Abstract
Aims: Timely reperfusion with primary percutaneous coronary intervention (pPCI) in ST-segment elevation myocardial infarction (STEMI) patients is associated with superior clinical outcomes. Aiming to reduce ischaemic time, an innovative system for home-to-hospital (H2H) time monitoring was implemented, which enabled real-time evaluation of ischaemic time intervals, regular feedback and improvements in the logistic chain. The objective of this study was to assess the results after implementation of the H2H dashboard for monitoring and evaluation of ischaemic time in STEMI patients.
Methods and results: Ischaemic time in STEMI patients transported by emergency medical services (EMS) and treated with pPCI in the Noordwest Ziekenhuis, Alkmaar before (2008-2009; n=495) and after the implementation of the H2H dashboard (2011-2014; n=441) was compared. Median time intervals were significantly shorter in the H2H group (door-to-balloon time 32 [IQR 25-43] vs. 40 [IQR 28-55] minutes, p-value <0.001, FMC-to-balloon time 62 [IQR 52-75] vs. 80 [IQR 67-103] minutes, p-value <0.001, and treatment delay 142 [IQR 103-221] vs. 159 [IQR 123-253] minutes, p-value <0.001). The H2H time dashboard was independently associated with shorter time delays.
Conclusions: Real-time monitoring and feedback on time delay with the H2H dashboard improves the logistic chain in STEMI patients, resulting in shorter ischaemic time intervals.
Abbreviations
CI: confidence interval
ECG: electrocardiogram
EMS: emergency medical services
ESC: European Society of Cardiology
FMC: first medical contact
GP: general practitioner
H2H: home-to-hospital
IQR: interquartile range
LBBB: left bundle branch block
NVVC: Netherlands Society of Cardiology
NWZ: Noordwest Ziekenhuis
OHCA: out-of-hospital cardiac arrest
pPCI: primary percutaneous coronary intervention
SD: standard deviation
STEMI: ST-segment elevation myocardial infarction
Introduction
Timely reperfusion therapy in patients with ST-segment elevation myocardial infarction (STEMI) is associated with superior clinical outcomes regarding morbidity and mortality1-5. Treatment with primary percutaneous coronary intervention (pPCI) is most beneficial if performed within two to three hours after the onset of symptoms6. Recent guidelines recommend a first medical contact (FMC) to balloon time of ≤90 minutes for pPCI7. A significant reduction in ischaemic time has been achieved with the implementation of pre-hospital triage and transmission of 12-lead electrocardiogram (ECG) recording to the PCI centre. The reduction in ischaemic time has resulted in a decline in mortality rates during the last decade8-16. Despite these developments, recent studies call for improvement in guideline adherence to reduce ischaemic time delays further17-19. Therefore, approaches involving awareness of time delay and building regional networks of STEMI care are needed.
The Netherlands Society of Cardiology (NVVC) initiated the Connect-STEMI programme to optimise regional collaboration from general practitioner (GP) to pPCI centre. One of the prime initiatives was transparency on ischaemic time intervals. This resulted in the development of an innovative system for monitoring the home-to-hospital (H2H) time in cooperation with emergency medical services (EMS). Additionally, a methodology of feedback to all involved care providers was concurrently initialised. The purpose of this study was to assess the effect of monitoring, evaluation and providing feedback with the H2H dashboard on ischaemic time in STEMI patients.
Methods
Retrospectively, all patients with a STEMI diagnosis treated with pPCI and transferred by EMS Noord-Holland Noord (population served 450,000) to the regional STEMI department of the Noordwest Ziekenhuis (NWZ) were included for analysis. Ischaemic time was compared between STEMI patients treated with pPCI and transported by EMS from January 2008 until December 2009 before the implementation of the H2H dashboard and STEMI patients treated after the implementation of the H2H dashboard from January 2012 until October 2014. Patients treated in 2010 and 2011 were excluded since the H2H dashboard was implemented during this period.
