Abstract
Aims: In patients with ST-segment elevation myocardial infarction (STEMI), timely reperfusion with primary percutaneous coronary intervention (PPCI) is the preferred treatment. However, it remains unclear whether the optimal strategy is complete revascularisation or culprit vessel PPCI only.
Methods and results: From January 2002 to June 2009 all patients treated with PPCI were identified from the Western Denmark Heart Registry. We examined mortality according to timing of multivessel PCI: acute procedure, staged procedure during the index hospitalisation, or staged procedure performed within 60 days. The hazard ratio (HR) for death was estimated using a time-dependent Cox regression model, with time of PCI for the non-culprit lesion as the time-dependent variable. The study cohort consisted of 5,944 patients, of whom 4,770 (80%) had single-vessel disease and 1,174 (20%) had multivessel PCI within 60 days. Among 354 (30.2%) patients with acute multivessel PCI, 194 (16.5%) patients with multivessel PCI during the index hospitalisation, and 626 (53.3%) patients with multivessel PCI within 60 days after the index hospitalisation, the adjusted HRs for one-year mortality were 1.53 (95% confidence interval (CI): 1.07-2.18), 0.60 (95% CI: 0.28-1.26), and 0.28 (95% CI: 0.14-0.54), respectively, compared to patients with single vessel disease.
Conclusions: Acute multivessel PCI in patients with STEMI was associated with increased mortality.
Introduction
Primary percutaneous coronary intervention (PPCI) is a well-established treatment for ST-segment elevation myocardial infarction (STEMI)1,2. In up to half of patients presenting with STEMI, multivessel coronary disease is present3-5 and has been found to be associated with worse prognosis4,6. Optimal treatment of patients with STEMI and multivessel disease is not clear. Both the European Society of Cardiology guidelines for PCI7 and the American College of Cardiology/American Heart Association guidelines for the management of patients with STEMI8 recommend acute PCI treatment of the culprit lesion. PCI of the non-culprit lesions are only recommended during the index procedure in haemodynamically compromised patients. Two randomised trials9,10 reported that multivessel treatment during PPCI was safe without increased mortality in controlled trials, but their sample sizes were too small to provide a definite answer.
A post hoc analysis of the “Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction” concluded a deferred angioplasty strategy of non-culprit lesions should remain the standard approach in patients with STEMI undergoing primary PCI, as multivessel PCI might be associated with a greater risk for mortality and stent thrombosis11. Two meta-analyses reported similar major adverse cardiovascular events and long-term mortality12,13 in STEMI patients treated either with acute complete revascularisation or with only infarct-related PPCI in the acute phase, whereas one large meta-analysis where prospective and retrospective studies were included supported current guidelines discouraging performance of multivessel primary PCI for STEMI14. The New York State PCI Registry15 reported that, in haemodynamically stable patients with multivessel disease, acute phase multivessel PCI resulted in increased mortality, compared with infarct-related PPCI only. One observational study reported lower adverse outcome rates for culprit lesion PPCI16 and another study found no significant difference17. We used data from the Western Denmark Heart Registry (WDHR) to examine differences in in-hospital and longer-term mortality for STEMI patients with multivessel disease treated with multivessel PCI compared to patients with single vessel disease (STEMI culprit lesion). Further, for patients with multivessel PCI we compared three strategies: multivessel PCI performed acutely, staged procedures during index hospitalisation, or staged procedures within 60 days after hospital discharge. We compared their outcomes to those among patients with single vessel disease.
Patients and methods
SETTING AND DESIGN
The study was conducted using Western Denmark’s healthcare databases, which cover the region’s entire population of approximately 3.0 million inhabitants (55% of the Danish population). A detailed description of the databases has been reported previously18,19.
