- myocardial infarction
- percutaneous transluminal coronary angioplasty
- shock
Abstract
Aims: Treatment delay is a powerful predictor of survival in STEMI patients undergoing primary PCI. We investigated the effectiveness of pre-hospital triage with direct referral to PCI, alongside more conventional referral strategies.
Methods and results: From January 2003 to December 2007, 1,619 STEMI patients were referred for primary PCI at our cathlab through two main triage groups: i.e., 1)following pre-hospital triage (n=524), 2)via more conventional triages (n=1,095) represented by the S.Orsola-Malpighi hospital emergency department triage (hub hospital) and local hospital triage. Pre-hospital diagnosis was associated with a 76 minute reduction in pain-to-balloon time (143 [107-216] vs. 219 [149-343], p=0.001) allowing mechanical revascularisation within 90 minutes from the first medical contact in the vast majority of the patients (>80%). Clinically, pre-hospital triage showed no significant reductions in terms of adjusted long-term mortality (HR 0.81, 95% CI 0.61-1.08; p=0.16) in the overall population. However, significant adjusted survival benefits were observed in high-risk groups (i.e., cardiogenic shock, TIMI risk score >30, diabetes mellitus).
Conclusions: This study shows that pre-hospital diagnosis allows for significant reductions in primary PCI treatment delays and suggests the hypothesis that this referral strategy might provide long-term survival benefits especially in high-risk patients.
Introduction
Guidelines by the European Society of Cardiology (ESC) and US/American groups (ACC/AHA), as well as other consensus documents, have recommended the implementation of efficiently working territorial systems of care based on pre-hospital triage and fast transfer to a referral centre for the optimal treatment of patients with STEMI (ST-elevation myocardial infarction)1-3. Pre-hospital ECG acquirement has a pivotal role in the pre-hospital triage process, but pre-hospital ECGs are performed in fewer than 10% of patients with STEMI4-6. In an initial experience7 we showed that pre-hospital telemedicine based triage coupled with fast direct referral to the percutaneous coronary intervention (PCI) laboratory can provide a meaningful reduction in PPCI (primary percutaneous coronary interventions) treatment delay and might provide short-term survival benefits, mainly to patients with cardiogenic shock. In a larger STEMI population treated by PPCI, we investigate the impact of such pre-hospital strategy on treatment delays and long-term mortality rates, as compared with more conventional referral strategies.
Setting
In 2003, the Health Care Agency of the Italian region Emilia-Romagna (4 million inhabitants) fostered the development of a territorial network for the treatment of STEMI (http://asr.regione.emilia-romagna.it/wcm/asr/aree di programma/governoclinico/gr fun/pr db clinici/stpr dbgreal.htm accessed on August 10, 2009). The regional project had to be gradually implemented in all nine provinces in the region through the definition of new diagnostic and therapeutic pathways. The realisation of the project was delegated to provincial committees of experts, composed of cardiologists and 118 EMS operators, and was led by the Regional Cardiology Committee which was a task force composed of cardiologists and health administrators.
In the province of Bologna (3,702km2, 2.95 million inhabitants) there are 12 hospitals admitting STEMI patients: two PCI hospitals with a high-volume catheterisation laboratory available on a 7-day/24 hour basis, and 10 peripheral hospitals without PCI facilities. The emergency calls from the province area are received by the 118 dispatch centre of Bologna, which coordinates all the resources of the EMS. Telemedicine with ECG transmission from the ambulance through a GSM mobile phone has been gradually implemented in the vast majority of the territory. The provincial Committees considered all the resources available and, accordingly, recommended PPCI to the following patients: 1)STEMI <12 h presenting at the emergency department of a PCI centre; 2)patients triaged by the 118 ambulance system within 12 hours of symptom onset and within 60 min driving time from a PCI centre; 3)high-risk STEMI in patients who spontaneously presented at peripheral hospitals; 4)patients with absolute contraindications to fibrinolysis. Lytic therapy, preferably started in the ambulance, and immediate transfer to a CCU was recommended for all other STEMI patients presenting within 12 hours of symptom onset8. Transfer for rescue PCI was encouraged for patients with evidence of persistent ST-elevation and pain after the administration of lytic therapy. Rapid transfer back to the CCU of non-PCI hospitals was recommended for patients shortly after PPCI, generally after a few hours in the CCUs of hub centres and preferably within 24 hours, provided no serious complications had arisen. Since June 2003, STEMI patients who call the 118 dispatch centre of Bologna, within a 60minute drive range from a PCI centre, are directly transported to the cathlab after pre-hospital, ambulance-telemedicine diagnosis (thus bypassing the emergency department and the coronary care unit)7.
