Abstract
Early ambulance services often confined their activities to a “scoop and run” approach, conveying sick patients quickly to the nearest emergency department. With the advent of modern ST-elevation myocardial infarction (STEMI) management and primary percutaneous coronary intervention (PPCI), the role of the emergency medical service (EMS) has expanded significantly. This review discusses the critical and evolving collaboration between the EMS and the heart attack centre.
Speed of reperfusion is a major determinant of outcome in STEMI and, whilst the patient delay (symptom to call time) has a central role in this, system delay (first medical contact to balloon time) is linked to mortality and is used to measure the response of a PPCI programme and is a key element of contemporary guidelines.
In addition to rapid diagnosis and transfer to the heart attack centre, the EMS has to deliver a growing number of established treatments including resuscitation and drug therapy. EMS also continually needs to develop expertise in new techniques such as advanced management of cardiac arrest patients, including automated cardiopulmonary resuscitation, and will need to deliver newer therapies if trials support their use, including cooling and preconditioning.
Ultimately, the EMS has a central role in the management of STEMI patients which needs to be fully aligned with the heart attack centres. This integration of services is perhaps best regarded as the Heart Attack Team.
Introduction
Diagnosis triage and treatment in the field are not new concepts, dating back at least as far as the Roman Empire. However, for certain very time-dependent illnesses such as heart attack, stroke and major trauma they are particularly important. In such conditions significant patient benefits can be achieved with early identification diagnosis and treatment but very importantly with transfer to the most appropriate, and not necessarily the nearest hospital. This “left shift” of management and key decision making to the earliest possible time point by the emergency medical service (EMS) mandates a high level of organisational structure, clear management pathways, effective communication, training, clinical judgement and an integrated team approach (Figure 1).
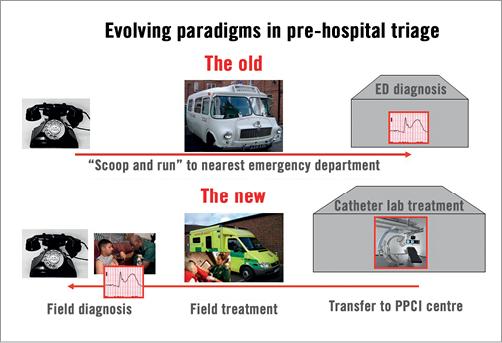
Figure 1. The “left shift” of diagnosis, triage, treatment in the field, and transfer to the appropriate hospital by the emergency medical services is particularly important in heart attack management.
Chest pain from an emergency medical service perspective
In the metropolitan area of London, there is a resident population of about 7.5 million, served by eight primary percutaneous coronary intervention (PPCI) 24/7 heart attack centres. In 2010-2011 the London Ambulance Service (LAS) received approximately 1.5 million emergency calls. Of these, around 70,000 (5%) were for chest pain, and 15,393 (1.0%) considered due to an acute coronary syndrome1. Therefore, from an EMS perspective, heart attack patients have to be cared for in the context of a large non-cardiac workload.
The “Heart Attack Team”
Over recent years a growing realisation has developed that specialist healthcare is best provided by a team approach. This is particularly relevant in cardiology where international guidelines now recommend a team approach centred on multidisciplinary meetings (MDTs) engaging all of the relevant parties including cardiologists, cardiac surgeons, imaging physicians, anaesthesia and intensive care teams, nursing and other healthcare colleagues. This concept has been embraced by the European Society of Cardiology (ESC) both in the “Heart Team” and in the development of patient-centred revascularisation guidelines co-authored by cardiologists and surgeons rather than the more traditional specialty-orientated documents2.
The concept of the “Heart Team” is a fairly hospital-orientated vision. Where heart attacks are concerned, however, pre-hospital EMS decision making and management are vital. Whilst system delay (first medical contact to balloon) is very important, associated with mortality3, and forms the basis for national and international guidelines2,4,5, from the myocardial salvage or infarct size reduction perspective, reducing the overall ischaemic or symptom to balloon time is critical.
Patients and the public are perhaps the most important link in the chain since calling for help is integral to launching the PPCI pathway. In addition, members of the public can give cardiopulmonary resuscitation. Reduction in patient delay (symptom onset to call) times is an important challenge for public education programmes which have historically struggled to make a big impact6. In spite of these difficulties, efforts are ongoing in many areas to increase awareness of chest pain and, for example in France, there is now evidence developing of a progressive reduction in patient delay7.