PATIENTS AND PROCEDURES
Primary PCI became the recommended treatment for STEMI in Denmark after publication of the results of the DANish trial in Acute Myocardial Infarction-2 (DANAMI 2) 1 in 2003. To be eligible for primary PCI, patients must meet the following criteria: 1) symptoms present less than 12 hours from onset of pain to time of catheterisation, and 2) ST-segment elevation (at least 0.1 mV in two or more standard leads or at least 0.2 mV in two or more contiguous precordial leads) or a new left bundle branch block (LBBB). We used the WDHR to identify all PPCIs performed from January 1, 2002, up to June 25, 2009. For inclusion in the present study, patients had to have either single vessel disease (culprit lesion) or multivessel disease (culprit lesion+non-culprit lesion) treated with PCI either acutely, in an in-hospital staged procedure, or within 60 days after hospital discharge. In addition, the patients had to be haemodynamically stable without cardiogenic shock (Figure 1 presents the flow chart for patient selection). Patients with cardiogenic shock, a critical pre-hospital condition, anaesthesiology assistance, intubation, use of intra-aortic balloon pump, or a systolic blood pressure <90 mmHg were excluded from the analysis. PPCI was performed according to the standard practices of the participating centres. A glycoprotein IIb/IIIa receptor blocker was administered at the operator’s discretion. The post-intervention antiplatelet regimen included lifelong acetylsalicylic acid (75-150 mg once daily) and clopidogrel with a loading dose of 300 mg followed by maintenance with 75 mg daily. The recommended duration of clopidogrel treatment was 3 to 12 months until November 2002 and 12 months thereafter.
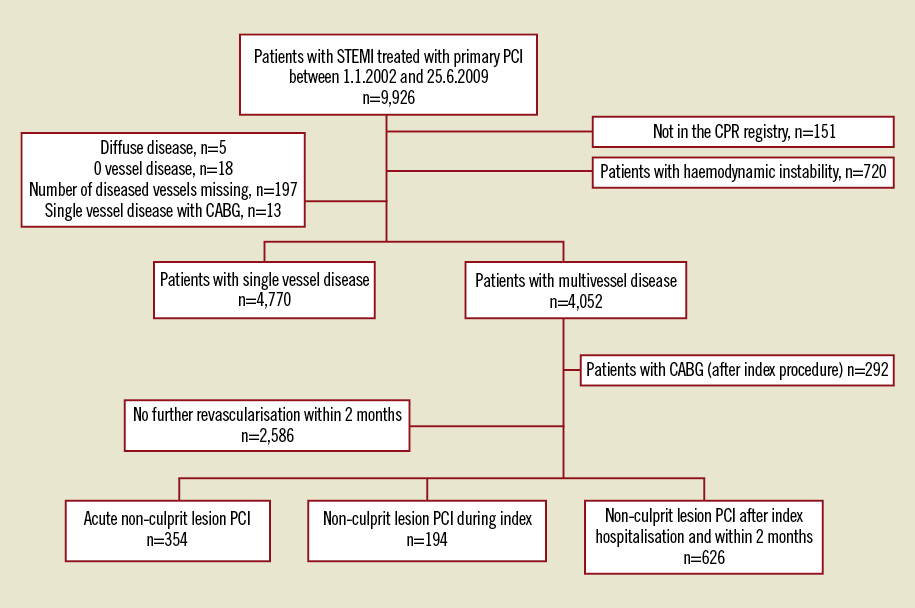
Figure 1. Trial flow diagram.
ENDPOINTS
The endpoint was time to all-cause mortality. Data on mortality were obtained from the Danish National Registry of Patients (DNRP)20, which has kept electronic records on the gender, date of birth, changes in address, date of emigration, and changes in vital status of the entire Danish population since 1968.
COVARIATES
We retrieved data from the WDHR on potential predictors for subsequent cardiovascular events, including characteristics of the patients, procedures and lesions. For each patient, we obtained data on all discharge diagnoses from the DNRP. We then computed comorbidity scores using the Charlson Comorbidity Index (CCI)21, which covers 19 major disease categories, including diabetes mellitus, heart failure, cerebrovascular diseases, and cancer. The index value is a weighted summary of the diagnoses, with each weight calculated based on one-year mortality associated with each disease in the original Charlson dataset.
