Abstract
Aims: To describe the safety of immediate retransfer to community hospitals following primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI).
Methods and results: In a cohort of 246 consecutive patients transferred to a tertiary institution who all underwent primary or rescue PCI, 166 (67%) were immediately retransferred back. The retransfer occurred only if they were haemodynamically stable and had undergone an uncomplicated procedure. In-hospital adverse events were assessed in each referral hospital. Patients had a mean age of 59 years, presented an anterior MI in 39%, and 91% were in Killip class 1. In this cohort, 75% of patients underwent primary PCI and 25% received rescue PCI. A transradial approach was used in 74% of patients. During ambulance transport back to the referral hospital, no adverse events occurred. In-hospital outcomes were favourable, with low death (2.4%), reinfarction (3.6%) and stroke (1.2%) rates. TIMI major bleeding occurred in 1.8% (catheter-related in 0.6%).
Conclusions: In this carefully selected population of STEMI patients, immediate retransfer to the referral hospital following primary or rescue PCI is feasible in more than 2/3 of patients and associated with a low risk of major clinical adverse events.
Introduction
Numerous randomised clinical trials and meta-analyses have demonstrated the benefits of transferring patients from community hospitals to percutaneous coronary intervention (PCI)-capable centres in order to receive mechanical reperfusion in the management of acute myocardial infarction1-5. However, many obstacles remain to achieve a widespread use of primary PCI as an initial strategy in the management of ST-elevation myocardial infarction (STEMI) in patients in outlying regions6. Aside from prohibitive expected transfer delays, bed shortages in coronary care units of PCI hospitals impede further the limited access to primary PCI for patients initially admitted to community hospitals. Pre-admission phone calls to confirm bed availability in the receiving coronary care unit to accept the transfer for primary PCI is clearly against recommendations to meet optimal door-to-balloon times7.
While same day retransfer to referring hospitals have been performed safely in elective PCI8 and in patients with acute coronary syndromes9, no data exist in the literature on the safety of the immediate retransfer following primary PCI for STEMI patients, who are at higher risk of acute adverse events. In this report, we describe the feasibility and safety of a hospital network with immediate retransfer of selected patients following primary or rescue PCI to their referring community hospitals.
Methods
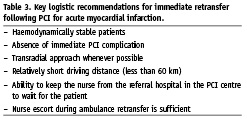
Between April 2004 and March 2005, 246 consecutive patients were transferred from 10 community hospitals to the Centre Hospitalier de l’Université de Montréal (CHUM), a large tertiary hospital in Montreal, Canada. There, they received primary PCI or rescue angioplasty in the setting of an acute STEMI. Patients were identified through the catheterisation laboratory database and the central hospital archiving system. Diagnosis of STEMI and decision to transfer patients to the PCI institution was left to the referring physician. Because of the chronic shortage of coronary care unit beds in the PCI institution and in order to improve access to primary PCI, a decision was taken in early 2004, in agreement with the referral hospitals, to transfer back haemodynamically stable patients who underwent an uncomplicated primary PCI. This decision led to immediate retransfer of 166 patients. The protocol allowed for such a transfer to occur within two hours of the procedure, with the same nurse who accompanied the patient and stayed during the procedure. The final decision as to whether to retransfer was left to the attending interventional cardiologist. Haemodynamic stability was defined as the absence of the need for vasopressor agents or intra-aortic balloon pump support. A procedure was considered uncomplicated if the final Thrombolysis in Myocardial Infarction (TIMI) flow was grade 2 or 3. In the culprit artery, and if haemostasis was achieved at the access site. The transradial approach was favoured whenever possible. Stents were used in suitable lesions and clopidogrel was systematically used before or after stent implantation. The decision to use glycoprotein IIb/IIIa inhibitors was also left to the referring physician and the attending interventional cardiologist. During the same period, 129 consecutive patients were admitted directly from the CHUM emergency room following primary PCI for acute myocardial infarction. The characteristics and outcomes of those patients are reported for purpose of comparison with a transferred population.