It is clear that the EMS is equally as important as the PPCI centre in heart attack care and thus it is logical when discussing optimal heart attack care to think of the Heart Attack Team (Figure 2). The EMS should be trained effectively as an integral “outreach team” of the PPCI centre with completely integrated protocols giving continuity of patient care.
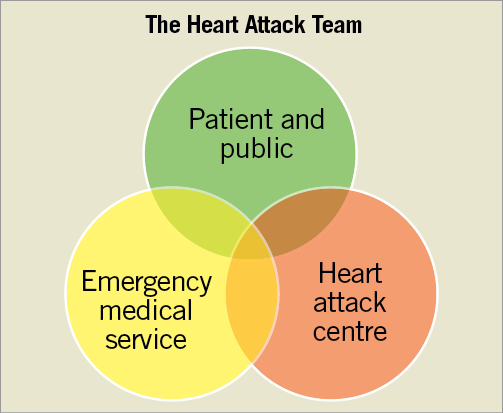
Figure 2. Whilst the Heart Team is a predominantly hospital-based concept, the Heart Attack Team must engage fully with the public and emergency medical service. This is particularly important in the planning of unified protocols and pre-hospital therapy.
From the concept of the Heart Attack Team it is clear that all parties including patients, the EMS and the heart attack centres need to be engaged for the effective rollout and delivery of primary angioplasty. The service cannot be delivered effectively by the hospital alone.
Training and empowering the emergency medical services
At the present time, the immediate diagnosis of heart attack is based on clinical assessment and the ECG. Whilst biomarkers are central to the revised definition of myocardial infarction8, conventional markers take hours rather than minutes to be diagnostically useful and thus give information which is outside of the immediate time frame necessary for decision making about emergency revascularisation with PPCI.
There are a number of models for pre-hospital diagnosis of heart attack in operation: from medically staffed ambulances, a full telemedicine style approach with telemetered ECG and remote patient assessment and interview, all the way to fully autonomous paramedic diagnosis and triage. All models have their strengths and weaknesses. Furthermore, different models can be better suited to different healthcare systems and geographical locations. In London, where there are eight 24/7 PPCI centres, relatively small travel times are involved and the diagnosis of STEMI and referral for consideration of PPCI is made fully autonomously by the ambulance crews.
In addition to the diagnostic model used, different services use different criteria for acceptance of patients to PPCI programmes. Although technical criteria typically mirror those for thrombolysis (typically chest pain believed cardiac <12 hours and ST-elevation in two or more ECG leads or left bundle branch block believed new) application of criteria varies from strict acceptance of clear-cut chest pain and ECG changes through to less clear presentations, for example with breathlessness and/or less categorical ECG changes. There are arguments in favour of both strategies. Strict criteria acceptance will result in a high proportion of patients having a true STEMI and undergoing PPCI; however, some patients actually having a heart attack with less clear presentations will not receive PPCI. Less strict criteria will result in patients with true heart attacks but less clear presentations receiving PPCI, but significant numbers of activations of the PPCI system for patients not ultimately having heart attacks. Indeed, recent guidelines specifically make the point that some cases of acute myocardial infarction do not have clear-cut ECG changes, particularly early in the presentation4. It is testament to the clinical judgement of modern EMS crews that a significant number of such cases in London, which would not technically reach “protocol positivity” for ST-elevation but are referred on the strength of the clinical presentation, do nevertheless have acute coronary occlusion9. Different approaches have strengths and weaknesses, and their applicability may also depend upon local resources and existing pathways of care.
EMS crews can be trained in ECG interpretation and indeed there is evidence that they can be at least as effective as junior doctors in emergency departments in this regard10. Crews have the additional advantage that their attention is focused usually on a single patient rather than a busy emergency department. Undoubtedly fully autonomous ambulance diagnosis, activation of PPCI pathways and direct transfer to the catheter laboratory are feasible, are presently in clinical practice including in the London network, and can reduce delays and deliver very rapid revascularisation in PPCI11,12.
All diagnostic communication between ambulance and heart attack centre takes time. Thus, from a heavily ECG telemetry-dependent or fully telemedicine-dependent system through to a fully autonomous system, EMS advanced clinical skills and ECG interpretation are of significant benefit to the patient. Many heart attack centres now actively engage their EMS in regular collaborative training to enhance pre-hospital diagnostic and treatment skills.
Ambulance resource deployment and geographical considerations
Different countries and geographical locations have different EMS providers and networks. As a result, local solutions need to be reached for specific regions and networks of care. In general it is easier to organise the emergency EMS response to a suspected heart attack when there is one principal centrally controlled ambulance provider. However, as long as communication is clear, multiple ambulance providers can serve a given geography.
