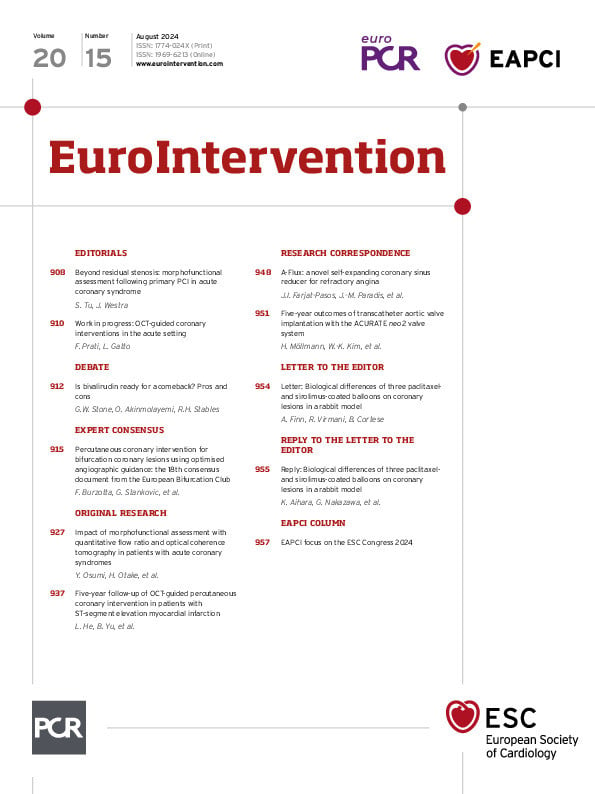
Abstract
BACKGROUND: Combining morphological and physiological evaluations might improve the risk stratification of patients who undergo percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS) culprit lesions.
AIMS: We aimed to investigate the clinical utility of morphofunctional evaluation after PCI for identifying ACS patients with increased risk of subsequent clinical events.
METHODS: We retrospectively studied 298 consecutive ACS patients who had undergone optical coherence tomography (OCT)-guided PCI. We performed OCT-based morphological analysis and quantitative flow ratio (QFR)-based physiological assessment immediately after PCI. The non-culprit segment (NCS) was defined as the most stenotic untreated segment in the culprit vessel. The primary outcome was target vessel failure (TVF), a composite of cardiac death, target vessel-related myocardial infarction, and ischaemia-driven target vessel revascularisation.
RESULTS: During a median follow-up period of 990 days, 42 patients experienced TVF. Cox regression analysis revealed that the presence of thin-cap fibroatheroma (TCFA) in the NCS and a low post-PCI QFR, or the presence of TCFA in the NCS and a high ΔQFR in the NCS (QFRNCS), were independently associated with TVF. The subgroup with TCFA in the NCS and a low post-PCI QFR had a significantly higher incidence of TVF (75%) than the other subgroups, and those with TCFA in the NCS and a high ΔQFRNCS had a significantly higher incidence of TVF (86%) than the other subgroups. The integration of TCFA in NCS, post-PCI QFR, and ΔQFRNCS with traditional risk factors significantly enhanced the identification of subsequent TVF cases.
CONCLUSIONS: Combining post-PCI OCT and QFR evaluation may enhance risk stratification for ACS patients after successful PCI, particularly in predicting subsequent TVF.
Optical coherence tomography (OCT) provides high-resolution imaging for stent optimisation during percutaneous coronary intervention (PCI)1. Residual ischaemia correlates with poorer clinical outcomes2. However, PCI adequacy is predominantly evaluated through OCT-based morphology, often without physiological assessment, especially in patients with acute coronary syndrome (ACS). OCT detects vulnerable plaques like thin-cap fibroatheroma (TCFA), which predict future cardiovascular events. Yet, relying solely on OCT morphology lacks sufficient positive predictive value, necessitating further refinement.
Fractional flow reserve (FFR) is a common method for evaluating myocardial ischaemia. Previous studies consistently demonstrated that post-PCI FFR can predict long-term cardiovascular events in chronic coronary syndrome (CCS) patients2. Quantitative flow ratio (QFR), an angiographically derived alternative to wire-based FFR, has emerged recently. Previous trials have demonstrated that QFR agrees with FFR measurements3. Based on these findings, we hypothesised that combining morphological plaque assessment using OCT and physiological assessment using QFR might improve the risk stratification of patients who undergo PCI for ACS culprit lesions. Thus, we conducted this study to investigate the clinical utility of morphofunctional evaluation after PCI for identifying ACS patients with an increased risk of subsequent clinical events.
