Abstract
Aims: Little information is available on the outcome after rotational atherectomy (RA) followed by drug-eluting stent (DES) implantation in calcified coronary lesions. The aim of this study was to evaluate the outcome of patients with severe lesion calcification undergoing RA followed by implantation of DES.
Methods and results: Ninety-five patients with 96 de novo severely calcified lesions were included. Twenty-nine patients (30.5%) had diabetes mellitus and seven patients (7.4%) had chronic renal failure. The total stent length per lesion was 48.4±24.9 mm. Procedural success rate was 95.8%. The incidence of cumulative major adverse cardiac events, defined as death, myocardial infarction (MI) and target vessel revascularisation (TVR), was 15.8% at the mean follow-up period of 14.7 months (range 6.0–57.7). Death occurred in four patients (4.2%). Non Q-wave MI occurred in 3 patients (3.2%) and Q-wave MI occurred in two patients (2.1%). The rate of target lesion revascularisation (TLR) was 9.5%. The rate of TVR was 11.6%. Two definite (2.1%) and 2 possible (2.1%) stent thromboses were observed.
Conclusions: RA followed by DES implantation in severely calcified coronary lesions appears to be feasible including high rate of procedural success and low-incidence of TLR considering this complex lesion subset.
Introduction
Coronary lesions with severe calcification have been classified as complex lesions and known to carry lower success rates and higher complication rates following percutaneous coronary intervention (PCI) compared to non- or mildly calcified lesions.1,2 In particular, stent delivery may be problematic and complete stent expansion may be difficult due to the resistance of heavily calcified plaque at the lesion site. Rotational atherectomy (RA, Rotablator, Boston Scientific-Scimed, Maple Grove, MN, USA) can facilitate stent delivery and expansion through calcific burden reduction and plaque modification, and improve procedural success rates for this type of lesions.2–4 Yet, the rates of target lesion revascularisation (TLR) and/or restenosis have not been satisfactory when bare-metal stents (BMS) were used.3–6 The use of drug-eluting stents (DES) has been reported to reduce TLR compared to BMS.7,8 However, little is known if the benefit of DES persists in calcified coronary lesions requiring RA before implantation of DES.
The aim of this study was to evaluate the outcome of patients with severe lesion calcification undergoing RA followed by DES implantation.
Methods
Study population
From April 2002 to November 2006, a consecutive series of patients with severely calcified de novo lesions undergoing RA before DES implantation was retrospectively identified from our database. Severely calcified lesions were defined visually as ACC/AHA lesion type B or C due to the presence of calcium within the vascular wall at the site of the stenosis that was noted without cardiac motion before contrast injection, generally compromising both sides of the arterial lumen.
Patients with myocardial infarction (MI) within the last 24 hours were excluded from analysis.
Procedure
PCI was performed after obtaining written informed consent. Procedural details of RA have been reviewed elsewhere.6 Procedures began with a 1.25, 1.5 or 1.75 mm burr with lower speed of between 150,000 and 170,000 rpm. Care was taken to prevent any drop in rotational speed 5,000 rpm using to-and-fro pecking motion of the burr, avoiding long passes. Intracoronary verapamil, nitroglycerin and pauses of ablation runs were used to control any slow-flow occurring during or after RA.
All patients were pretreated with aspirin and either ticlopidine or clopidogrel. A minimum of 300 mg loading dose of clopidogrel was administered before the procedure if patients were not pretreated. During interventions, patients received intravenous unfractionated heparin (100 IU/kg) to maintain activated clotting time > 300 seconds. Dual antiplatelet therapy with aspirin and a thienopyridine (ticlopidine 250 mg twice daily or clopidogrel 75 mg/day) was continued for at least six months after DES implantation.
Post-procedural creatine kinase (CK) was routinely measured in all patients after the index procedure. In case of a rise in CK over the upper normal limit, CK and CK-MB measurements were repeated.
Definitions
Chronic renal failure was defined as the presence of previously documented renal failure and/or a baseline serum creatinine level > 1.5 mg/dl. Procedural success was defined as a final residual stenosis < 30% and grade 3 Thrombolysis In Myocardial infarction (TIMI) flow without in-hospital major adverse cardiac events (MACE). MACE were defined as death, MI, and TVR, either percutaneous or surgical. Deaths were classified as either cardiac or non-cardiac. Death of unknown cause was adjudicated as cardiac. MI was defined as a rise in CK concentration above twice the upper normal limit in conjunction with an elevation of the CK-MB fraction. TLR was defined as a repeat revascularisation with a stenosis > 50% in the target segment. TVR was defined as any repeat revascularisation within the treated vessel.
Stent thrombosis was classified according to the Academic Research Consortium (ARC) definition.9
Quantitative coronary angiographic analysis
Cineangiograms were analysed with a validated edge detection system (CMS, version 6.0; MEDIS, Leiden, the Netherlands). Analysis was performed inside the stent and in the 5 mm proximally and distally to the stented segment.
Statistical analysis
Descriptive analyses were used. Continuous variables are presented as mean±SD and categorical variables are presented as frequencies with percentage.