STATISTICAL METHODS
Distributions of continuous variables in the group of patients with single vessel disease (culprit lesion) and the group with multivessel PCI were compared using the Kruskal-Wallis test. Distributions of categorical variables were compared using the Chi-square test.
We counted endpoint events that occurred during the follow-up period and compared rates for the two groups. Follow-up began on the date of PPCI procedure and continued until date of death, emigration, June 25, 2010, or after seven years of follow-up (to ensure at least 10% of the study population at risk), whichever came first. We constructed Kaplan-Meier curves for patients with multivessel PCI and single vessel PCI. Patients with multivessel disease PCI were stratified according to the time of the non-culprit lesion PCI (acute, staged during index hospitalisation, or performed within 60 days of hospital discharge). Cox proportional hazards regression analysis was used to estimate the hazard ratio (HR) for mortality (using single vessel disease as the reference) with time for multivessel PCI as a time-dependent variable. We used the change-in-estimate variable selection strategy to assess inclusion of potential confounders. This entailed retaining variables that changed the crude HR estimates for overall mortality by more than 10 percent22.
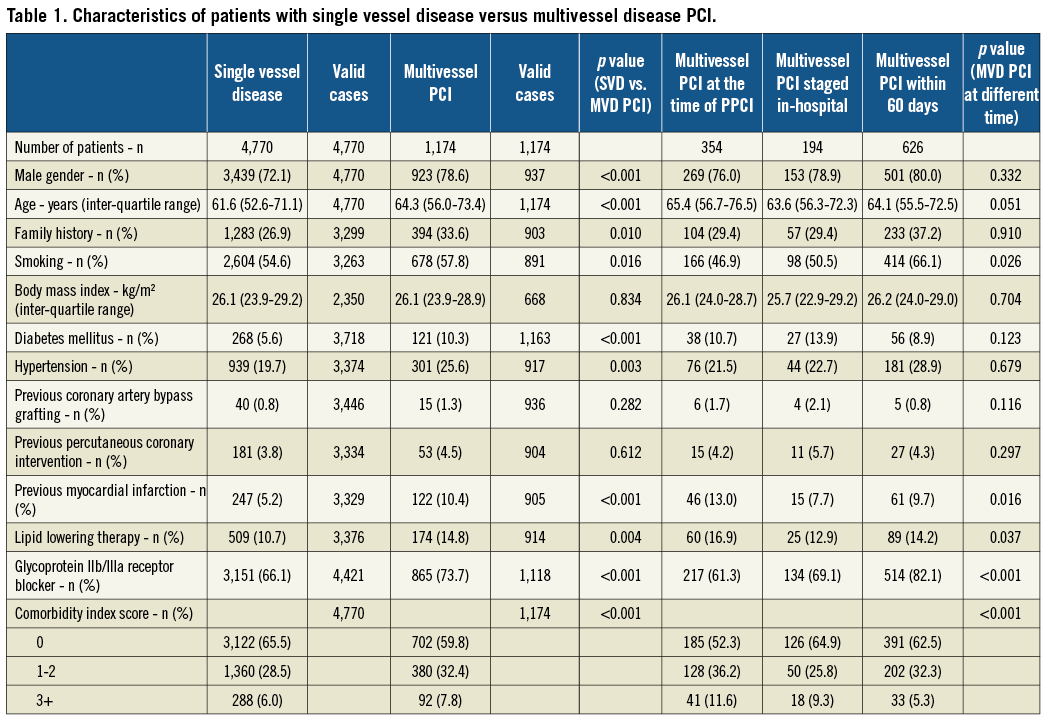
We used multiple imputation methods to impute missing covariate values23. We assessed all variables in Table 1 and Table 2 and found that only age and CCI score changed HR estimates for the mortality outcome by more than 10 percent. Thus, we adjusted only for these variables, together with gender, in the final model. All data analyses were carried out using SAS software version 9.13 (SAS Institute Inc., Cary, NC, USA).