Methods
STUDY POPULATION
This study included patients with ACS who had undergone OCT-guided PCI for de novo native lesions with drug-eluting stents between January 2010 and October 2020 at 5 institutions. The exclusion criteria were (1) left main trunk artery lesion, (2) cases without analysable OCT imaging, (3) cases with a final Thrombolysis in Myocardial Infarction grade <3, (4) lesions involving the right coronary artery ostium, (5) patients with atrial fibrillation, (6) patients with cardiac shock, (7) cases with poor angiogram quality for QFR, and (8) patients without at least 6 months of follow-up. Participating institutions and detailed definitions of ACS are provided in Supplementary Appendix 1 and Supplementary Appendix 2.
The study protocol complied with the Declaration of Helsinki and was approved by the Ethics Committee of Kobe University Hospital. Informed consent was obtained as an opt-out on the Division of Cardiovascular Medicine website at Kobe University Graduate School of Medicine. The study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN000047675).
OPTICAL COHERENCE TOMOGRAPHY IMAGING ANALYSIS AND DEFINITIONS
We retrospectively collected the OCT images from a frequency-domain OCT system (ILUMIEN [Abbott]) at the end of the procedure. Details of the OCT image acquisition technique are described in Supplementary Appendix 3.
The OCT images were analysed for every cross-section over the entire length of the target segment. The target vessel segment was divided into the following longitudinal subsegments: (1) stented segment, (2) adjacent reference segment (≤5 mm in length), and (3) non-culprit segment (NCS) (Figure 1). The NCS was defined as the most stenotic untreated segment, with 30-70% area stenosis outside the stented segment in the entire OCT pullback analysis. The lumen area measurements were obtained in every frame at 0.1 mm or 0.2 mm intervals.
A qualitative assessment was performed to evaluate the presence of irregular in-stent protrusion, thrombus, malapposition, stent edge dissection, lipid-rich plaque (LRP), and TCFA. The details of the OCT analysis are presented in Supplementary Appendix 3.

Figure 1. Subsegments analysed by QFR and OCT. A) QFR (the NCS is indicated with a yellow arrow; the white bracket indicates ΔQFRNCS) and (B) OCT showing (1) stented segment; (2) adjacent reference segment (≤5 mm); (3) non-culprit segment. NCS: non-culprit lesion; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; QFR: quantitative flow ratio; QFRNCS: QFR in the NCS
POST-PCI QUANTITATIVE FLOW RATIO COMPUTATIONAL ANALYSIS
QFR was computed offline using the three-dimensional (3D) software package QAngio XA 3D (Medis Medical Imaging). 3D quantitative coronary angiography (3D-QCA) data were readily available.
Post-PCI QFR was calculated for the target vessel, and ΔQFR in the NCS (QFRNCS) was calculated in the same vessel. ΔQFRNCS represents the pressure gradients at the NCS (Figure 1). Details of the QFR analysis are presented in Supplementary Appendix 4.
OUTCOMES AND STATISTICAL ANALYSIS
The primary outcome was target vessel failure (TVF), defined as a composite of cardiac death, target vessel-related myocardial infarction (MI), and ischaemia-driven target vessel revascularisation (TVR). We further assessed non-target lesion revascularisation (TLR) TVR to evaluate the relationship between NCS-related findings and non-TLR TVR separately. Further details of the outcomes and statistical analyses are described in Supplementary Appendix 5 and Supplementary Appendix 6.
Results
STUDY POPULATION
In total, 456 consecutive patients underwent OCT-guided PCI for ACS during the study period. After excluding 158 patients, 298 patients with 298 vessels were enrolled in this study (Supplementary Figure 1). All vessels had the NCS outside the stent segments, with a median artery length of 26.7 (interquartile range [IQR] 18-36) mm, which was not significantly different between the TVF and non-TVF groups. The mean % diameter stenosis (DS) by 3D-QCA of the NCS was 21.5±12.1%. Baseline patient, lesion, and procedural characteristics are shown in Table 1. Post-PCI 3D-QCA, QFR, and OCT findings are shown in Table 2 and Table 3. The distribution of post-PCI QFR is shown in Supplementary Figure 2, with a median value of 0.96 (IQR 0.91-0.98).