STEMI was defined as ongoing chest pain (>30 minutes), together with electrocardiographic ST-elevation (≥0.2 mV in ≥2 leads in V1-V3 or ≥0.1 mV in other leads) or presumed new left bundle branch block (LBBB) and a typical rise and fall of cardiac biomarkers. Patients with unclear symptom onset or subacute infarction (symptoms ≥12 hours) were excluded. In case of out-of-hospital cardiac arrest (OHCA), only patients with return of spontaneous circulation at the moment of arrival at the catheterisation laboratory were included. Finally, patients with incorrect time measurements in the H2H group were excluded.
Both patients in the historic group and those in the H2H group were treated according to the same protocol. Pre-hospital protocols included triage by 12-lead electrocardiographic findings in the field, transferred to the operator on call. Patients were treated in the ambulance with aspirin, intravenous heparin bolus, and a loading dose of clopidogrel. Glycoprotein IIb/IIIa inhibitors were administered periprocedurally in patients without contraindications. On arrival at the hospital, patients were transferred as soon as possible to the catheterisation laboratory. Haemodynamically unstable and intubated patients were first presented at the emergency department to optimise their medical condition prior to pPCI. Procedures were performed according to current international guidelines.
Time points were defined according to the European Society of Cardiology (ESC) guidelines7 (Figure 1). Patient delay was specified as the time interval from the onset of symptoms until the emergency service number was dialled. Call-to-balloon time was defined as the time between call to EMS and time of first reperfusion of the culprit artery and contains all time intervals of system delay. Time from call to departure of ambulance was described as reaction time, and response time as the interval between the EMS call and EMS arrival on scene. Time of first ECG with signs of transmural ischaemia was defined as FMC. Time from call to arrival on scene and the transfer of the patient to the PCI centre were described as transport intervals. The period after arrival at the PCI centre was divided into transmission time, door-to-needle time and needle-to-balloon time. The “door” time point was specified as the time of arrival at the PCI centre. Needle time was marked as the time of intravascular access, and balloon time that of the first intracoronary balloon inflation or reperfusion obtained by another device.
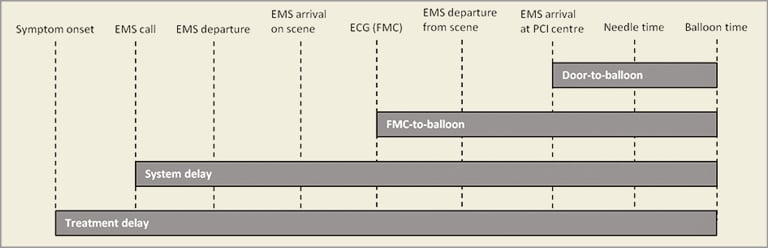
Figure 1. Delay from symptom onset to first balloon inflation in STEMI patients transported by EMS and treated with pPCI. EMS: emergency medical services; FMC: first medical contact; pPCI: primary percutaneous coronary intervention
For the present study, an overview of ischaemic time intervals was made and guideline adherence was assessed. The target time for treatment delay was 150 minutes, since pPCI is recommended to be performed within two to three hours after onset of symptoms. For call-to-balloon time, the target time was 120 minutes, for FMC-to-balloon 90 minutes and for door-to-balloon time 60 minutes. Response target time of the EMS was set at 15 minutes.
In the historic cohort, all time points were collected manually and no feedback on target time was given. The H2H dashboard collected all time points from EMS call to reperfusion of the culprit artery during pPCI in STEMI patients. Ambulance staff use buttons in the ambulance to register time points, which are assembled in an EMS database. Time points in the PCI centre are assessed by catheterisation laboratory nurses and imported into the electronic patient file. The H2H dashboard automatically merges both EMS and PCI centre data on time points, providing an overview of all time intervals of total call-to-balloon time (Figure 2). The dashboard (Active Professionals P.L.C., Rotterdam, the Netherlands) is maintained by a data manager of the EMS and the Cardiology Department of the NWZ. This enables both the Cardiology Department and the EMS to evaluate all ischaemic time intervals carefully. As a result, several improvements in logistics were made in the period in which the H2H dashboard was implemented in 2010 and 2011. At arrival at a patient with chest pain, an ECG was immediately carried out instead of their first taking an anamnesis. In addition, sterile equipment was prepared before the arrival of the patient at the catheterisation laboratory. Furthermore, all outliers were discussed and training on diagnosis was provided repeatedly.
