Guidelines exist to help operators, hospitals and regions provide best practices for treating patients with ST-elevation myocardial infarction (STEMI): the recommendations of guideline writing groups are based upon the best evidence available and provide a foundation upon which to build a primary PCI programme1,2. Thus, it is interesting to discover areas where guidelines are potentially ignored. An example of such discordance was evident 15 years ago: the STEMI guidelines cautioned against routine angiography after fibrinolysis (Class IIB)3. However, the majority of clinicians in the USA ignored this advice and proceeded early to the catheterisation laboratory to confirm and potentially improve culprit artery patency via percutaneous coronary intervention (PCI)4-6. The post-lytic PCI rebellion was not necessarily a misguided approach to STEMI care. As demonstrated in registries and randomised clinical trials, clinicians acted with a leap of faith: patients referred for routine early angiography after fibrinolysis were at the forefront of pharmacoinvasive therapy7,8.
In this issue of EuroIntervention, two groups present registry studies addressing “grey areas” in STEMI care with leaps of faith that go beyond current guidelines and recommendations. Schoos et al describe a mega primary PCI centre serving 2.5 million inhabitants, a task that might be considered overwhelming9; Tarkin et al present a retrospective analysis identifying the challenges of treating STEMI patients requiring inter-hospital transfer, accepting 20-minute differences in median treatment delay for transfer patients as compared to direct presenters for primary PCI10. These rebellions in primary PCI span the space-time continuum of STEMI care: what is the maximum distance allowed for a regional primary PCI programme, what is the maximum time delay allowed to favour primary PCI over a pharmacoinvasive approach? A closer look at these leaps of faith defines the cutting edge of clinical care for patients with STEMI.
Space and primary PCI
The maximum regional space afforded to a primary PCI centre is challenged by the findings of the Schoos et al registry study. Two aspects of space are considered in this analysis: 1) the physical span of geography covered by a single primary PCI centre, and 2) the maximum annual volume of primary PCI procedures experienced by a single institution and selected operators. While a prior survey of European primary PCI practice in 2010 showed a general catchment population of 300,000-1.1 million inhabitants per centre11, two findings from this prior study should be noted. First, there are heart attack centres already in existence that are serving larger populations: for example, Finland has two centres serving populations exceeding 2 million patients per centre and Denmark has five centres averaging approximately 1.1 million patients per centre. Second, the Widimsky et al survey was not intended as an outcomes study –the description of European clinical practice did not preclude better, worse or similar outcomes with smaller or larger spatial territories ascribed to regions.
However, there is logic to limits of space and volume. An overload of primary PCI patients –24 hours a day, seven days a week– could lead to unintended delays in treatment due to competition for catheterisation laboratory space, hospital beds and operator fatigue. To counter these potential adverse effects, the Danish group has demonstrated a methodology for high-volume mega-centre primary PCI programmes:
– Establish a national reperfusion strategy including a commitment to primary PCI with 12-lead ECG and defibrillator capability mandatory at first medical contact, with a predetermined upstream pharmacology plan to maximise efficiency.
– Enhance emergency medical services with simultaneous on-site physician support and transmission of pre-hospital ECG to the primary PCI centre. This allows re-routing of all confirmed STEMI patients to the primary PCI centre with ground transport for 85% of all STEMI patients.
– Incrementally fund an interventional cardiologist and three nurse staff members in-hospital around the clock for primary PCI, with a second ad hoc primary PCI team on call.
– Establish a post-PCI plan for length of stay (65% on a three-day fast track, based upon lower risk features) to maximise efficient use of hospital beds for a high-volume primary PCI programme.
Using this comprehensive strategy, the Danish team defied the limits of space: after merging the two primary PCI centres, time from diagnostic ECG to balloon decreased by 18% (p<0.001) with no adverse impact on any other time-related parameter or all-cause mortality.
A further sign that high volumes were associated with quality improvement, not quality detriment, was a dramatic increase in pre-hospital triage over time: from 38% to 72% of all STEMI patients between 2010 and 2012. These findings are consistent with a recent analysis of the transfer STEMI population in the USA: for every 50-patient increase in primary PCI volume, primary PCI centres were 32% more likely to achieve guideline recommended reperfusion goals12. In conjunction with the Danish mega-centre registry results, these findings suggest there is no U shape curve defining the relationship of space, volume and outcomes (Figure 1). Rather, such findings are a call to revise recommendations in favour of emphasising the potential benefits of higher-volume primary PCI centres that use ample support, proven quality initiatives and pre-established algorithms to achieve best outcomes for patients13.