Study design and selection criteria
This retrospective analysis investigated all patients referred for PPCI at the S.Orsola-Malpighi intervention laboratory due to STEMI either 1)within 12 hours of the self-reported onset of symptoms, or 2)beyond this time limit in the presence of symptomatic/ECG evidence of continuing ischaemia, with onset prior to hospital admission. No restrictions based on age, sex or clinical status were applied. The study period comprises the years 2003-2007. Informed consent (for PCI, participation in the study protocol and anonymous publication of scientific data) was systematically sought whenever possible; in line with national practice, patients in coma or cardiogenic shock were treated and are anonymously reported in the study (no patient was excluded due to lack of informed consent). This retrospective cohort study (conceived in accordance with the principles of the most recent revision of the Declaration of Helsinki) was based on a prospectively collected database (at S.Orsola-Malpighi intervention laboratory).7,9,10 The database contains demographic information, comprehensive clinical, ECG and procedural data concerning STEMI patients treated by primary PCI and was approved by the ethics committees of the S.Orsola-Malpighi hospital.
Outcome measures
Analysis was based on comparison of the outcomes associated with two main triage groups: i.e., 1)following pre-hospital triage; 2)via the more conventional triage (S.Orsola-Malpighi hospital emergency department triage [hub hospital] and peripheral hospital triages [spoke hospitals]). The main outcome measures were: 1)pain-to-balloon time, 2)long-term all-cause mortality. A decision to perform subgroup analysis in specific high-risk patients (cardiogenic shock, TIMI risk index >30, diabetes mellitus and anterior STEMI site) was planned before the data were released for statistical analysis. The statistical analysis plan was developed in December 2009.
PPCI protocol
Before performing PPCI, all patients received aspirin (250 mg i.v.) and unfractioned heparin (5000 IU i.v.). Use of β-adrenergic blocking agents, nitrates, and IIb/IIIa agents during the PCI procedure was strongly encouraged. In the first two years of the provincial network (2003-2004), pre-procedural administration of IIb/IIIa agents was mainly encouraged in patients transferred from spoke hospitals and in patients with large myocardial infarction (i.e., anterior myocardial infarction). Furthermore, until 2005, the lack of ambulance refrigeration facilities precluded on-scene administration of unfractioned heparin and IIb/IIIa agents. Since 2005, early administration has been more strongly encouraged in all settings. The drugs administered were abciximab (0.25mg/kg as an intravenous bolus, followed by 0.125µg/kg/min for 12 hours or tirofiban (as a 10µg/kg or 25µg/kg intravenous bolus, always followed by 0.15µg/kg/min for 18-24 hours). After PPCI, ticlopidine or clopidogrel was administered for at least one month to patients who received bare metal stents (for six to 12 months to patients with drug eluting stents)1.
Angiographic analysis and definitions
Quantitative coronary angiography was analysed by experienced site investigators blind to all data apart from the coronary angiogram. Culprit vessel TIMI flow grades were assessed before and after PPCI. STEMI was defined as significant ST-elevation (in two adjacent leads and ≥0.1mV in leads I-III, aVF, aVL, V4-V6 and ≥0.2mV in leads V1-V3), as recorded in a pre-hospital ECG or the first ECG obtained at the hospital of admission1. TIMI risk index was calculated using the equation:11 (heart rate in bpm×[age in years/10]2)/systolic blood pressure in mmHg. Cardiogenic shock (secondary to left or right ventricular dysfunction) was defined as persistent systolic blood pressure <90mmHg (recorded in the catheterisation laboratory before PPCI or aortic balloon pump implantation), unresponsive to i.v. fluid administration or requiring vasopressor agents to maintain systolic pressure ≥90mmHg12. Pain-to-balloon time was defined as the interval (minutes) between onset of symptoms and first balloon dilatation. ECG-to-balloon time was defined as the interval (minutes) between acquirement of the diagnostic ECG (on scene in the pre-hospital triage group or at emergency departments in the conventional triage group) and first balloon dilatation.
