Introduction
Percutaneous coronary intervention (PCI) of calcified coronary lesions remains a challenge in routine clinical practice. Optimal lesion preparation prior to stent implantation is essential in this lesion subset1. The randomised PREPARE-CALC (The Comparison of Strategies to PREPARE Severely CALCified Coronary Lesions) trial demonstrated superiority for a strategy of lesion preparation with rotational atherectomy (RA) prior to drug-eluting stent (DES) implantation compared to a modified balloon (MB) angioplasty strategy2. As lesion location may have an important influence on device deliverability and strategy success, the aim of this sub-analysis was to investigate the interaction between treatment effect and lesion location.
Methods
The trial design and study population have been described previously2. Briefly, PREPARE-CALC is a randomised controlled trial enrolling patients with severely calcified coronary lesions undergoing PCI. Patients were randomised 1:1 to an initial strategy of lesion preparation using RA versus MB followed by implantation of a new-generation sirolimus-eluting stent (Orsiro; Biotronik AG, Bülach, Switzerland) (Supplementary Figure 1). The primary endpoint was strategy success, defined as successful stent delivery and expansion with attainment of <20% in-stent residual stenosis of the target lesion in the presence of Thrombolysis In Myocardial Infarction (TIMI) 3 flow without crossover or stent failure. The co-primary endpoint was in-stent late lumen loss (LLL), defined as the difference between post-procedure and nine-month in-stent angiographic minimal lumen diameter.
Results
Overall, 200 patients were enrolled. A total of 93 patients had left anterior descending (LAD) lesions and 107 patients had non-LAD lesions. Baseline characteristics were well balanced across the treatment groups (Supplementary Table 1). In-hospital outcomes and nine-month angiographic follow-up results are shown in Table 1. For LAD lesions, strategy success was similar for both strategies (96.1% in the RA group vs 95.2% in the MB group; p>0.99), with a longer procedure (86.2±32.5 vs 67.3±42.8 minutes; p=0.021) and fluoroscopy time (22.3±10.8 vs 15.2±10.9 minutes; p=0.004) in the RA group. In contrast, for non-LAD lesions, strategy success was significantly more common with an RA-based strategy compared to an MB-based strategy (100% vs 70.7%; p<0.001) with comparable procedure (90.3±37.4 vs 86.7±37.3 minutes; p=0.61) and fluoroscopy time (25.5±13.5 vs 22.6±14.3 minutes; p=0.31). At nine months, mean in-stent LLL was similar for LAD and non-LAD lesions according to the lesion preparation strategy (Figure 1).
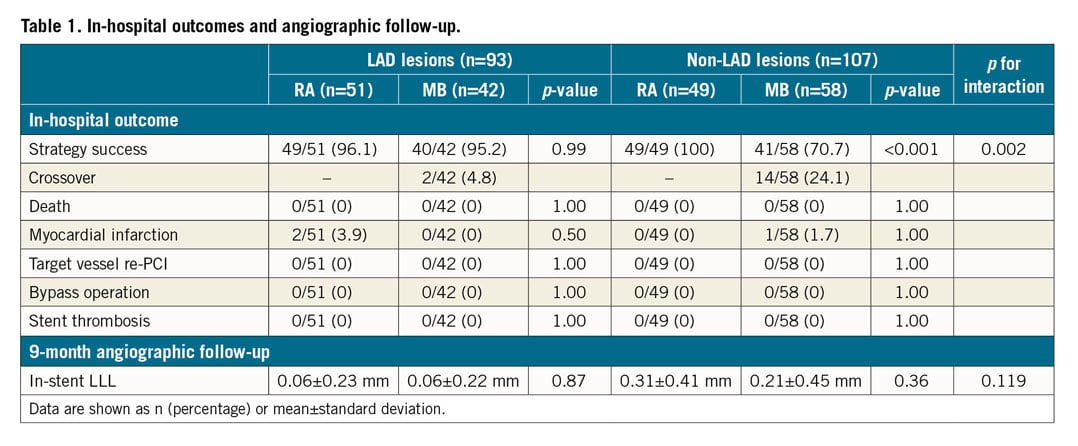
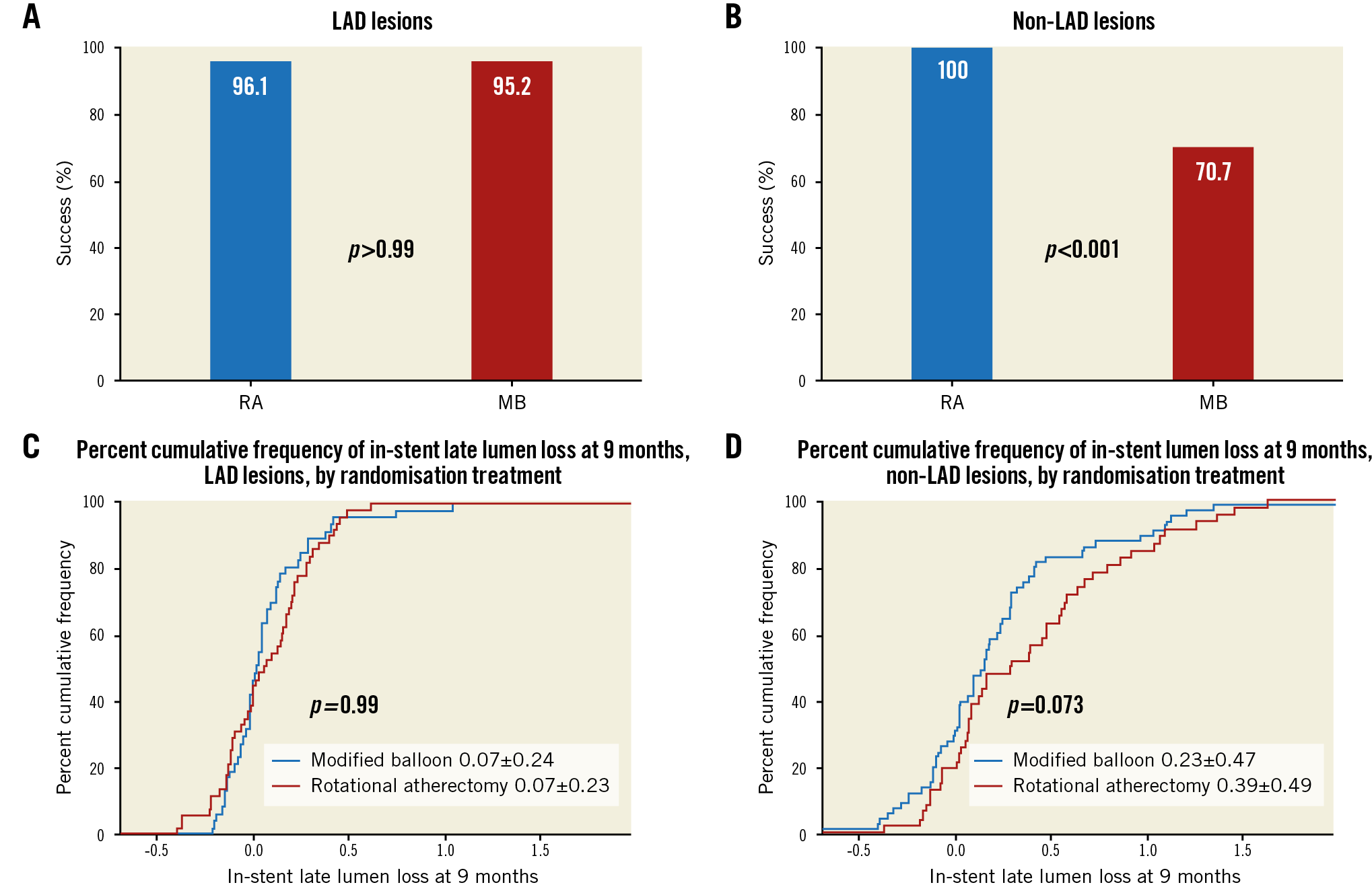
Figure 1. Strategy success (A and B) and in-stent LLL (C and D) according to lesion location.
Discussion
In patients with calcific coronary artery disease, results from the PREPARE-CALC trial demonstrated that strategy success was higher with an RA-based lesion preparation strategy compared with an MB-based strategy prior to DES implantation. This difference was mainly due to a higher frequency of crossover and stent failure in the MB group. The co-primary endpoint of in-stent LLL at nine months was comparable, and clinical outcome was excellent overall with both treatment strategies2.