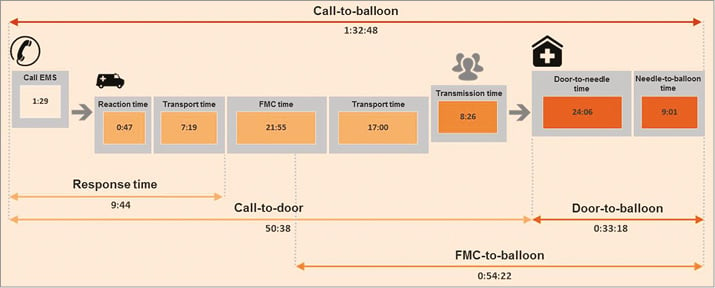
Figure 2. Example of H2H dashboard.
The primary endpoint was time delay.
STATISTICAL ANALYSIS
Continuous data are presented as mean with standard deviation or as median with interquartile range. The Student’s t-test for means and the Mann-Whitney U test for medians were used for comparing groups. Categorical variables were expressed as counts with percentages and compared with Pearson’s chi-square test. Univariable and multivariable linear regression on log-transformed door-to-balloon time, FMC-to-balloon time and treatment delay was performed to test the relation between the use of the H2H time monitoring dashboard and ischaemic time intervals. The number of cardiovascular risk factors (hypertension, hypercholesterolaemia, current smoking, family history of cardiovascular disease, and/or diabetes) was used as a continuous covariate in the linear regression analysis. All statistical tests were performed with SPSS software, Version 22.0 (IBM Corp., Armonk, NY, USA). P-values <0.05 assessed by two-sided tests were considered to be statistically significant.
Results
A total of 441 STEMI patients were transported by EMS to the NWZ and treated with pPCI after the implementation of the H2H dashboard. The historic control cohort consisted of 495 STEMI patients. The two groups were comparable with respect to age and sex. More patients with cardiogenic shock were treated with pPCI in the H2H group. In addition, more patients with OHCA were present in the H2H group (20% H2H group vs. 9% historical group, p-value <0.001) (Table 1). Analysis of ischaemic time in the historic cohort shows that over time no improvements were made, since the slope of the regression lines over time was not significantly different from zero (door-to-balloon Beta 0.00 [–0.04;0.04], p-value=0.990, FMC-to-balloon Beta –0.04 [–0.09;0.00], p-value=0.061, treatment delay Beta –0.01 [–0.10;0.07], p-value=0.785) (Figure 3).
