Abstract
Early reperfusion of the occluded artery is the mainstay of the treatment of ST-segment elevation myocardial infarction (STEMI), and the best way to coordinate the resources to deliver optimal care as soon as possible is through STEMI networks. Coordination of the healthcare system is the responsibility of each of the 17 different autonomous communities in Spain. Since 2002, when the first STEMI network in Spain was established, six other communities have developed regional networks, covering 39% of the population in Spain. In the autonomous communities, after implementing an intervention model, an improvement in the reperfusion times with an increase in the number of primary percutaneous coronary interventions has been observed. This optimisation of the system has resulted in a decrease in the mortality rate among STEMI patients treated in Spanish communities with a STEMI network. Despite the encouraging advances, the challenge remains of assuring equity of treatment for all of our patients regardless of their region of residence.
Introduction
Early reperfusion of the occluded artery is the mainstay of the treatment of ST-segment elevation myocardial infarction (STEMI). Primary percutaneous coronary intervention (p-PCI) is the preferred therapy, with a Class IA indication in the European Society of Cardiology guidelines1. The objective of a STEMI network is to coordinate the resources, to deliver the best care as soon as possible and therefore to diminish the mortality among STEMI patients. Lack of organised p-PCI networks is associated with fewer patients receiving some form of reperfusion therapy2. Countries preparing to start STEMI networks can set up their goals based on the experiences of other programmes3. The aim of this review is to summarise the different models of STEMI networks currently available in Spain in order to help other physicians and politicians in their decisions on developing new networks.
Current situation of STEMI treatment in Spain
Spain is divided into 17 different autonomous communities. Coordination and management of the healthcare system is the responsibility of each community government. In 2002 the first STEMI network in Spain was established. Since then, the number of people covered by STEMI networks has slowly increased. With the advent of the last two networks, created under the auspices of Stent for Life Spain, the population currently covered by STEMI networks reached 39% of the entire country. To date, seven autonomous communities have a fully developed STEMI programme at a community level with data on at least one year of outcome.
In 2010, according to the National Institute of Statistics4, 59,165 patients were admitted to hospital with a diagnosis of acute myocardial infarction, and of those 19,437 died (most of them prior to reaching hospital). According to a recent registry, 38% of patients admitted to hospital with a diagnosis of acute myocardial infarction suffered from a STEMI5. With these data, we were able to estimate an annual incidence of 44 STEMI patients admitted to hospital per 100,000 people in Spain. However, recent unpublished data (Marrugat et al, personal communication) roughly estimated a rate of nearer 70 STEMI patients per 100,000 people in Spain. Primary PCI rates can be influenced by a lower incidence of the disease, and the lack of a STEMI national registry means these figures are only estimates. According to the registry of the Interventional Cardiology Working Group of the Spanish Society of Cardiology, 64,331 PCIs were performed during 2010. Of these, 14,248 (22.1%) were PCI for STEMI patients and 10,339 (72.6%) were p-PCI. Overall, the mean rate of p-PCI per million inhabitants was 219 in 2010, with an inhomogeneous distribution among different regions (Figure 1). Overall, regions with STEMI networks presented higher rates of p-PCI as compared to those without networks (158.98 vs. 324.12, p<0.001) (Figure 1) despite similar figures in overall PCI (1376.58 vs. 1254.6, p=0.81) (Figure 2).
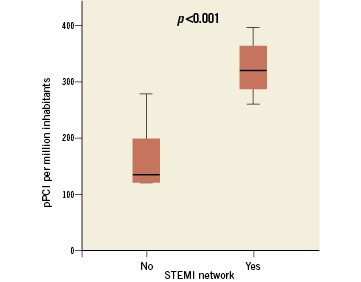
Figure 1. Comparison of p-PCI between communities with and without STEMI network.