Baseline characteristics, treatment strategies, ambulance transport and subsequent in-hospital clinical outcomes were collected through detailed individual chart review performed in each of the 10 referral hospitals included in the network by the principal investigator (AM). In-hospital mortality was considered when death occurred at any time from admission to the primary hospital. PCI was considered successful if final TIMI flow in culprit vessel was reported as normal (grade 3) and if residual stenosis was <20%. Myocardial reinfarction was defined as a > 50% increase in cardiac biomarkers (troponin or CKMB) in the setting of chest discomfort or ischaemic ECG changes. Stroke was considered when any focal or global neurological deficit lasting more than 24 hours was reported. Significant arrhythmia included new onset arrhythmias leading to haemodynamic instability or requiring immediate treatment. We considered that haemodynamic instability occurred during ambulance transport if vasopressor drugs were needed. TIMI major bleeding events10 were also recorded during ambulance transport and full index hospitalisation. The abstraction of this retrospective data was approved by the CHUM and all the referring institution’s Directors of Professional Services as part of a quality of care assessment. Continuous variables are reported as the mean value±SD. Student t test was used for analysis of continuous variables and chi-square test for analysis of discrete variables.
Results
A total of 375 patients underwent primary or rescue PCI in our centre during the study period. Of these, 129 patients presented directly to the CHUM emergency room and were admitted to the coronary care unit; these patients will serve as comparators. Of the initial 246 transferred patients, slightly over two thirds (166 patients or 67.5%) were retransferred back to their referral hospital immediately after the intervention, all accompanied by a nurse. Only three patients, which had been transferred with a physician because of instability prior to PCI, were retransferred with physician accompaniment. Baseline clinical, angiographic and procedural characteristics of retransferred patients (group A=129 patients), those transferred and admitted to the PCI centre (group B=80 patients) and patients who presented directly to PCI centre (group C=129 patients) are shown in Table 1. Patients immediately retransferred after PCI were younger, with an average age of 58.6 years, and mostly male (75%). The myocardial infarction involved the inferior wall in 55% of the patients, and the anterior wall in 39%. The majority (91%) of patients retransferred presented in Killip class 1 infarction; a larger proportion had single vessel disease (60%) than those patients transferred and admitted to the PCI centre. Also, a larger proportion of patients returned to their centres were managed from the transradial approach. Three patients had suffered cardiogenic shock prior to transfer to our centre. Palliative care was selected in two of them, justifying retransfer to the referring hospital. The cardiogenic shock of the third patient resolved following late reperfusion during ambulance transport after initial thrombolysis at the referral hospital. As expected, the proportion of patients in cardiogenic shock was higher in patients admitted in the coronary care unit of the PCI centre. The distance from our institution to the referral hospitals was less than 20 km in 100 patients (60%), 20 to 40 km in 57 patients (34%), 40 to 60 km in three patients (2%) and more than 60 km in six patients (4%).
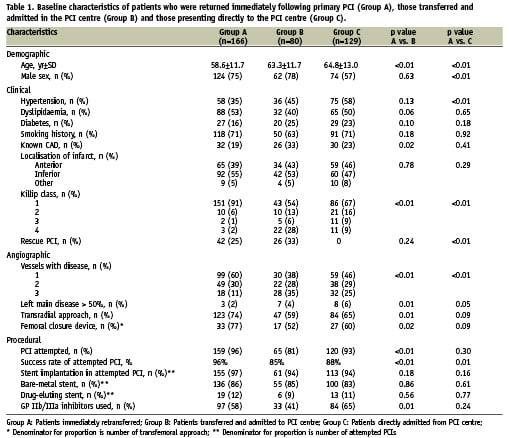
The majority of patients retransferred to their referral hospital (75%) were sent for primary PCI, while the remaining 25% were sent for rescue angioplasty following failed thrombolysis. The success rate of attempted angioplasty was 96%. Stent implantation was performed in most patients (97%). Of the patients who did not receive PCI, two were retransferred to their referral hospital in order to wait for coronary artery bypass graft surgery, and five did not receive any reperfusion strategy for technical reasons. In 74% of these cases, a transradial approach was used. In the others, access was secured through the femoral artery and a closure device was used in 77%. Sheath removal and manual compression was performed prior to retransfer in the others. Clopidogrel was administered in 96% of patients and glycoprotein IIb/IIIa inhibitors in 58% (41% before procedure, 17% during procedure and in one case after procedure). None of the patients who were retransferred received vasopressor support or intra-aortic balloon pump support during the intervention. Median door-to-balloon delays (from presentation in the hospital to first balloon inflation) were 137 minutes for primary PCI patients and 269 minutes for rescue angioplasty patients.