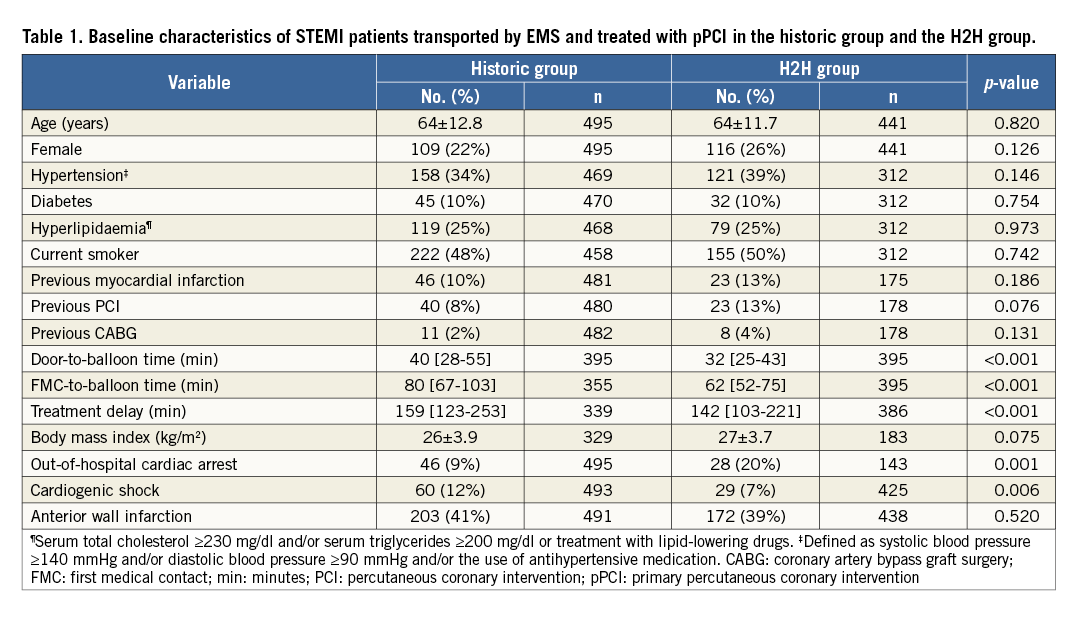
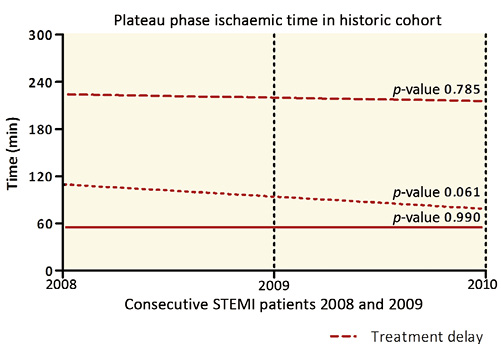
Figure 3. Plateau phase of ischaemic time intervals in 2008 and 2009. FMC: first medical contact
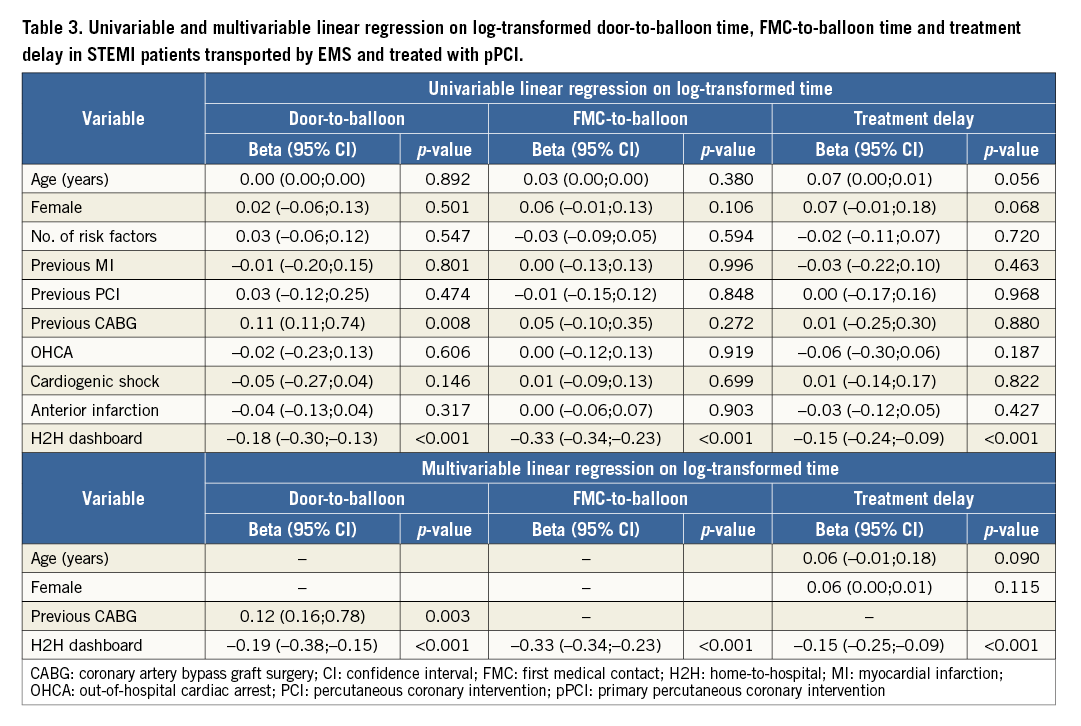
An overview of the call-to-balloon time intervals as collected by the H2H dashboard is given in Table 2. Call-to-balloon time was 79 minutes (IQR 69-90 minutes). Median treatment delay was 142 minutes (IQR 103-221 minutes). In 98% of all cases the call-to-scene target time of 15 minutes was achieved. Approximately 90% of the patients achieved the recommended door-to-balloon time of 60 minutes, 89% the recommended FMC-balloon time of 90 minutes and 93% the recommended call-to-balloon time of 120 minutes. Compared with the recommended time interval of two to three hours in the ESC guidelines, 55% of the patients had a treatment delay <150 minutes. All median ischaemic time intervals were significantly shorter in the H2H group in comparison with the historic cohort (door-to-balloon time 32 minutes [IQR 25-43 minutes] vs. 40 minutes [IQR 28-55 minutes], p-value <0.001, FMC-to-balloon time 62 minutes [IQR 52-75 minutes] vs. 80 minutes [IQR 67-103 minutes], p-value <0.001, and treatment delay 142 minutes [IQR 103-221 minutes] vs. 159 minutes [IQR 123-253 minutes], p-value <0.001) (Figure 4). Univariable linear regression on log-transformed door-to-balloon time, FMC-to-balloon time and treatment delay showed that the use of the H2H time monitoring dashboard was associated with shorter time delays. After adjusting for baseline characteristics, the H2H dashboard was independently associated with shorter door-to-balloon time (Beta –0.19 [–0.38;–0.15], p-value <0.001), shorter FMC-to-balloon time (Beta –0.33 [–0.34;–0.23], p-value <0.001), and shorter treatment delay (Beta –0.15 [–0.25;–0.09], p-value <0.001) (Table 3).
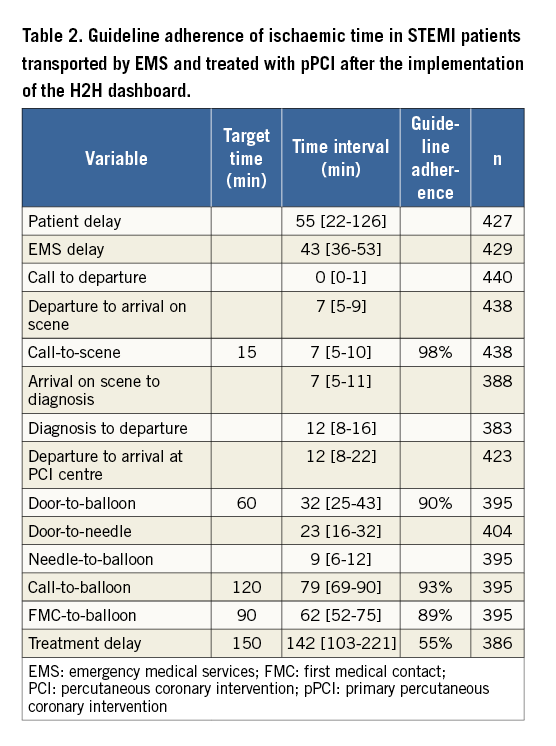
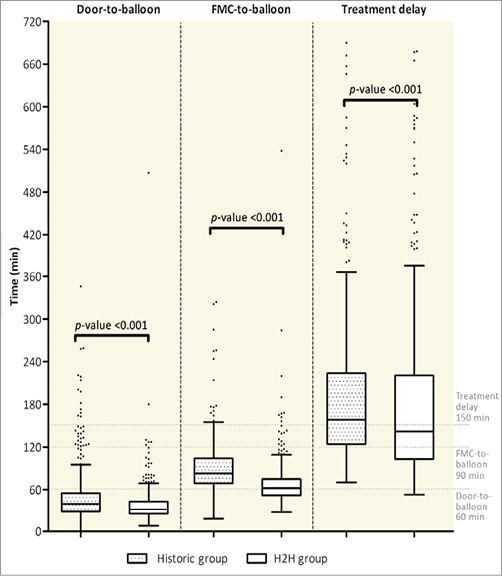
