used to determine variables independently associated with short-term mortality. P values less than 0.05 were considered significant. All analyses were performed with SPSS 15.0 statistical package for Windows (SPSS 15.0, Chicago, IL, USA).
Results
Study population
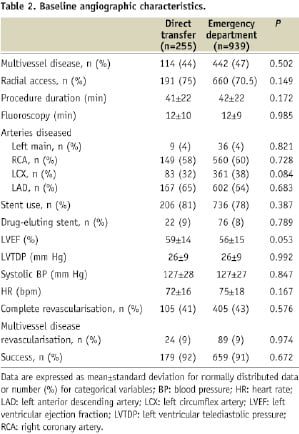
Between May 2005 and December 2008, 1,194 consecutive STEMI patients were treated with PPCI in our centre. First medical contact was established with the ED of the PCI-hospital in 596 patients (50%), with the ED of non-PCI hospitals in 343 patients (29%) and with EAS-061 in 255 patients (21%). Baseline clinical characteristics of the population and angiographic findings are summarised in Tables 1 and 2.
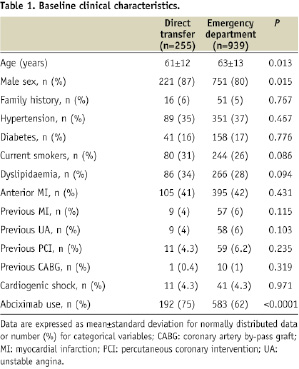
During the period of time analysed, 69 patients (7.1%) in the ED group and 12 patients (4.7%) in the DT group presented without significant angiographic stenoses. These patients represent a false positive activation of the program, but the overall percentage was low in both groups and without significant differences (p=0.200). These patients were excluded from the final analysis. Only two patients transferred to PPCI by the EAS-061 died during the transport, both in the ED group.
Time intervals in PPCI
Time intervals in the whole series are displayed in Table 3.
As we can observe, all time intervals were significantly reduced in the group of DT.
There were no significant differences between the two groups in the number of patients achieving a door-to-balloon delay lower than 90 minutes (31.5% vs. 26.8%, P=0.145). Nonetheless, when groups were compared with regard to a door-to-balloon delay lower than 120 minutes, there was a higher proportion of patients achieving this goal in the DT group (66% vs. 46%, P<0.0001).
Interventional hospital vs. non-PCI hospitals
We also performed a subgroup analysis of the time intervals according to the hospital type, PCI or non-PCI. In both groups DT resulted in a consistent significant reduction in the time intervals.
In the PCI-hospital area, 113 patients (16%) experienced DT. These patients had lower door-to-balloon delay and a shorter time–to-treatment interval (Figures 2 and 3).
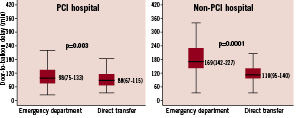
Figure 2. Box plot showing the difference between DT and ED groups with regard to the door-to-balloon delay depending on the patient origin. Time intervals are expressed in median and interquartile range.
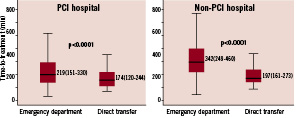
Figure 3. Box plot showing the difference between DT and ED groups with regard to the time to treatment depending on the patient origin. Time intervals are expressed in median and interquartile range.
The percentage of patients achieving a door-to-balloon delay < 90 minutes was 41% in the ED group and 53% in the DT (P=0.028) and that of patients experiencing a door-to-balloon delay < 120 minutes was 66% in the ED and 80% in the DT (P=0.009).
In the catchment area of the group of non-PCI hospitals, 142 patients (29.3%) were transported directly from the field. The door-to-balloon and the overall ischaemic time were also shorter in the DT group (Figures 2 and 3). However, no differences were observed with regard to the PCI hospital-balloon time (31 minutes [24-40] vs. 33 minutes [26-40], P=0.139). The percentage of patients achieving a door-to-balloon delay <90 minutes was 1.5% in the ED group and 15% in the DT (P<0.0001) and that of patients experiencing a door-to-balloon delay <120 minutes was 10% in the ED and 57% in the DT (P<0.0001).
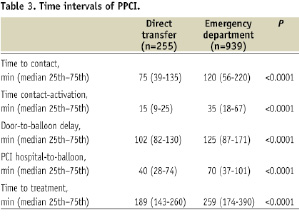
Clinical outcomes
Overall 30-day mortality was 5.9% for the entire cohort. Thirty-day mortality was 2.7% for the DT group and 6.8% for the ED (p=0.017) (Figure 4).