Ascertainment of events
Long-term outcomes were ascertained by the Emilia-Romagna Regional Health Agency from coded hospital discharge records (obligatorily archived for all public/private Italian hospitals) and municipal civil registries. Hospital records were reviewed for additional information whenever deemed necessary.
Statistical analysis
Continuous data were expressed as mean±SD or median (25th-75th percentiles), as appropriate, and categorical data as counts (percentages). Group comparisons of categorical variables were conducted using the chi-square test with Yates correction. The two-tailed Student t test was used to compare normally distributed continuous variables. Comparisons of non-normally distributed variables were conducted using the Mann Whitney Rank Sum test. The incidence of long-term mortality of the two study groups was estimated by the Kaplan-Meier method and compared using the Log-rank test. Cox proportional-hazard regression analysis was used to assess whether pre-hospital triage was an independent predictor of long-term death in the overall study population and in the prespecified patient subgroups. The following potential confounders were included in the multivariable model: age (continuous variable), gender, year the procedure was performed, anterior infarction site, cardiogenic shock, diabetes, hypertension, hypercholesterolaemia, history of smoking, prior infarction, prior PCI, prior coronary artery bypass intervention, multivessel coronary disease, pre-PCI TIMI grade flow, IIb/IIIa agent administration. Analyses were conducted using SPSS for Windows, release 17.0 (SPSS Inc, Chicago, IL, USA). All p-values refer to 2-tailed tests of significance; p <0.05 was considered significant.
Results
Characteristics of the study population
In the study period (January 2003 to December 2007), a total of 1,768 patients with STEMI underwent PPCI at our cathlab within 12 hours of symptom onset (or longer in the presence of persisting ischaemia). Of these, 1,619 patients satisfied the eligibility criteria (after exclusion of 68 patients who underwent rescue PCI and 81 who developed STEMI after hospital admission). Pre-hospital triage was carried out in 524 patients (32% of the eligible patients). Of note, the rate of patients who underwent pre-hospital ECG increased during the study period: 12% in 2003 (implementation started in June 2003), 35% in 2004, 36% in 2005, 36% in 2006, 41% in 2007. Table1 reports the basal clinical characteristics and risk factors of the study population according to the type of triage. Baseline clinical assessment was done for all subjects on cathlab arrival, before PCI accomplishment. The two groups were comparable in terms of clinical characteristics (systolic pressure was slightly lower in the pre-hospital group whilst heart rate appeared slightly higher in the other group). As regards angiographic and procedural characteristics (Table 2), significant differences between the two groups only regarded pre-procedural TIMI flow (the pre-hospital triage group was associated with a higher frequency of unfavourable TIMI flow (probably due both to the shorter treatment delay and the unavailability until 2005 of heparin and IIb/IIIa agents in ambulances) and the rate of administration of IIb/IIIa agents (higher in the pre-hospital triage group).