Results
STUDY POPULATION
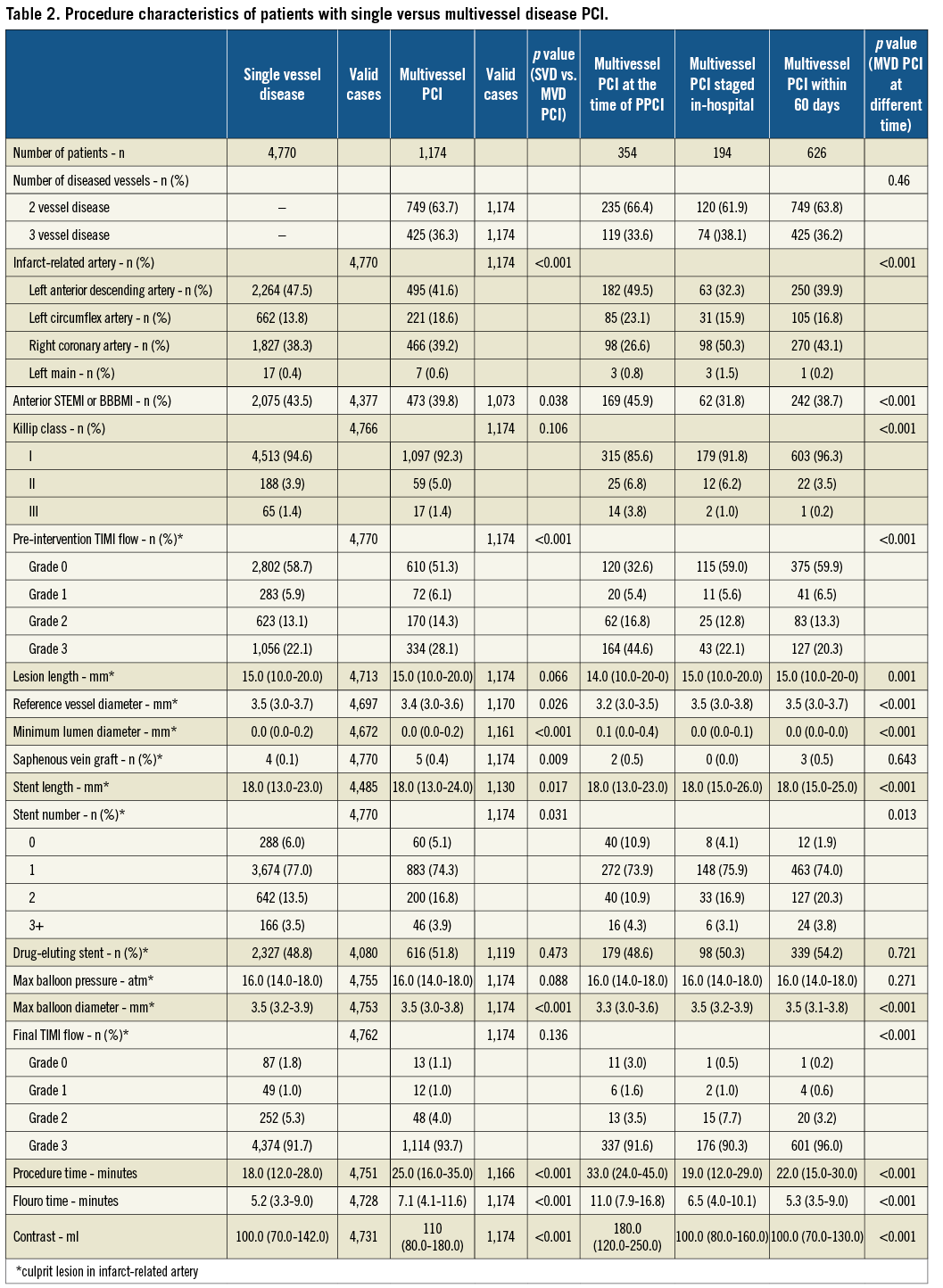
A total of 9,926 patients were treated with primary PCI for STEMI or BBBMI at one of the three participating PCI centres between January 1, 2002, and June 25, 2009. Mortality data were not available for 151 patients, who were foreign citizens or who had emigrated. Patients with haemodynamic instability or cardiogenic shock (n=720 [7.2%] patients with single vessel disease n=264 and patients with multivessel disease n=442), a coronary artery bypass operation within two months (n=292 [2.9%]) and patients with multivessel disease but without further revascularisation within 60 days (n=2,586 [26.1%]) were excluded. Thus, the final study cohort consisted of 5,944 patients, of whom 4,770 (80%) had single vessel disease PCI and 1,174 (20%) had multivessel disease PCI within 60 days. There were significant differences in several baseline characteristics, including cardiac risk factors and comorbidity, for patients with single vessel disease vs. multivessel PCI (Table 1).