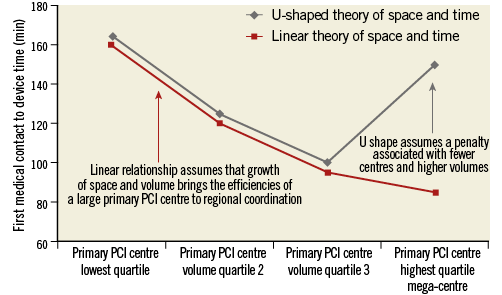
Figure 1. Two different theories of primary PCI regionalisation: U-shaped vs. linear. The relationship between first medical contact to device times and the size of a primary PCI programme may follow two potential courses. For both curves, a low-volume primary PCI centre may be expected to have inefficiencies related to inconsistent and infrequent transfer/triage algorithms resulting in increased times to reperfusion. On the other hand, the concept that very high volumes and large regions of service are associated with delays (the U-shaped curve) is not clearly supported: it seems more likely that the relationship between better reperfusion times and larger regional spaces/volumes of primary PCI may be linear and steadily improve in the setting of enhanced support, pre-established algorithms and emphasis on pre-hospital triage to the high-volume primary PCI centre.
Time and primary PCI
The clinical practice of primary PCI for the transfer population continues to subvert guideline recommendations: first medical contact to device times in this population are frequently greater than 120 minutes12-14, yet there are no signs that clinicians are embracing a pharmacoinvasive approach in this situation of delay. The study by Tarkin et al provides a rational explanation behind the ongoing rebellion against this fixed time-outcome determination10. In a retrospective registry analysis of primary PCI patients treated at a single London heart attack centre, patients who presented to non-PCI hospitals and required inter-hospital transfer had a 20-minute increase in their call to balloon times (p<0.0001) compared to patients presenting directly to primary PCI centres. Despite this delay associated with inter-hospital transfer STEMI patients, hospital mortality rates among direct presenters and transfer patients were identical (1.7 vs. 1.5%, p=0.89).
There are two key observations from this registry analysis:
1) Despite a well-organised system for pre-hospital triage and transport directly to a primary PCI centre, many STEMI patients continue to present first to a non-PCI centre.
2) While first medical contact to device times are frequently >120 minutes and such delay has a potential mortality price15, the differential between direct presentation and transfer STEMI populations in terms of adjusted mortality may be difficult to demonstrate16. These findings are consistent with US observations regarding the transfer STEMI population: first, over 80% of the US transfer STEMI population utilises self-transport, thus removing the capability of triage and diversion to a primary PCI centre12. Second, as shown in the Minnesota Regional STEMI Program, transfer patients with delay frequently have less clear-cut diagnoses of STEMI –with indeterminate ECG, left bundle branch block and the need for further diagnostic testing prior to catheterisation– that may prompt their initial presentation to a non-PCI centre17. The cause of the delay appears to be critical in understanding the impact of time on outcomes. If delay is due to cardiac arrest and CPR, then the patient is clearly at higher risk of death; on the other hand, if the delay is due to non-diagnostic ECG changes with a CT scan performed to rule out aortic dissection, mortality impact may be negligible.
These findings lead clinicians to bend the time limitations of primary PCI as supported by the London registry findings: transfer STEMI patients may be different from directly presenting STEMI patients and the risk associated with their delay to primary PCI may be small. The finding of a fourfold increase in protocol negative ECGs in the transfer group as compared to the direct presentation group (31.6% vs. 9.4%, p<0.0001) is consistent with a component of the transfer STEMI delay being related to a necessary pause to consider other diagnostic possibilities. While these findings challenge the strict 120-minute time-outcome relationship mandated by guidelines1,2,18, they do not necessarily refute the concept that we should continue to improve regional systems with greater use of pre-hospital triage, pre-hospital pharmacology and emergency room bypass to allow both the shortest possible reperfusion time and the most efficient care of patients referred for primary PCI.
Resolving primary PCI practice and guideline discordance
The next set of ESC and AHA guidelines may need to consider these examples of discordance between recommendations and clinical practice. As with the rebellion against early angiography after fibrinolysis, the ongoing rebellion against penalising transfer STEMI programmes that exceed 120-minute reperfusion times should be considered closely in the context of the delay aetiology. The results of the STREAM trial seem to support an ongoing transfer for primary PCI strategy in this situation as much as they support the alternative of a pharmacoinvasive approach8. A focus on enhancements of pre-hospital triage and pre-hospital algorithms via high-volume heart attack centres is likely to be more critical than limitations of space or volume. Clinicians will continue to employ leaps of faith in the “grey areas” of STEMI care as they enhance their primary PCI programmes to meet the needs of their region. With those leaps of faith, there must be a commitment of those who rebel against the time-space rules to ongoing analysis of STEMI programme metrics to ensure that patient needs are being met with quality and consistency.
Conflict of interest statement
H. Dauerman is a consultant for Medtronic and has received research grants from Abbott Vascular and Medtronic.