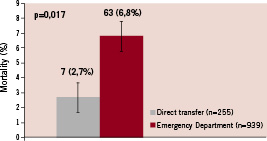
Figure 4. Bar chart of 30-day mortality. Direct transfer group experienced significantly lower mortality than patients from ED.
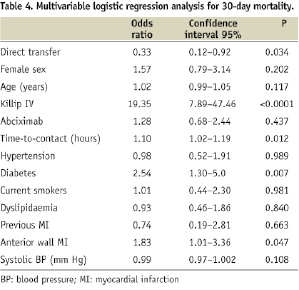
A multivariable logistic regression analysis identified the DT strategy as independently associated with a better short-term prognosis (Odds ratio [OR] 0.33, CI 95% 0.12 – 0.92, p=0.034). Results of multivariable analysis are displayed in Table 4.
Discussion
Previous studies have demonstrated that patients with STEMI directly transferred to PPCI bypassing ED of PCI and non-PCI hospitals experience lower door-to-balloon delay, shorter time-to-treatment and a trend to lower mortality21-27. However, these results have not been tested in a regional angioplasty network characterised by a high degree of dispersion in the population. We report the first study conducted in a region with such characteristics. Direct transfer to the catheterisation laboratory by EAS reduces crucial time intervals in patients with STEMI and improves short-term mortality. This large prospective registry confirms the findings of previous smaller studies and expands its benefit to those patients transferred from long distances, in a rural area and with a highly scattered population.
Our 30-day mortality in the overall series (5.9%) was comparable with previously reported registries of angioplasty networks. Manari et al28 observed an in-hospital mortality that ranged from 7.2% to 5.9% depending on the patient subgroup (on-site or transfer PPCI) and Ting and co-workers29, analysing the results from the Mayo Clinic protocol, reported a 30-day mortality from 9.4% to 15.5% (on-site or transfer-PPCI). Information with regard to the effect of DT strategy on mortality is scarce. Le May et al21 reported that the direct referral to PPCI by paramedics was independently associated with a better in-hospital outcome. However, their control group was a retrospective cohort of patients receiving thrombolytic therapy and this result might have influenced the differences in mortality observed between groups. Moreover, patients with cardiogenic shock were excluded from the direct transfer protocol. Ortolani and co-wokers26 found that DT strategy was associated with lower in-hospital mortality only in patients presenting in cardiogenic shock, but they failed to show a significant survival benefit in the overall population (4.8% for DT, 7.3% for ED in PCI-hospital and 7.4% for transfer from non-PCI hospitals, p=0.537). Recently, a meta-analysis was carried out to address the effect of DT on mortality, pooling the results of five studies with 980 patients overall. Authors conclude that there is insufficient evidence to support that this strategy is associated with an improved short-term prognosis (relative risk for in-hospital or 30-day mortality 0.51, CI95% 0.24-1.10)30. Our study, the largest conducted to date, sheds light into this controversial field by demonstrating that patients transported directly from the field have a better 30-day survival. These patients experienced a relative reduction of nearly 70% in this endpoint. We speculate that the reduction in the time delays to accomplish reperfusion and a long-standing contact with the medical system are the responsible for this positive achievement. Although delays in our registry were greater than recommended, our mortality rates were lower than observed with thrombolytic therapy in the large Swedish registry RIKS-HIA31. In this registry, patients treated with lytic therapy experienced a 30-day mortality of 9.5%. And, importantly, 30-day mortality of patients in the DT group was even lower than reported with pre-hospital thrombolysis (7.6% at 30-day in the RIKS-HIA registry), which supports the use of this strategy. However, these figures should be interpreted with caution because direct comparison with previous registries might have serious limitations, taking into account that these are different populations, i.e., Killip IV rates in Swedish registry was higher than reported in our series. Further research is warranted to determine if DT is superior to pre-hospital thrombolysis.
Limitations
This study has several limitations. First, its non-randomised method may have introduced variables affecting time intervals and clinical outcomes. Second, our results may not be applicable to other hospitals without similar resources and trained staff. Thirdly, we do not have a control group with on-site or pre-hospital thrombolysis for assessing possible differences in mortality between this group and the PPCI group.
Conclusions
Direct transfer to the catheterisation laboratory, bypassing the ED of PCI and non-PCI hospitals, shows a significant reduction in the time intervals to accomplish reperfusion and is associated with a better 30-day outcome. This is a safe and feasible strategy to implement in interventional hospitals receiving both short- and long-distance transfers for PPCI.