MORTALITY
The median follow-up time was 3.9 years (25th-75th percentile: 2.3-5.7 years), with a one-year mortality of 4.8% (n=287) and seven-year mortality of 12.1% (n=722). Among patients with single vessel disease PCI and multivessel disease PCI, one-year cumulative mortality was 4.9% (n=235) and 4.4% (n=52), respectively; seven-year mortality was 17.4% (n=555) and 20.2% (n=157), respectively (Table 3). Among patients with multivessel, non-culprit lesion PCI performed acutely, staged during the index hospitalisation, or performed within 60 days, one-year cumulative mortality was 10.2% (n=36), 3.6% (n=7), and 1.4% (n=9), respectively; their seven-year mortality was 32.2% (n=87), 14.2% (n=22), and 15.2% (n=48), respectively (Figure 2). After adjustment for age, gender, and CCI score, overall seven-year mortality did not differ between patients with multivessel PCI and patients with single vessel disease (HR = 0.96, 95% CI: 0.80-1.14) (Table 4). Among patients with multivessel PCI, those with acute multivessel PCI had higher short-term and long-term mortality than patients with single vessel disease PCI. Mortality in patients with multivessel disease PCI and a staged procedure within the index hospitalisation was comparable to that in patients with single vessel disease PCI. Patients with multivessel disease PCI performed as a staged procedure after discharge from the index hospitalisation, but within 60 days, had lower mortality rates compared to patients with single vessel disease PCI at all-time intervals under study (Table 4). However, among patients with multivessel who were discharged, 135 patients (5.1% of patients with multivessel disease without any further revascularisation within 60 days than culprit lesion) died within 60 days, and an eventual planned revascularisation strategy was not known (Figure 3).
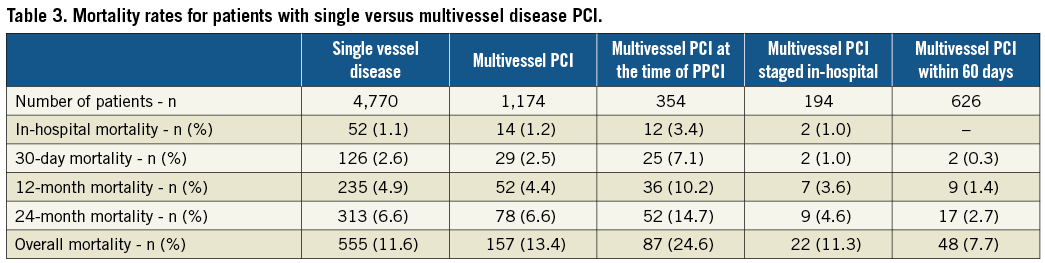
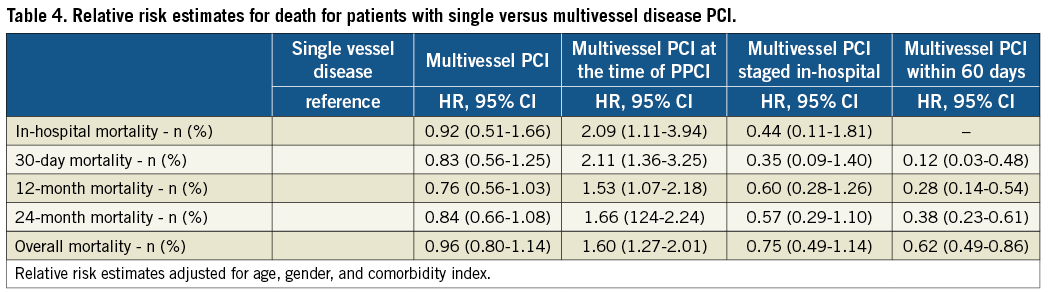
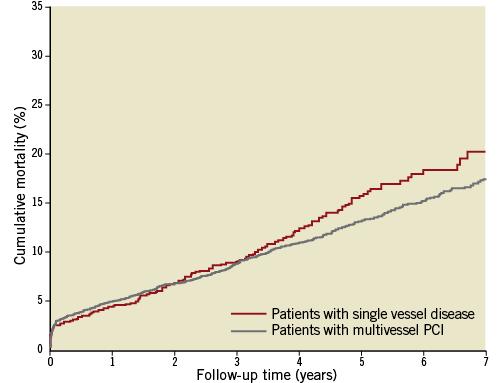
Figure 2. Time-to-event curves for all-cause mortality for patients with single vessel disease (culprit lesion only) and for patients with multivessel PCI.
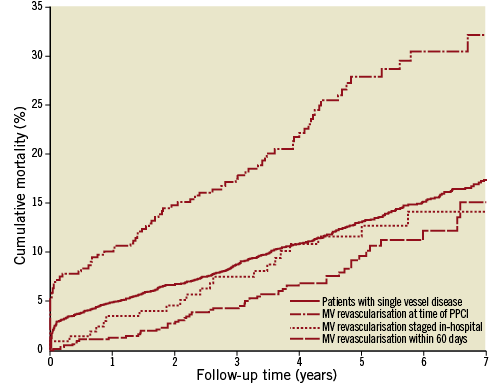
Figure 3. Time-to-event curves for all-cause mortality for patients with single vessel disease (culprit lesion only) and for patients with multivessel PCI. For patients with multivessel PCI three strategies are shown: multivessel PCI performed acutely, staged procedures during index hospitalisation, or staged procedures within 60 days after hospital discharge.