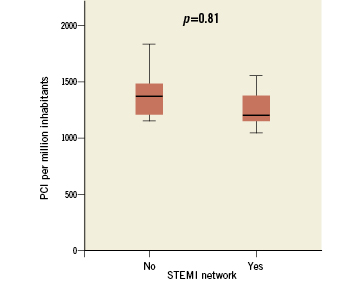
Figure 2. Comparison of PCI between regions with and without STEMI network.
MODEL OF INTERVENTION IN CATALONIA: CODI INFART CATALUNYA
Catalonia has a population of 7,529,618 inhabitants in 32,113 km2. The territory is divided into seven health regions. The most populated region is located in Barcelona and its metropolitan area. In 2010, myocardial infarction was the main cause of death in Catalonia, with 2,288 deaths. In 2004, the Catalan Society of Cardiology together with the Health Department designed a model of intervention with p-PCI for the patient with persistent STEMI living in the metropolitan area of Barcelona. Patients with less than three hours of symptoms and with an expected first medical contact to balloon time of less than 90 minutes were treated with p-PCI. However, the overall number of patients treated with p-PCI did not increase. In October 2007, the Catalan Society of Cardiology communicated directly to the Health Department of Catalonia that there was a need for a new model of intervention which would cover the entire autonomous community. A new task force was then constituted by the Catalan Society of Cardiology, the Emergency Medical System and Government representatives. This task force finally published the “Codi Infart Catalunya” binding act on May 12th, 2009.
The model is based on the following characteristics:
– It is addressed to all STEMI patients
– The clinical protocol is based on the European Society of Cardiology guidelines
– It eliminates barriers from the first medical contact to revascularisation by giving EMS and emergency room staff the power to activate the code
– Total coverage of the Catalonia territory with assistance divided among hospitals, p-PCI available 24/7, and EMS having a central role
– Obligatory return to referral hospital once the patient is stable
– Obligatory registry of data
Catalonia has 10 public p-PCI hospital centres, five of them with 24/7 service located in the Barcelona metropolitan area. During working hours all 10 p-PCI hospitals are part of the network. Overnight and during weekends the network comprises five centres with 24/7 service. A single Emergency Medical System (EMS) covers the whole territory.
All personnel capable of obtaining and reading an ECG are able to activate the STEMI code. After identifying a STEMI patient, EMS or medical staff select the reperfusion therapy by following an established protocol which takes into account the duration of symptoms and the estimated transport times. Two helicopters are accessible in case of need. Out-of-hospital thrombolysis is available for patients with an estimated first medical contact to p-PCI centre transport time of more than 90 minutes; otherwise, patients are treated with p-PCI. In the case of p-PCI, an EMS operator contacts the p-PCI centre personnel and the patient is transported directly to the cathlab.
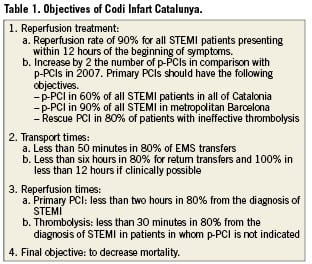
Codi Infart objectives are summarised in Table 1.
In 2010, 2,884 codes were activated; of these 2,181 (75.6%) patients had a discharge diagnosis of STEMI and in 2,121 PCIs were performed. A total of 1,834 (84.1%) p-PCIs with a rate of 281.1 p-PCIs per million inhabitants were performed. In addition, 256 patients were admitted directly to the p-PCI centre without any code activation. As a result, the rate of PCI in Catalonia reached 315.3 per million inhabitants. Furthermore, 194 patients received thrombolytic therapy (45.8% out-of-hospital) and among them 74 (38.1%) were treated with rescue PCI.
In 83.5% of patients, transport to a PCI centre was by ambulance. Of these, primary EMS transfer (from home to cathlab) was carried out in 1,406 (48.5%) patients. The rest are accounted for by inter-hospital transfer.
The mean time between symptoms onset to first medical contact (FMC) was 80 minutes. This was reduced to 60 minutes for patients in whom the FMC was performed directly by the EMS. The mean time between FMC to PCI was 90 minutes and FMC to needle was 46 minutes.