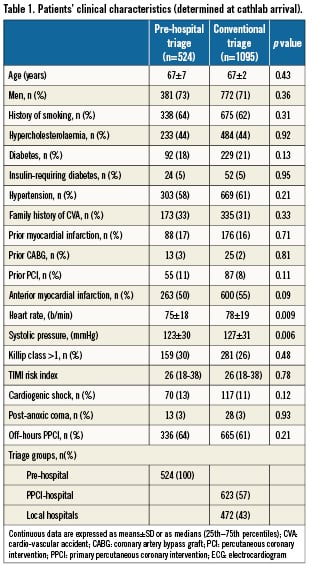
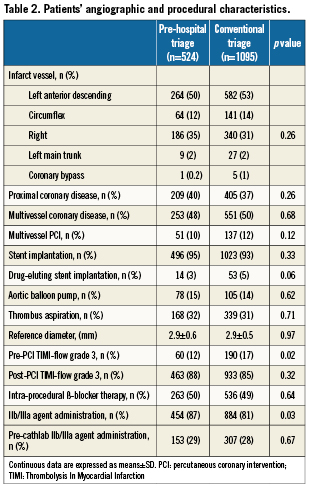
Treatment delay
Door-to-balloon time differed considerably between the two study groups, with the pre-hospital triage group showing the shortest time: 143 (107 – 216) vs. 219 (149 – 343) min for the conventional triage group (p=0.001) (Table 3). Of note, revascularisation within three hours of symptom onset was obtained in 67% of
pre-hospital triage patients vs. 37% of conventional triage patients (p<0.001) (Table 3, Figure 1). Notably, only pre-hospital triage was associated with an ECG-to-balloon time (to a certain extent equivalent to door-to-balloon time) less than 90 min in more than 75% of the patients (82% vs. 59%, p < 0.001) and with an ECG-to-balloon time less than 120 min in 95% of the patients (Table 3, Figure 2). Cathlab arrival-to-balloon time was 21 minutes in both groups.
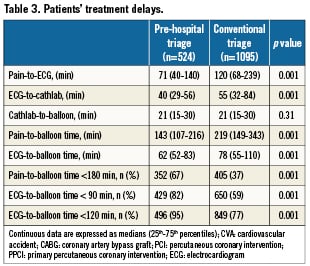
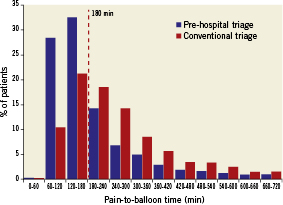
Figure 1. Histograms of the percent distribution of pain-to-balloon time among STEMI patieAnts undergoing PPCI following pre-hospital triage or conventional triage. The dashed red line indicates the 3-hour time limit.
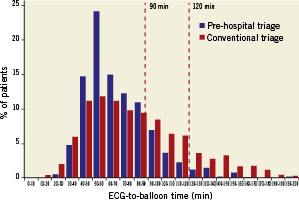
Figure 2. Histograms of the percent distribution of ECG-to-balloon time among STEMI patients undergoing PPCI following pre-hospital triage or conventional triage. The dashed red lines indicate the 90 and 120 minute time limits.
Long-term outcome
Outcomes were ascertained for 1,595 (99%) patients. The median follow-up was 578 days (25th-75th percentile, 391– 886) in the overall population, 549 days (386-730) in the pre-hospital triage group and 597 (399-964) in conventional triage patients. During the in-hospital and follow-up periods, 72 and 185 patients died respectively in the pre-hospital and conventional triage groups. Figure3A reports survival curves in the overall study population according to the type of triage. The analysis, based on the Kaplan-Meier method, did not show significant differences in terms of 2-year incidence of all-cause mortality (15% vs. 17%; p=0.23) between pre-hospital and conventional triage groups. Differences were more apparent in high-risk subgroups of patients: cardiogenic shock (n=187, 33% pre-hospital triage vs. 53% conventional triage, p<0.01) (Figure3B), TIMI risk score >30 (n=643, 28% vs. 33%, p=0.12) (Figure4A) and diabetes (n=321, 22% vs. 27%, p=0.18) (Figure 4B). At Cox multivariable regression analysis (adjusting for potential clinical, logistic and procedural confounders [see above]), pre-hospital triage was not associated with a significant reduction of death in the overall population (HR 0.81, 95% CI 0.61-1.08; p=0.16). However, in the overall population analysis it was possible to detect significant interactions between pre-hospital triage and cardiogenic shock (p=0.02), pre-hospital triage and TIMI risk score >30 (p=0.04), and pre-hospital triage and diabetes (p=0.03). Notably, pre-hospital triage led to significant adjusted long-term mortality reductions in cardiogenic shock (HR=0.54, 95% CI 0.32-0.92, p=0.02), TIMI risk score >30 (HR=0.71, 95% CI 0.51-0.99, p=0.04) and diabetes (HR=0.51, 95% CI 0.28-0.92, p=0.02). As reported in Figure 4C, no clear long-term benefit could be detected in patients with anterior STEMI (n=863, 16% vs. 18%, p=0.39; adjusted data: HR=0.84, 95% CI 0.57-1.24, p=0.40).