Ambulance services typically have a number of response vehicles available including patient transfer ambulances, rapid response vehicles without patient-carrying capacity, motorcycles, and sometimes pedal cycles for metropolitan and indoor use. Rapid response vehicles or bikes can be deployed in strategic locations, allow rapid response, ECG recordings, resuscitation, defibrillation and the administration of drugs and other evolving pre-hospital therapies. Ultimately, however, a vehicle with patient-carrying capacity will be required to transfer a patient for PPCI.
When large distances or slow road journeys are anticipated, sometimes air transfer can save time. Although this approach sounds attractive there are a number of important limitations, particularly when land journeys are feasible. Whilst aircraft (rotary or fixed wing) fly fast compared with land vehicles, the logistics of getting the patient from the scene to the aircraft, and then from the aircraft to the cardiac catheter laboratory are complex and can easily result in an air transfer delivering a longer call to balloon time than a long land ambulance journey. On the other hand, if a rotary wing aircraft can be alerted and dispatched very early, land very close to the scene, take off and land very close (preferably a trolley push rather than secondary transfer) to the cardiac catheter lab then there are very significant gains to be made13. In spite of these benefits, however, depending on local weather patterns, resource and aviation regulations, aeromedical transport availability can be restricted and a robust full 24/7 service may not be available requiring a surface transport solution.
However the transfer is coordinated, it is vital that the PPCI centre is alerted so that the cardiac catheter laboratory is ready to receive the patient immediately. It is also important that the PPCI centre is aware of the clinical status of the patient, including out-of-hospital cardiac arrest (OOHCA) or cardiac arrest with return of spontaneous circulation (ROSC), so that an anaesthetic team can be made available on patient arrival including the provision of further resuscitation such as mechanical CPR and facilities for therapeutic hypothermia if indicated.
Inter-hospital transfer for primary angioplasty
Primary angioplasty and the heart attack team work at their best from a logistic standpoint when patients call promptly for help, the EMS arrives quickly, makes a rapid diagnosis, goes directly to the cardiac catheter laboratory and the PPCI procedure is performed as soon as possible. When such a pathway occurs, reperfusion times are usually within recommended guidelines and significant myocardial salvage is achievable. Unfortunately, the patient pathway is not always as smooth as this. A significant number of STEMI patients do not present in this manner and fall into two main categories: those who self-present to the emergency department, with either an immediate or subsequent diagnosis of ST-elevation MI, and those who are assessed by the EMS and are not felt to be having a clinically overt STEMI at presentation, taken to the nearest emergency department and when reassessed are felt to be having a STEMI or subsequently develop clear ST elevation. In either scenario, patients can end up at a hospital which is not equipped to perform an immediate PPCI procedure.
This scenario has been the subject of a number of randomised trials, since a secondary inter-hospital transfer to a heart attack centre will add very significant delay, raising the question of whether immediate local thrombolysis might be superior to transfer for PPCI. In the event, although in some specific scenarios thrombolysis may have merits (see section on pre-hospital therapies below), overall the randomised trials generally support immediate transfer for primary angioplasty when distances are not prohibitive even with the attendant delays14.
Following the results of the “transfer for PPCI” trials, most PPCI networks adopt an inter-hospital transfer strategy for patients who for whatever reason find themselves in a non-PPCI centre with an ST-elevation MI. These cases are a logistical challenge. There is a tendency for prolonged inter-hospital discussions to take place, especially in unclear cases. In London this problem has been addressed by a “send first phone second” policy. Even when the diagnosis is secure, however, it can be challenging to raise an ambulance and to get the patient out of the first hospital quickly. On the one hand, such patients are in a “place of safety” with a heart monitor and defibrillator and thus it could be argued that such patients might not have the priority of an emergency in the community. On the other hand, they are at risk of long reperfusion times, and are a common reason for breeching of guidelines. Inter-hospital transfer for PPCI remains a major logistical challenge.
Pre-hospital therapies
The development of more advanced therapies, some of which may be effective when given prior to PPCI, has extended further the role of EMS crews in the pre-hospital setting. Many EMS services were engaged in pre-hospital thrombolysis during the thrombolytic era and thus have a background in clinical decision-making protocols, drug administration and concepts of risk and benefit in this context.
The widespread adoption of PPCI has resulted in a dramatic fall in thrombolysis. Unfortunately, the intuitively attractive approach of thrombolytic “facilitation” en route for PPCI, especially where long journeys are concerned, was not supported by the ASSENT-4 PCI randomised trial which was stopped due to an excess of adverse outcomes in the facilitation arm15, although in some networks this strategy is used and may be helpful when long transfers are anticipated.