Discussion
The findings of the present study indicate that among STEMI patients treated with primary PCI in a real-world clinical setting, presence of multivessel disease treated with PCI did not increase short-term or long-term mortality rates overall. Patients with STEMI and multivessel disease undergoing complete revascularisation in the acute phase had higher short-term and long-term mortality than patients with single vessel disease and culprit lesion PCI only. However, staged multivessel PCI was found to be safe.
In patients with STEMI and acute multivessel PCI, the potential advantages of staged intervention are completeness of revascularisation and possible shortening of the cumulative hospital stay. In patients with haemodynamic instability in the acute setting there is a further clinical indication for acute complete revascularisation24,25. We found an increased mortality rate in all time intervals examined among patients with acute multivessel PCI, despite exclusion of patients with cardiogenic shock, a critical pre-hospital condition, anaesthesiology assistance, intubation, use of an intra-aortic balloon pump, or a systolic blood pressure <90 mmHg. Patients with multivessel PCI were older and had more comorbidity (especially patients with acute multivessel PPCI), compared to patients with single vessel disease and staged revascularisation procedures. Our results are in line with data from the New York State PCI Registry15, which showed that haemodynamically stable patients with multivessel PCI had a higher in-hospital mortality rate, compared to patients undergoing PCI only in the infarct-related artery. Four other studies11,14,16,26 reported similar results, with an increased rate of major adverse cardiac events in patients undergoing multivessel PCI acutely compared to PCI restricted to the infarct-affected artery. The largest registry, the National Cardiovascular Data Registry27, found that patients undergoing multivessel PCI were at higher risk and were more likely to be in cardiogenic shock. In addition, overall in-hospital mortality rates were higher in patients undergoing multivessel PCI. Similar results were found among Medicare Beneficiaries28 who underwent single vessel versus multivessel PCI during an hospitalisation.