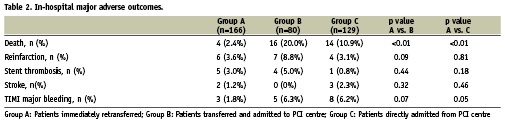
During the ambulance transport from the PCI centre to the referral hospitals, there was no death, significant arrhythmia, haemodynamic instability or TIMI major bleeding. Major in-hospital adverse outcomes are shown in Table 2. In-hospital death occurred in four patients (2.4%); three out of these four deaths were to be expected based on the findings at catheterisation and on clinical grounds. Conservative treatment was advocated after discussion with the referring physician. Reinfarction occurred in six patients (3.6%) and ischaemic stroke was diagnosed in two patients (1.2%). TIMI major bleeding was observed in three patients (1.8%), only one of which was attributable to the PCI procedure. Mean left ventricular ejection fraction at discharge from the referral hospital was 49.6% and median total length of stay (from presentation in the emergency room to final discharge from the referral hospital) was five days. In comparison, patients transferred and admitted to our coronary care unit suffered higher in-hospital adverse events, as would be anticipated from their higher risk profile. The death rate for these patients was 20.0%, reinfarction rate was 8.8%. No strokes occurred. TIMI major bleeding was documented in 6.3% of patients (3.8% related to PCI) and median length of stay was seven days.
Discussion
Immediate retransfer to referral hospitals following successful primary or rescue PCI for STEMI in this carefully selected population was not associated with any adverse event during ambulance transport. Furthermore, largely because of this selection process, patients experienced very low rates of in-hospital major cardiovascular events. Mortality rates were low and death was foreseeable before retransfer in the majority of the cases. Indeed 50% of deaths resulted from severe anoxic encephalopathy following prolonged cardiopulmonary resuscitation before reaching the catheterisation laboratory.
To our knowledge, the present report is the first to suggest the safety of immediate retransfer following emergent angioplasty for STEMI. One article9 reported the safety of immediately retransferring patients following PCI performed for acute coronary syndromes. However, a physician was present during ambulance transport in most cases. Our experience suggests that, with appropriate selection of low risk patients after an uncomplicated procedure, immediate retransfer following primary or rescue PCI for STEMI without physician surveillance during ambulance transport is feasible, and appears to be safe. The preferential use of the transradial approach was likely one of the facilitating factors.
The occurrence of six reinfarctions which represent an in-hospital rate of 3.6% is consistent with previous data in the literature11,12. Of those six events, five were due to definite early stent thrombosis. Although an explanation is available for two cases (early antiplatelet medication withdrawal because of severe gastrointestinal bleeding and thrombosis associated with heparin-induced thrombocytopenia), these numbers are of concern even though no in-hospital mortality was associated with these adverse events. All patients underwent emergent angiography and only one patient could not receive successful revascularisation. Strokes also occurred at a higher rate than anticipated but the absolute number is too small to draw any conclusion.
In Canada and in many others industrialised countries, coronary care unit bed availability in PCI-capable centres is one of the many obstacles that limit access to primary PCI in patients presenting to community hospitals. Using two simple clinical criteria (haemodynamic stability and absence of immediate post-PCI complication), we were able to retransfer two-thirds of patients referred to our institution. Protocols such as the one used in this series are likely to provide better access to the catheterisation laboratory for patients suffering STEMI, especially in the context of limited admission capacity of the PCI centres.
The results observed in our population may only be applicable to carefully selected, low-risk patients for whom the attending interventional cardiologist established the safety of immediate retransfer. Moreover, the experience presented is one of a Canadian network of community hospitals located within a reasonable driving distance from the PCI centre. These data may, therefore, not be applicable to networks involving longer transfer delays.
In conclusion, immediate retransfer of carefully selected stable patients who underwent successful and uncomplicated primary or rescue PCI to their referring community hospitals without physician accompaniment during ambulance transport appears to be safe and associated with low rates of in-hospital adverse clinical outcomes. Other hospital networks may benefit from such a strategy in order to improve access to mechanical reperfusion.
Acknowledgements
We thank Dr. Brian Potter for his careful review of the manuscript.