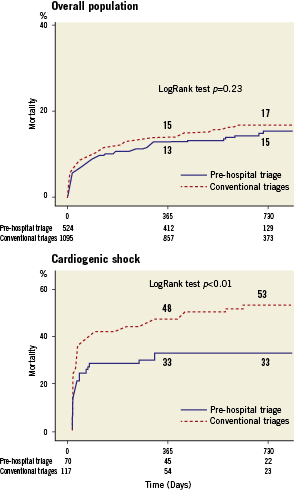
Figure 3. Kaplan-Meier curves for the overall study population (n=1,619) and cardiogenic shock (n=187) patients according to triage type: overall mortality.
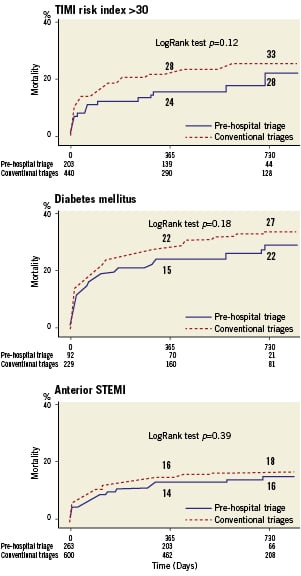
Figure 4. Kaplan-Meier curves for TIMI risk index > 30 (n=643), diabetes mellitus (n=321) and anterior STEMI site (n=863) patients according to triage type: overall mortality
Discussion
European and American STEMI guidelines state that PPCI represents the preferred treatment for STEMI patients if performed by an experienced team within 90-120 minutes of the first medical contact1,3,13. However, in the real-world, especially in STEMI patients who require inter-hospital transfer, only a minority of patients receive PPCI within the recommended time14. The creation by EMSs and hospitals of efficient systems of care that integrate the pre-hospital and hospital phases of the STEMI diagnostic-therapeutic process holds great promise for improving time to reperfusion and patient outcome2. The utilisation of pre-hospital ECG for on-scene evaluation of patients with suspected STEMI represents apivotal component in the development of the STEMI network15. However, American national experiences have shown that pre-hospital ECGs are performed in less than 10% of patients with STEMI and unfortunately their adoption has not increased in the last decade4-6. In our STEMI network setting, in which EMS providers perform on-scene ECG in all suspected acute coronary syndromes, more than 30% of the patients treated by PPCI received pre-hospital triage associated with direct transport to the catheterisation laboratory. Notably, the rate of utilisation of such triage progressively increased during the study period (years 2003-2007), reaching more than 40% in the last year of our experience, therefore denoting improvements in the network’s logistics and changes in patients’ contact behaviour patterns. As expected, this study provides evidence that implementation of pre-hospital triage can lead to a highly relevant reduction in PPCI treatment delay. Average reductions in pain-to-balloon delay appeared to be about 75 minutes as compared with more conventional triage. It seems worth noting that only pre-hospital triage was associated with a median time of reperfusion of ~ 2 hours (when the possibility of ventricular function recovery is higher16) and only this type of triage allowed ECG-to-balloon times less than 90 and 120 minutes in the vast majority (respectively 82% and 95%) of the patients (largely achieving the target of door-to-balloon times established by the D2B Alliance17 and by the international guidelines1,3). Results in a similar direction were also reported in the Ottawa preliminary experience, in which patients treated by PPCI were referred directly from the field by paramedics trained in the interpretation of ECG18. However, when compared with our data, the Canadian study reported a longer pre-hospital triage group median ECG-to-balloon time (91 vs. 62 min.), a difference which can likely be explained by triage dissimilarities between the two networks (i.e., telemedicine based ECG interpretation vs. paramedic ECG interpretation, transport of the patients directly to the cathlab vs. direct transport to the cardiac care centre) or by distinct geographic-logistic contexts. In previously reported data6,7,18,19, pre-hospital triage has shown trends for lower in-hospital mortality risk. In the present report, pre-hospital triage was associated with a not significant reduction of long-term adjusted mortality. However, interestingly, this kind of triage showed relevant survival benefits in high-risk patients like those with cardiogenic shock (46% reduction in long-term adjusted mortality), high TIMI risk score (29% reduction) and diabetes (49% reduction). These observations seem broadly in line with previous studies showing the dramatic role played by ischaemic time in patients with cardiogenic shock7,20,21 treated by PPCI. In particular, a remarkably good outcome has been documented in cardiogenic shock patients undergoing mechanical revascularisation within two hours of symptom onset7. Obviously, in a PPCI setting such very short treatment delay can be regularly achieved only by taking advantage of the possibilities of pre-hospital diagnosis. Diabetic patients with STEMI treated by PPCI have a higher risk of impaired myocardial perfusion (due to coronary microcirculation damage) and mortality22,23. In our diabetic subgroup analysis, pre-hospital diagnosis was associated with a meaningful reduction of the risk of long-term mortality. On patho-physiological grounds, this finding could be explained by the higher vulnerability of diabetic myocardium to ischaemic injury24, and highlights, particularly in such patients, the clinical importance of early coronary reperfusion.