Figure 4. Door-to-balloon time, FMC-to-balloon and treatment delay in STEMI patients transported by EMS and treated with pPCI in the historic cohort and after the implementation of the H2H dashboard. FMC: first medical contact
Discussion
The key findings of this study were: 1) close monitoring and feedback on time delay with the H2H dashboard resulted in shorter ischaemic time intervals, and use of the H2H dashboard was independently associated with shorter ischaemic time delay, and 2) ischaemic target times as proposed by European guidelines were reached in approximately 90% of the cases, with the exception of treatment delay.
In the past decade, a number of strategies have been proposed to reduce treatment delays in STEMI patients. The use of pre-hospital triage, ECG recording by EMS and direct transfer to PCI-capable centres and immediate activation of catheterisation laboratory staff resulted in major improvements in ischaemic time8-13. This has resulted in lower short- and long-term mortality and morbidity rates14-16. The main focus of the H2H programme was: 1) to monitor time delay from EMS activation to reperfusion of the culprit vessel, 2) to improve accurate registration in the electronic patient file, and 3) to allow regular feedback to healthcare personnel to evaluate performance on a continuous basis. The literature shows that feedback mechanisms on time delay may be effective. Tödt et al20 were successful in reducing ischaemic time in STEMI patients by identification, evaluation and reorganisation of the process from FMC to balloon. In the pre-intervention phase, they actively observed time delay in patients. This led on to the intervention phase, where education, ECG evaluation, feedback, prioritising of ECG recording by EMS and starting the PCI procedure as soon as possible resulted in a significantly shorter time delay. In 2005, Bradley et al21 interviewed staff at 11 hospitals with shortest door-to-balloon times: a total of eight themes were identified contributing to short in-hospital time delays. One of the factors was data feedback to monitor progress and identify problems and successes. Bradley et al22 later found that efficient logistics and real-time feedback to staff in the emergency department and catheterisation laboratory were strategies associated with short door-to-balloon times.