Total hospital mortality was 3.1%, but 4.1% in patients who received thrombolytic therapy. Only 60 (2.75%) patients did not receive any reperfusion therapy with a mortality of 16.6%.
NAVARRA
The first STEMI patient treated with angioplasty in Navarra was in 1991. Since then, there has been a continuous drive to consolidate an intervention model and this was started formally in 2002. Navarra is a community with 10,391 km2 and 624,054 inhabitants. A PCI centre and three referring hospitals constitute the STEMI network. A pharmaco-invasive strategy is chosen for patients with an estimated transfer time to PCI centre of more than two hours, with administration of thrombolytic and further referral to the PCI centre. Based on that model the rate of PCI per million inhabitants is 415.77, and 79.4% of STEMI patients are treated with p-PCI with a mortality at 30 days of 3.78%8.
MURCIA
Murcia is a community with 11,314 km2 and 1,470,069 inhabitants. The STEMI network is composed of one PCI centre with 24/7 availability and 10 other secondary hospitals within one hour of transfer time to the PCI centre. Murcia´s intervention model (APRIMUR) was created in February 2000 and achieved total community coverage in 2001. Reperfusion strategy depends on the duration of symptoms. If the patient presents with less than three hours of chest pain and the estimated transfer time to the PCI centre is more than 90 minutes, thrombolytic therapy is administered before the patient is referred to the PCI centre. Otherwise, the patient will be treated initially with p-PCI. In 2010, 380 PCIs were performed with a rate of 282 PCIs per million inhabitants7. After the establishment of APRIMUR the in-hospital mortality decreased from 14.6% in 2000 to 6.6% in 20099.
BALEARIC ISLANDS
The Balearic Islands comprise five different islands with a total population of 1,113,114 inhabitants and a surface area of 4.992 km2. In March 2008 the STEMI network was created. In selecting the most suitable reperfusion therapy, the model takes into account the time duration of symptoms and the availability of resources. The final responsibility for selection of the reperfusion therapy rests with the interventional cardiologist, with an ECG transmitted by telemetry. A total of 1,298 patients have been treated in a 21-month period. 56.7% were treated with p-PCI and 26.1% with thrombolytic therapy. Of these, 60% of patients were finally referred to secondary PCI. Overall, 68% of patients were treated with p-PCI resulting in a rate of 265 p-PCIs per million inhabitants. In-hospital mortality had dropped from 21% in 2001 to 7.36% by the end of 2010.
GALICIA
Galicia had four 24/7 PCI centres and a rate of 307 p-PCIs per million inhabitants before the development of the STEMI network. However, due to the geographical peculiarities of the region a coordinated approach to cover the entire community was needed. The current network (PROGALIAM) has demonstrated its ability to treat 92% of the population in Galicia by p-PCI within 90 minutes and 99% within 120 minutes from the first medical contact. This new programme increased the rate of p-PCIs to 354 per million inhabitants7 and decreased the mean door-to-balloon time from 126 to 99 min.
CASTILLA LA MANCHA
Castilla La Mancha had four PCI centres and a rate of 142 p-PCIs per million inhabitants before the implementation of the “CORECAM” STEMI network. After one year of implementation the region increased the rate of reperfusion to 346 p-PCIs per million inhabitants7. This success is related to the coverage of the entire community either by ambulances or by helicopters able to fly overnight.
Conclusion
The development of models of intervention for the treatment of STEMI patients resulted in a decrease of reperfusion times in parallel to an increase in the rate of p-PCI. In addition, STEMI networks have allowed us to perform a quality control in a country that otherwise did not have any type of STEMI registry at a national level. The development of these networks was made possible by the combined efforts of medical societies, emergency medical systems, cardiologists and physicians working in acute cardiac care units and ambulances, and the dedicated support of local governments. Despite the encouraging advances made in recent years, we still have the tremendous challenge of assuring equity of treatment for all of our patients regardless of their region of residence.
Conflict of interest statement
The authors have no conflicts of interest to declare.