Table 1. Baseline characteristics.
| Overall (n=298) | TVF (n=42) | Non-TVF (n=256) | p-value | |
|---|---|---|---|---|
| Age, years | 66±12 | 66±13 | 66±12 | 0.63 |
| Male | 227 (76) | 30 (71) | 197 (77) | 0.44 |
| Hypertension | 194 (65) | 26 (62) | 168 (66) | 0.64 |
| Diabetes mellitus | 112 (38) | 16 (38) | 96 (38) | 0.94 |
| Dyslipidaemia | 197 (66) | 24 (57) | 173 (68) | 0.19 |
| Haemodialysis | 4 (1) | 2 (5) | 2 (1) | 0.04 |
| Smoker | 177 (59) | 25 (60) | 152 (59) | 0.98 |
| Family history | 60 (20) | 14 (33) | 46 (18) | 0.02 |
| ACS | 0.31 | |||
| STEMI | 194 (65) | 28 (67) | 166 (65) | |
| NSTEMI | 62 (21) | 11 (26) | 51 (20) | |
| uAP | 42 (14) | 3 (7) | 39 (15) | |
| Laboratory data | ||||
| eGFR, mL/min/1.73 m2 | 72.0±18 | 70.9±23 | 71.7±17 | 0.78 |
| Peak CK, IU/L | 1,275 (347-2,579) | 1,246 (399-2,863) | 326 (1,275-2,513) | 0.42 |
| Peak CK-MB, IU/L | 123 (26-270) | 110 (30-260) | 123 (24-271) | 0.71 |
| LVEF, % | 54.3±10.4 | 50.3±11.5 | 55.0±10.1 | 0.007 |
| Medication at discharge | ||||
| Statin | 286 (96) | 39 (93) | 247 (96) | 0.27 |
| ß-blocker | 191 (64) | 32 (76) | 159 (62) | 0.08 |
| Lesion characteristics | ||||
| Vessel location | 0.68 | |||
| LAD | 171 (57) | 26 (62) | 145 (57) | |
| LCx | 32 (11) | 3 (7) | 29 (11) | |
| RCA | 95 (32) | 13 (31) | 82 (32) | |
| Multivessel disease | 107 (36) | 23 (55) | 84 (33) | 0.006 |
| Procedure | ||||
| Stent diameter, mm | 3 (2.75-3.5) | 3 (2.5-3) | 3 (2.75-3.5) | 0.33 |
| Stent length, mm | 24 (18-32) | 28 (21-32) | 24 (18-32) | 0.41 |
| Post-dilation | 212 (71) | 26 (62) | 186 (73) | 0.15 |
| Values are expressed as mean±standard deviation, n (%) or median (25th-75th percentiles). ACS: acute coronary syndrome; CK: creatine kinase; CK-MB: creatine kinase-myocardial band; eGFR: estimated glomerular filtration rate; IU: international units; LAD: left anterior descending artery; LCx: left circumflex artery; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NSTEMI: non-STEMI; PCI: percutaneous coronary intervention; RCA: right coronary artery; STEMI: ST-segment elevation myocardial infarction; TVF: target vessel failure; uAP: unstable angina pectoris | ||||
Table 2. Post-PCI physiological indices.
| Overall (n=298) | TVF (n=42) | Non-TVF (n=256) | p-value | |
|---|---|---|---|---|
| Entire target vessel | ||||
| MLD, mm | 1.8±0.5 | 1.7±0.5 | 1.8±0.5 | 0.10 |
| Diameter stenosis, % | 34.2±9.8 | 41.1±12.4 | 33.1±8.8 | <0.001 |
| Post-PCI QFR | 0.96 (0.91-0.98) | 0.86 (0.73-0.94) | 0.96 (0.91-0.98) | <0.001 |
| Non-culprit lesion | ||||
| MLD, mm | 2.4±0.6 | 2.0±0.6 | 2.4±0.5 | <0.001 |
| Diameter stenosis, % | 21.5±12.1 | 32.0±13.6 | 19.7±11.1 | <0.001 |
| ∆QFRNCS | 0.006 (0-0.027) | 0.06 (0.020-0.080) | 0.004 (0-0.018) | <0.001 |
| Values are expressed as mean±standard deviation or median (25th-75th percentiles). MLD: minimum lumen diameter; NCS: non-culprit segment; PCI: percutaneous coronary intervention; QFR: quantitative flow ratio; QFRNCS: QFR in the NCS; TVF: target vessel failure | ||||
Table 3. Post-PCI OCT findings.