Similarly a “facilitation” approach with intravenous glycoprotein IIb/IIIa antagonists did not appear to confer a major advantage in the FINESSE or AGIR-2 trials16,17. However, the ON TIME-2 trial and subsequent pooled analysis of its two phases suggested improved ECG ST-segment resolution and clinical outcomes with pre-hospital tirofiban for STEMI patients undergoing PPCI18,19. As a result, upstream glycoprotein IIb/IIIa treatment prior to PPCI for STEMI may have a role in some clinical networks and scenarios, and has been upgraded from a level III to IIb recommendation in the most recent 2012 ESC STEMI guidelines4. The ongoing Euromax trial20 is comparing pre-hospital bivalirudin with current “standard of care” in the context of PPCI.
The recently published STREAM study21 investigated a different strategy known as the “pharmacoinvasive” approach (as distinct from “facilitation” where the intention is PPCI as soon as possible). For the subgroup of early presenting (<3 hours) patients who cannot undergo PPCI within an hour of first medical contact, the study found that a strategy of pre-hospital thrombolysis, transfer and “timely” angiography (median 17 hours) with rescue PCI reserved for patients who did not reperfuse with thrombolysis might be as effective as PPCI.
From the perspective of oral antiplatelet agents, virtually all patients suspected of having a heart attack receive pre-hospital aspirin in the absence of a serious contraindication. Dual antiplatelet therapy (DAPT) is routine in PPCI and many EMS programmes administer both aspirin and clopidogrel for patients with STEMI. Recently two new antiplatelet agents, prasugrel and ticagrelor, have become available for use with aspirin as superior alternatives to clopidogrel for DAPT in STEMI treated with PPCI, and their use is supported by current guidelines4. The reported rapid efficacy of these new antiplatelet agents (which are typically administered in the PPCI centre) has recently been challenged in this clinical context22, something which is of concern in an era of falling glycoprotein IIb/IIIa antagonist use. The ongoing ATLANTIC study23 is comparing the efficacy of pre-hospital and in-hospital ticagrelor prior to PPCI for STEMI and may help address this important issue.
Whilst PPCI remains the standard of care for reperfusion in STEMI, it is clear that pre-hospital antithrombotic drug therapy is a rapidly developing field, and it is essential that EMS programmes work closely with their hospital colleagues to agree coordinated drug protocols that progress appropriately with clinical guidelines.
Non-pharmacological pre-hospital therapies are not yet in widespread mainstream use; however, a number of approaches have been deployed and are under active investigation.
Mechanical CPR machines for prolonged cardiac arrest offer a more consistent circulatory output than manual CPR and, importantly, free up EMS crews to deal with other key tasks.
Remote preconditioning describes the process of inducing intermittent ischaemia (typically in the arm or leg with a pressurised cuff) to increase myocardial salvage and reduce infarct size. This therapy is very feasible and may be effective in the pre-hospital setting24. Whilst the mechanism of the benefit remains to be fully explained, remote preconditioning is the subject of ongoing investigation.
Therapeutic hypothermia (cooling) in hospital has been shown to improve neurological recovery in comatose OOHCA/ROSC patients25,26. Pre-hospital cooling might confer further benefits; however, it is a logistical challenge. Furthermore, it is difficult to maintain hypothermia on arrival at hospital and through the transition from EMS to hospital-delivered hypothermia27. That said, some programmes are actively engaging in pre-hospital cooling, and newer devices and techniques such as trans-nasal cooling, the feasibility of which is currently being investigated in London and other networks, may make this process more effective28.
Whether a facilitation or even a pharmacoinvasive strategy is adopted, what is clear is that STEMI patients should be transferred as soon as possible to a PPCI centre. The advent of yet more choices of pre-hospital therapy, many of which interact with in-hospital and catheter laboratory therapies, mandates close working between the pre-hospital and in-hospital members of the Heart Attack Team: this includes the planning stage when deciding what therapeutic strategies to adopt in the network in question.
Out-of-hospital cardiac arrest (OOHCA)/return of spontaneous circulation (ROSC) and shock
Even after the implementation of primary angioplasty protocols for clinically stable STEMI patients, many healthcare networks relied on immediate transfer to the nearest hospital (which was often not a PPCI centre) for some of the highest risk patients such as those with OOHCA/ROSC and cardiogenic shock. The concept of heading to the nearest “place of safety” and avoiding potentially longer journeys for such patients appeared to have some attractions; however, such high-risk patients, whilst having a high mortality risk, can gain the most from an aggressive specialist approach both in the ambulance (including the advanced therapies discussed above) and at the centre.
