Coronary calcification represents an advanced stage of the inflammatory atherosclerosis process1. From a clinical point of view, it is associated with the elderly and chronic comorbidities such as diabetes mellitus or chronic kidney disease23. Typically, in these clinical contexts, revascularisation outcomes from percutaneous coronary intervention are worse than those in younger and less comorbid patients45.
Currently, the ageing of the population is leading to an increase in the number of comorbid patients with calcified coronary arteries needing revascularisation6. Moreover, in this subset of patients, the selected revascularisation type is most often percutaneous, given the less invasive nature of the procedure compared to coronary artery bypass graft. As a result, most interventional cardiologists have to deal with complex, high-risk percutaneous coronary intervention (CHIP) procedures in everyday practice. The treatment of diffuse calcified lesions falls entirely within this category of CHIP procedures that require the use of specific tools to successfully perform the procedures.
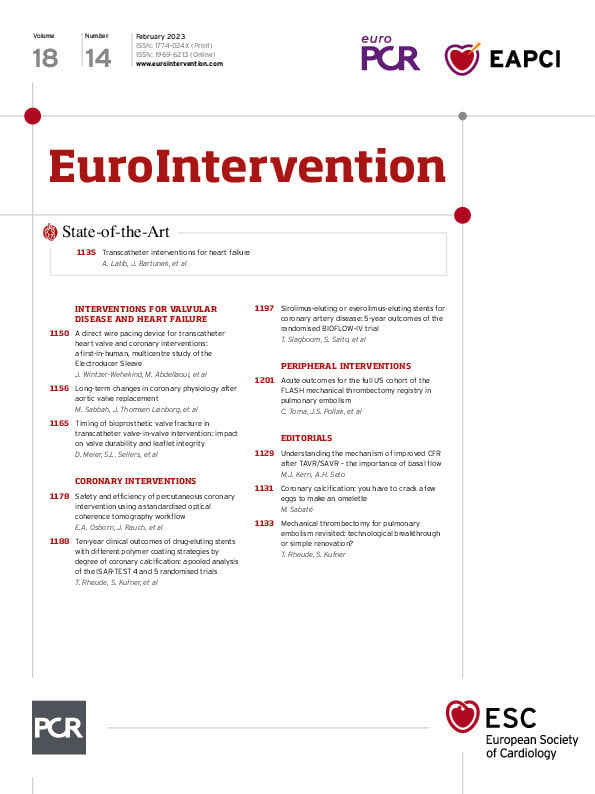
In this issue of EuroIntervention, Rheude et al investigate the long-term outcomes (up to 10 years) of patients treated with different stent platforms according to the degree of coronary artery calcification7. In a pooled analysis involving 4,953 patients (6,924 lesions), the authors found an incremental risk of events according to the degree of calcification. Interestingly, in patients with severe calcification, no differences in event rates were observed between permanent polymer, biodegradable polymer and polymer-free drug-eluting stent platforms. At 10 years, the rates of clinical events in patients with severe calcification nearly doubled, including mortality, target lesion revascularisation, myocardial infarction and stent thrombosis, compared to those without angiographic calcification. Remarkably, 10-year mortality and target lesion revascularisation rates in the group with heavily calcified lesions nearly reached one in two and one in three, respectively.
From a procedural point of view, despite being highly complex lesions (high rates of type B2/C lesions, chronic total occlusions and ostial locations) with long lesion and stent lengths, the use of rotational atherectomy was anecdotal even in heavily calcified patients (3%). Lesion/vessel preparation is essential to ensure adequate stent expansion. Stent underexpansion is typically related to an increased risk of stent thrombosis and restenosis8. In fact, in the present study, stent thrombosis was three times higher in severe calcified lesions (3.6% vs 1.3% in non-calcified vessels). We must acknowledge that some of the current balloon-based techniques and the new ablative tools (e.g., orbital atherectomy) were not available on the market a decade ago. However, others, such as the above-mentioned rotablation or scoring/cutting balloons, were available and might have eventually impacted long-term prognoses if used more frequently in this heavily calcified cohort of patients9. Similarly, the rate of intravascular imaging (IVI) use was not reported. IVI has been demonstrated to improve outcomes and is currently recommended in CHIP procedures9. Imaging may help recognise the calcium disposition, select the debulking technique, assess the response to lesion preparation and optimise stent implantation. In this regard, several algorithms have been developed to help in the decision-making process of the treatment of calcified lesions10.
Despite the above-described limitations, the results of this study will lay the groundwork for future trials aimed at improving outcomes in CHIP procedures.
Conflict of interest statement
The author has no conflicts of interest to declare.