Study limitations
This is a large single-centre registry retrospective study, thus no power analysis or sample size calculations were performed. Our analysis has several limitations and should be interpreted accordingly. First of all, the patient selection process used may be taken into account. Since we used the cathlab as a starting point, our study selected only patients eligible for mechanical reperfusion who reached the cathlab alive. Therefore, it may not represent all STEMI cases that occurred in our catchment zone during the study period. In particular, we cannot exclude that very sick STEMI patients did not reach our cathlab since they died in spoke or hub hospital emergency departments, during inter-hospital ambulance transport (conventional triage group) or during pre-hospital triage. Secondly, our results may be partially influenced by several recognised and unrecognised selection biases. Although the study groups were well matched with regard to baseline clinical and angiographic characteristics, the lack of ambulance administration of heparin and Gp IIb/IIIa inhibitors (until 2005) could at least partially explain the higher frequency of unfavourable pre-PCI TIMI flow in the pre-hospital group. A further bias regards the known tendency of sicker patients to call ambulance services, a factor that explains the high prevalence of cardiogenic shock in the pre-hospital triage group. Both these findings represent negative biases potentially decreasing the favourable effect on mortality of the pre-hospital diagnosis strategy that in more comparable patients groups could consequently still turn out more effective. As reported in our provincial network organisation protocol, spoke hospitals were encouraged to transfer mainly high-risk patients for PCI. Probably as a result of this selection criteria, the conventional triage group showed a slightly, not statistically significant, higher incidence of anterior STEMI. Moreover, to overcome some of these limitations we tried to control for known prognostic factors (i.e., anterior STEMI site) by means of statistical adjustment (multivariable regression analysis). However, since the use of adjustment cannot address the problem for unknown or unmeasurable prognostic factors and considering that no type of statistical adjustment can completely overcome the pitfalls of non-randomised comparisons, our results should be interpreted with caution. The striking results regarding patients with cardiogenic shock, TIMI risk index >30 and diabetes were generated by a numerically limited subgroup analysis; however, the decision to perform these analyses was taken before the data were released for statistical analysis, in consideration of pathophysiological aspects and previously reported data. Therefore, the potentially significant hypothesis that pre-hospital telemedicine based triage may provide major clinical benefits for high-risk patients needs to be tested in more adequately powered dedicated studies. Finally, this study focused on patients not receiving fibrinolytic therapy, living (in the vast majority of cases) within a 90 minutes drive of a PCI centre, in an Italian province covered by a mobile phone network and with an adequate territorial distribution of emergency vehicles. Since transfer patients commonly undergo transport times in the 120-minute range25, it should be underlined that the encouraging results of the present study may not be automatically replicated in less favourable settings.
Conclusion
This study indicates that pre-hospital triage with direct transportation to the cathlab is associated with great reductions of treatment delay, allowing prompt mechanical revascularisation in the vast majority of the patients (>80%). As regards clinical outcome, the results of the present study suggest the hypothesis that a pre-hospital triage strategy might provide long-term survival benefits especially in high-risk patients like those with cardiogenic shock or diabetes.
Conflict of interest statement
The authors have no conflict of interest to declare.