In contrast, other studies have found that performing multivessel PCI acutely did not lead to increased mortality5,29. In the study by Varani et al5 the multivessel disease group consisted of patients with acute multivessel PCI (37%), PCI within 24 hours (12%), and PCI within 48 hours (12%); the remaining patients with multivessel disease had only culprit lesion PCI (39%), and some had haemodynamic compromise. After exclusion of patients with haemodynamic compromise upon admission, mortality differences between the subgroups of multivessel disease patients disappeared. The authors stated that a word of caution is mandatory regarding routine performance of early multivessel PCI due to the observational nature of their study and the risk of subacute stent thrombosis. When a staged procedure was used, the 30-day mortality rate was 2.1% - comparable to the 1.0% 30-day mortality rate found in our study. Our group has previously shown that in unselected STEMI patients treated with PPCI, 25% of definite stent thromboses occurred acutely within 24 hours and another 50% occurred within 30 days30. Qarawani et al29 observed similar short-term and one-year mortality rates among both patients with multivessel disease treated acutely with complete revascularisation and patients with culprit lesion PCI only. However, re-intervention was higher and hospital stay shorter in patients treated with acute multivessel PCI. Based on a small randomised study, Di Mario et al9 reported that it was safe to perform acute multivessel PCI. However, no clinical or economic advantages were obtained from the more aggressive initial approach, and the need for subsequent clinically driven revascularisation was low.
More than half of patients treated with multivessel PCI in our study underwent a more conservative procedure, with non-culprit lesion revascularisation after hospital discharge and within 60 days. This group had the lowest mortality rate at one year and at two years, as well as after the longest follow-up available. Revascularisation in this group may have been clinically driven, guided by objective evidence of residual ischaemia, or suggested by the operator during the initial procedure. Only one other study assessed the approach of a staged procedure after hospital discharge: as in the present study, the New York State PCI Registry15 found a reduced mortality rate in patients treated with a staged PCI within 60 days. Both studies suffer from selection bias, as this group of patients represents those with culprit vessel PCI who survived for up to 60 days.
These findings support the need for a large-scale randomised trial to evaluate revascularisation strategies in patients with STEMI and multivessel disease.
Limitations
The validity of our findings depends on data quality and the ability to control for potential confounding. Our design is based on computerised registries with complete nationwide coverage, allowing study of a well-defined, large population with complete follow-up. However, like all observational studies, our study is prone to biases related to unmeasured factors. Bias due to unknown variables cannot be eliminated.
We excluded patients with cardiogenic shock, critical pre-hospital condition, anaesthesiology assistance, intubation, use of an intra-aortic balloon pump, or a systolic blood pressure <90 mmHg. However, in some enrolled patients undergoing acute multivessel, there might have been a strong clinical indication for this aggressive approach that we were not able to identify in the WDHR, as acute multivessel PCI at the time of primary PCI was more commonly performed in patients with Killip class III, anterior STEMI (LAD as culprit lesion) and in patients where no flow could be achieved in the infarct-related coronary artery (TIMI 0). Further, the chosen strategy in patients with multivessel disease was taken by the cardiologist treating the patients (either the PCI operator or the cardiologist controlling the patients after discharge from index hospitalisation). There may have been a selection between a severe proximal lesion in the left anterior descending coronary artery and a lesion in a non-dominant circumflexus. STEMI patients who underwent non-culprit lesion PCI after hospital discharge and within 60 days represent those with multivessel disease who survived up to 60 days and those who did not develop relative contraindications to repeat PCI (such as renal failure or neurologic complications). Two thirds of patients with multivessel disease did not undergo further revascularisation within 60 days. It is important to note that we did not have access to data on left ventricle ejection fraction or medical therapies received before hospitalisation and after discharge in patients with and without multivessel disease.
Conclusion
Acute multivessel PCI in STEMI patients was associated with increased mortality compared to patients with single vessel disease. Non-culprit lesion revascularisation is safer when performed as a staged procedure.
Conflict of interest statement
The authors have no conflicts of interest to declare.