Results
Baseline and procedural characteristics
A total of 95 patients with 96 de novo severely calcified coronary lesions were identified. Of those, bailout RA was performed in 61 lesions (63.5%) because of impossibility to cross the lesion with a balloon or impossibility to expand a balloon after crossing. Baseline clinical characteristics are reported in Table 1.
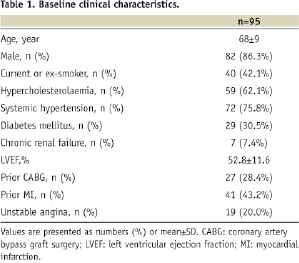
Overall, 29 patients (30.5%) had diabetes mellitus and seven patient (7.4%) had chronic renal failure. Lesion and procedural characteristics are reported in Table 2.
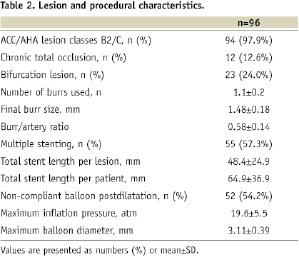
Fifty-one lesions (53.1%) were located in the left anterior descending artery; 16 (16.7%) in the left circumflex artery; 20 (20.8%) in the right coronary artery; and nine (9.4%) in the left main coronary artery (four were unprotected). There were 12 chronic total occlusions (12.6%) and 23 lesions involving a major side branch (24.0%). The number of diseased vessels per patient was 1.6±0.8. After RA, the following stents were implanted: the Cypher stent (Cordis, Johnson and Johnson Company, Warren, NJ, USA) in 44 patients with 45 lesions, the Taxus stent (Boston Scientific, Natick, MA, USA) in 40 patients, the Endeavor stent (Medtronic, Minneapolis, MN, USA) in three patients and the Costar stent (Conor Medsystems, Menlo Park, CA, USA) in eight patients. In particular, multiple stenting was utilised in 55 lesions (57.3%). Among 23 bifurcation lesions, stenting of both the main branch and the side-branch was utilised in 14 lesions. Postdilatation with the non-compliant balloon was performed in 52 lesions (54.2%). The maximum inflation pressure was 19.6±5.5 atmospheres. Intravascular ultrasound (IVUS)-guided procedure was performed in 23 lesions (24.0%). The number of stents implanted per lesion was 1.8±0.8 and the total stent length per lesion was 48.4±24.9 mm. Thirty-eight patients (40.0%) received additional stenting to treat other non-severely calcified lesions without RA during the index procedure. The number of lesions treated per patient was 1.6±0.8. The number of stents implanted per patient was 2.5±1.3 and the total stent length per patient was 64.9±36.9 mm. The rate of complete revascularisation was 82.1%. Glycoprotein IIb/IIIa inhibitors were electively utilised in 26 patients (27.4%). Intra-aortic balloon pump (IABP) was electively inserted in nine patients (9.5%).
Quantitative angiographic results
The quantitative angiographic results are reported in Table 3.
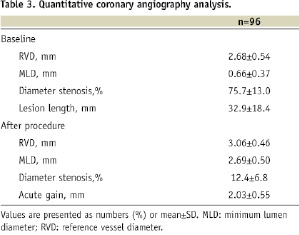
The reference vessel diameter was 2.68±0.54 mm. Residual stenosis was 12.4±6.8%. The lesion length at baseline was 32.9±18.4 mm and 56 lesions (58.3%) were > 20 mm. After final stent dilatation, the acute gain was 2.03±0.55 mm.
In-hospital and clinical outcomes
In-hospital and clinical outcomes are shown in Table 4.
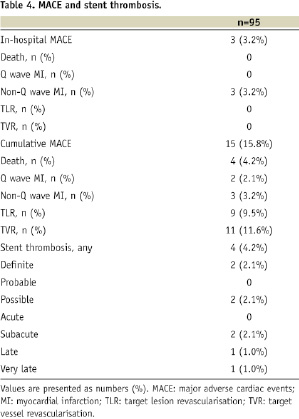
Procedural success rate was 95.8%: one patient had residual stenosis of 36.12% by quantitative angiography and three patients (3.2%) developed a non-Q–wave MI during hospitalisation. Of those, prolonged slow-flow was observed in one patient after RA. In addition, one minor coronary perforation (type II according to the Ellis classification) and two spiral coronary dissections (type D according to the NHLBI classification) occurred during the procedure, however, without any MACE.
The incidence of cumulative MACE was 15.8% at the mean follow-up period of 14.7 months (range 6.0–57.7). Among 15 patients with MACE, 9 were treated with the Cypher stent and six were treated with the Taxus stent in the index procedure. Death occurred in four patients (4.2%): all were sudden cardiac deaths. Non Q-wave MI occurred in three patients (3.2%). Q-wave MI occurred in two patients (2.1%): both were due to angiographic documented stent thrombosis. TLR occurred in nine patients (9.5%). Of those, six (including two with definite stent thrombosis) were performed for symptoms and/or signs of ischaemia. TVR occurred in 11 patients (11.6%). Of those, 10 patients were treated by PCI and one by CABG. Among 45 patients (47.4%) with angiographic follow-up, no coronary aneurysms were found in the stented segment. Binary restenoses were observed in seven patients with eight lesions. Of those, seven were focal (< 10 mm in length) in-stent and one was total occlusion. All restenoses were successfully treated with repeat PCI.