In line with these studies, the current study showed that implementing a dashboard enabling close monitoring, evaluation and feedback can result in a significant reduction of ischaemic time. All components of time delays were shorter after the implementation of the H2H dashboard, including treatment delay, FMC-to-balloon time and door-to-balloon time. Guideline adherence was, however, only 55% for the treatment delay target time of 150 minutes. This might be due to the fact that in 50% of the cases the encountered patient delay was more than 55 minutes. For all other target time intervals guideline adherence was approximately 90%. In comparison, Helve et al17 found poorer guideline adherence: only 25% of patients had a FMC-to-balloon time of less than 90 minutes and 62.8% a door-to-balloon time of less than 60 minutes.
Median total treatment delay in other studies varied from 165 minutes to 203 minutes23-25. However, Spencer et al26 demonstrated that the geographical situation has to be taken into account when time intervals are compared between studies. The surface area of the Netherlands is approximately 41,500 square kilometres with 30 pPCI centres. The NVVC Connect Initiative developed regional care tracks in an efficient manner so that the EMS have to travel as short a distance as possible to reach a pPCI centre. In a Danish study where in-hospital data were linked with EMS data by Schoos et al27, the time delay was stratified per geographic zone (0-25 km, 65-100 km and 100-185 km). Treatment delay in comparable geographical zones (zone 1:135 minutes) was similar to the results of the present study (142 minutes). FMC-to-balloon time (zone 1:79 minutes) was shorter in the present study (62 minutes), which mainly indicates differences in either patient delay or response time of the EMS.