Incremental improvements in resuscitation, including improved cardiopulmonary resuscitation, use of therapeutic hypothermia and PPCI, have been shown to improve outcomes in OOHCA patients29. This concept is supported by international guidelines which recommend that these high-risk patients are transferred to a specialist facility with a full post-cardiac-arrest service, including therapeutic hypothermia and primary angioplasty30. As a result, EMS crews need to be engaged in network-wide OOHCA/ROSC protocols and maintain close contact with their local heart attack centres. In London and many other cities and regions a network-wide agreement has been reached such that all OOHCA/ROSC patients are transferred direct to a PPCI unit for consideration of immediate PPCI and other post-cardiac-arrest therapies.
From ambulance to catheter laboratory
However effective the EMS is at diagnosing and transferring STEMI patients to the heart attack centre, and however fast the catheter laboratory response, losing time between the ambulance “wheel stop” to getting the patient into the catheter lab is a common cause of revascularisation delay. The concept of “assessment” of the patient in a separate clinical area may help occasionally, but in general serves only to slow down the process. With a modern EMS service the ambulance is effectively the coronary care unit, and the next stop should be the catheter laboratory, which is an excellent assessment, monitoring and resuscitation environment. The best way to encourage this “direct from ambulance to lab” approach is to ensure that EMS crews feel entirely at ease working with the catheter laboratory team as part of the Heart Attack Team. EMS crews can be trained to understand the issues of sterile fields and radiation protection such that they can be fully integrated members of the catheter laboratory team. They are able to explain to the patient what will happen, brief the hospital team, transfer the patient onto the catheter laboratory table simultaneously with hospital staff transferring ECG monitoring and preparing to undertake the PPCI procedure.
Non-ST-elevation myocardial infarction
Non-ST-segment elevation ACS (NSTEMI) when associated with a biomarker rise is, according to the revised criteria, myocardial infarction8. Indeed the six-month mortality rates for STEMI and NSTEMI are similar31. On that basis, one might imagine that emergency revascularisation with primary angioplasty could be beneficial for NSTEMI as well as STEMI patients. A routine invasive approach for NSTEMI patients seems to be superior to a selective invasive approach32, and an early approach (<24 hours) seems to be superior to a more delayed strategy for high-risk patients33. This is reflected in contemporary guidelines34,35. The benefits of a routine immediate “primary” intervention approach have not been proven in the absence of evidence of ongoing refractory ischaemia36-40.
The Direct Angioplasty for Non ST Elevation Acute Coronary Events (DANCE) pilot study is exploring the concept of primary angioplasty for clinically overt at presentation high-risk ACS patients in London41, with fully autonomous ambulance diagnosis and triage direct to the heart attack centre cardiac catheter laboratory, and may provide further insight.
From an EMS perspective, NSTEMI which is clinically “overt” at presentation (i.e., with a compelling clinical presentation and ECG changes) will be important if a primary angioplasty strategy proves to be clinically useful. In any case, guidelines are progressively recommending an earlier invasive approach for high-risk cases, and thus it is inevitable that the role of the EMS will grow for this patient group. Further to this, healthcare systems incorporate specialist hospitals as well as general hospitals, and thus pre-hospital recognition of high-risk NSTEMI will allow direct transfer to the heart attack centre, reducing delays and secondary transfers whilst expediting the provision of specialist care.
In London a programme of direct 24/7 access to the PPCI centre for clinically overt at presentation high-risk ACS patients is being rolled out. Such patients will then have the option of immediate angiography±revascularisation if deemed clinically appropriate.
Conclusions
The EMS is equally as important as the PPCI centre in delivering efficient heart attack care. The pre-hospital team should therefore be trained effectively as an integral part of any PPCI programme with completely integrated protocols giving continuity of patient care and delivering established and developing pre-hospital therapies. The Heart Attack Team model embraces these concepts, such that all parties including patients, the EMS and the heart attack centres are engaged for the effective rollout and delivery of primary angioplasty.
Conflict of interest statement
M. Dalby reports undertaking consultancy work for Eli Lilly, Daiichi Sankyo-Lilly Alliance, AstraZeneca, Boston Scientific and receives research support from Abbott Vascular, Daiichi Sankyo-Lilly Alliance and Medtronic. M. Whitbread has no conflicts of interest to declare.