The mean duration of dual antiplatelet therapy was 9.9 months (range 6.0–51.6). Overall, stent thrombosis occurred in four patients (4.2%) (Table 4). Of those, two were definite (2.1%) with angiographic confirmation after hospital discharge and occurred at two days and four days after the procedure with total stent length of 105 mm (Cypher stents) and 130 mm (Taxus stents). Both patients were successfully treated with balloon angioplasty resulting in TLR. One of these had chronic renal failure. Both patients suffered from sudden cardiac deaths at 71 days and 172 days after the index procedure while on dual antiplatelet therapy. The other two thrombotic events were possible (2.1%) with sudden cardiac deaths at 198 days (during dual antiplatelet therapy) and 537 days (aspirin therapy only) after stenting.
Discussion
PCI for severely calcified lesions has been one of the most difficult procedures to achieve procedural success.1,2 RA followed by implantation of BMS has emerged as a promising technique for treatment of this subset of lesions.2–6 Using BMS, Moussa et al previously reported procedural success in 93.4% of cases, but with TLR rate of 18.0% and restenosis rate of 22.5%, despite the mean lesion length was only 9.4±6.8 mm.3 Similarly, other studies showed favourable acute results but high rates of TLR and/or angiographic restenosis after BMS implantation following RA.4–6 Implantation of DES has shown lower TLR rates compared to BMS.7,8 Yet, little information is available on the outcome after RA followed by DES implantation in calcified coronary lesions. Recently, Clavijo et al reported an excellent result of TLR rate of 4.2% at six months follow-up after RA followed by sirolimus-eluting stent implantation in 81 patients with calcified lesions.10 Although pre-intervention lesion length was not presented in this study, total stent length was 24.4±6.27 mm which was shorter than that in our study of 48.4±24.9 mm. Moreover, they reported the rate of bailout RA was only 22%, which was quite less compared to our study of 63.5%. Also, Khattab et al showed TLR rate of 7.4% at nine months follow-up after implantation of DES following RA in 27 patients with calcified lesions.11 In this study, the rate of bailout RA was unavailable and total stent length was only 25.4±24.9 mm. Therefore, TLR in our study would be more frequent as the “real-world” outcome for complex diffuse calcified lesions compared to those reported by Clavijo et al or Khattab el al. However, we think that the TLR rate of 9.5% is quite encouraging regarding the complexities of patients and lesions in the present study, including diabetes mellitus of 30.5%, chronic total occlusions of 12.6%, bifurcation lesions of 24.0% and multiple stenting of 57.3%. It has been reported that post-procedure minimum stent area is correlated with restenosis following DES implantation.12,13 RA is helpful to facilitate stent expansion in calcified lesions through plaque modification.2 In addition, high-pressure dilatation can improve expansion of DES.14 The plaque modification with RA in conjunction with aggressive stent dilatation with mean maximum inflation pressure of 19.6±5.5 atmospheres might reduce restenosis resulting in the low rate of TLR in the present study. Furthermore, damage to polymer has been reported after delivery failure of the Cypher stent.15 The use of RA can facilitate stent delivery and this may avoid damage to polymer of DES and reduce TLR.
There have been many concerns on stent thrombosis after DES implantation.16,17 Although we cannot make a definite statement because of small sample size of the present study, the rate of definite/probable stent thrombosis of 2.1% might be relatively high, compared to those of simpler patients and lesions. However, it may be justified by such complex lesion subset. Both stent under-expansion and total stent length have been reported as independent factors for DES thrombosis.18–20 Thus, plaque modification with RA to achieve appropriate stent expansion in severely calcified lesions, especially in diffuse long ones requiring multiple stenting, will be quite important to prevent stent thrombosis.
The present study has some limitations. It is an observational study reflecting the experience of a single institution without the control group. However, it is extremely difficult to have an adequate control group and randomisation would be impossible because the calcified lesions that cannot be dilated without RA do not undergo successful stenting. CK-MB measurements were taken, only in case of a rise in CK over the upper normal limit after the index procedure. If we were able to define MI as a rise in CK-MB concentration above three times the upper normal limit, the rate of non Q-wave MI might be higher than 3.2% during hospitalisation. In addition, the sample size is relatively small and angiographic follow-up, which may trigger TLR, was obtained only in 47.4% of patients.
Conclusions
In conclusion, RA followed by DES implantation in severely calcified coronary lesions appears to be feasible, including a high rate of procedural success and a low-incidence of TLR considering this complex lesion subset.
Acknowledgements
We would like to thank Massimo Ferraro, RN, for providing data during preparation of the manuscript.