In other studies, median door-to-balloon time ranged from 30 to 81 minutes24. Compared with these results, the door-to-balloon time after the implementation of the H2H dashboard (32 minutes) was similar to the shortest times reported in the literature. Menees et al, in the period 2005-2009, demonstrated a reduction in door-to-balloon times retrieved from a national database in the USA28. Median door-to-balloon time in 2009 was 67 minutes and 83.1% had a door-to-balloon time under 90 minutes. Since practice makes perfect, a certain improvement can be expected over time. However, our data suggest that time improvements are limited if not closely evaluated, since no improvements were made in time delay in the period before implementation of the H2H dashboard.
Though significant reduction in time delay was observed after the implementation of the H2H dashboard, no independent association was found with short-term mortality. This might be due to either a limited sample size, or the fact that, if time delay is minimised, differences in outcome measure are more subtle. Previous studies that found associations between ischaemic time and mortality often had long ischaemic time in the reference population, whereas the ischaemic time in our historic cohort was already relatively short2,5. Outcome parameters such as infarct size or pre-discharge ejection fraction of <30% prove to be more sensitive when short time delays are compared1,3. This indicates that, if institutions already have a good working STEMI network with short transportation times, the impact of using the H2H dashboard on short-term mortality may be marginal.
Limitations
The present study has some limitations. Time points are automatically collected with the H2H dashboard in contrast to the manually retrospectively assessed time points in the group before the implementation of the H2H dashboard. However, the manner of time measurement only differs for the “door” time point, which was estimated by the catheterisation lab nurse in the historic group, which might have led to an underestimation or overestimation of the door-to-balloon time in the historic group. In addition, there were no data on the number of transferred patients from other (non-PCI) centres in the historic cohort. In the H2H group, this was approximately 4%. However, it is not expected that there were differences between the groups in transference rates, since no protocol changes were implemented. Finally, the focus of the H2H dashboard is on system delay, while patient delay composes a large part of treatment delay. Future initiatives and research on increasing public awareness might reduce treatment time even more29,30.
Conclusions
In conclusion, this study emphasises the importance of monitoring, evaluation and providing feedback on ischaemic time delays in STEMI patients. By implementing a system that automatically collects time intervals, little effort has to be made to enable evaluation. Outliers can easily be identified and discussed with all team members in order to make improvements where needed. A similar monitoring system might be helpful for other pPCI centres in order to achieve target times and a reduction of time delay. As a performance indicator for monitoring systems, total call-to-balloon time can be proposed, since it incorporates the complete logistic chain in STEMI patients and its components are well defined.
Real-time monitoring and feedback on time delay with the H2H dashboard improves the logistic chain in STEMI patients, resulting in shorter ischaemic time intervals. This study emphasises the importance of well-defined performance indicators and active management of STEMI care.
| Impact on daily practice This study emphasises the importance of monitoring, evaluation and providing feedback on ischaemic time delays in STEMI patients. Outliers can easily be identified and discussed with all team members in order to make improvements where needed. The present study showed that real-time monitoring and feedback on time delay with the H2H dashboard improves the logistic chain in STEMI patients, resulting in shorter ischaemic time intervals. A similar monitoring system might be helpful for other pPCI centres in order to achieve target times and a reduction of time delay. |
Funding
The Department of Cardiology received research grants from Biotronik, Medtronic, Boston Scientific, BMS Medical Imaging, Edwards Lifesciences, St. Jude Medical and GE Healthcare.
Conflict of interest statement
The authors have no conflicts of interest to declare.