To date, the impact of lesion location on the performance of different strategies for lesion preparation has not been well investigated. In this subgroup analysis, lesion preparation with either RA or MB resulted in comparable strategy success rates in LAD lesions, whereas in non-LAD lesions an upfront RA-based strategy seems to be superior. This is driven by a higher rate of crossovers in non-LAD lesions. The mean LLL was comparable for both strategies, irrespective of lesion location.
Despite iterative improvements in coronary devices and techniques, calcified lesions remain a challenging scenario in patients undergoing PCI, with elevated rates of periprocedural complications as well as long-term adverse events in comparison with non-calcified lesions. Optimal lesion preparation is arguably the critical determinant of procedural success, facilitating lesion dilatation, device delivery and stent expansion, as well as determining the long-term effectiveness of DES. As PCI of calcified lesions is complex and time-consuming, and selection of available tools may be influenced by local availability and expertise, insights from randomised trials with protocol-mandated interventions may shed light on potential differences between available strategies.
Overall, lesion preparation with upfront RA was superior to MB angioplasty in the primary analysis of the current trial2. Moreover, with current-generation DES, an RA-based strategy does not result in higher LLL, which was a limitation with older-generation devices1,2. However, the results of this subgroup analysis suggest that, in lesions located outside the LAD, a primary strategy with RA may be preferable in terms of strategy success, whereas for LAD lesions a strategy of provisional MB with bail-out RA remains feasible and effective. Although the precise reasons for the observed differences in strategy success in this open-label trial are not known, these findings might reflect constraints on the deliverability of both MB and stents in lesions located in non-LAD vessels, which tend to be more tortuous and can be associated with more limited guide catheter support. With accumulating evidence and experience in the treatment of patients with calcified coronary lesions over recent years3, these observations warrant further investigation.
Limitations
The small number of lesions and the lack of information about the lesion location within each individual vessel are limitations of the present analysis. Moreover, we did not capture information on changes in planned stent size and length by the interventionalist during the intervention.
Conclusion
Lesion preparation with either RA or MB before drug-eluting stent implantation in severely calcified coronary lesions is associated with a comparable strategy success rate in LAD lesions. In lesions located outside the LAD, an upfront RA-based strategy may be superior to MB.
|
Impact on daily practice Optimal lesion preparation is critical in severely calcified coronary lesions. Lesion location may play an important role in technical success. This subgroup analysis of the PREPARE-CALC trial suggests that lesions located in the LAD may be equally well treated with an initial strategy of RA or MB angioplasty, whereas a non-LAD lesion location favoured a strategy of upfront RA. |
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Conflict of interest statement
R. Toelg reports speaker honoraria from Boston Scientific and Biotronik. R.A. Byrne reports lecture fees from B. Braun Melsungen AG, Boston Scientific, Biotronik, and Micell Technologies, and research funding to the institution from Boston Scientific and CeloNova Biosciences. The other authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Supplementary data
To read the full content of this article, please download the PDF.