| Overall (n=298) |
TVF (n=42) | Non-TVF (n=256) | p-value | |
|---|---|---|---|---|
| Target vessel | ||||
| Length, mm | 51.9±12.8 | 53.3±11.5 | 50.5±15.0 | 0.47 |
| MLA, mm2 | 3.9±2.3 | 2.8±1.8 | 4.0±2.4 | <0.001 |
| Stented segment | ||||
| Average lumen area, mm2 | 6.8±2.1 | 6.3±2.5 | 6.8±2.1 | 0.18 |
| MLA, mm2 | 5.2±1.7 | 4.7±1.8 | 5.2±1.7 | 0.049 |
| Lumen expansion, % | 80.5±17.4 | 79.0±17.7 | 77.7±16.7 | 0.65 |
| Irregular protrusion | 143 (48) | 29 (69) | 114 (44) | 0.003 |
| Thrombus | 84 (34) | 21 (50) | 63 (25) | <0.001 |
| Malapposition | 56 (23) | 10 (24) | 46 (18) | 0.37 |
| Suboptimal stent deployment | 177 (59) | 27 (64) | 150 (59) | 0.49 |
| Reference segment | ||||
| Proximal reference | ||||
| Mean lumen area, mm2 | 7.8±2.9 | 7.1±3.2 | 8.0±2.8 | 0.06 |
| Stent edge dissection | 15 (5) | 5 (12) | 10 (3) | 0.028 |
| Thrombus | 32 (11) | 10 (24) | 22 (9) | 0.003 |
| LRP | 65 (22) | 16 (38) | 49 (19) | 0.006 |
| TCFA | 13 (4) | 5 (12) | 8(3) | 0.01 |
| Distal reference | ||||
| Mean lumen area, mm2 | 5.7±2.5 | 5.3±3.1 | 5.7±2.3 | 0.22 |
| Stent edge dissection | 13 (4) | 3 (7) | 10 (3) | 0.34 |
| Thrombus | 21 (7) | 5 (12) | 16 (6) | 0.18 |
| LRP | 34 (11) | 7 (17) | 27 (11) | 0.25 |
| TCFA | 10 (3) | 3 (7) | 7 (3) | 0.14 |
| Mean reference lumen area, mm2 | 6.8±2.3 | 6.2±2.8 | 6.9±2.2 | 0.07 |
| Non-culprit segment | ||||
| Artery length outside stent segment, mm | 26.7 (18-36) | 26.4 (19.2-33.9) | 26.8 (17.9-36.8) | 0.80 |
| Distance from stent, mm | 16 (13-21) | 16 (13-20) | 18 (14-23.3) | 0.10 |
| Length, mm | 9.5 (5.6-13.6) | 14.2 (10.3-16.9) | 8.4 (5.2-12.4) | <0.001 |
| MLA, mm2 | 5.0±2.6 | 3.9±2.6 | 5.2±2.5 | 0.004 |
| Thrombus | 14 (5) | 3 (7) | 11 (4) | 0.42 |
| LRP | 100 (34) | 23 (55) | 77 (30) | <0.001 |
| TCFA | 27 (9) | 11 (26) | 16 (6) | <0.001 |
| Values are expressed as mean±standard deviation, n (%) or median (25th-75th percentiles). LRP: lipid-rich plaque; MLA: minimum lumen area; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; TCFA: thin-cap fibroatheroma; TVF: target vessel failure | ||||
CLINICAL OUTCOME
During the median follow-up period of 990 (IQR 700-1,350) days after PCI, 42 (14%) patients experienced TVF. This included 9 (3%) patients who had cardiac death, 3 (1%) patients who experienced target vessel-related MI, and 34 (11%) patients who experienced TVR (Supplementary Table 1).
The median value of QFR at the time of the TVR event was significantly lower than that at the time of primary PCI (0.69 vs 0.85; p<0.001), and the median value of lesion-level ΔQFRNCS at the time of the TVR event was significantly higher than that at the time of primary PCI (0.18 vs 0.06; p<0.001) (Supplementary Figure 3). Further details and a representative case of TVF are shown in Supplementary Figure 4.
COMPARISONS BETWEEN THE TARGET VESSEL FAILURE AND NON-TARGET VESSEL FAILURE GROUPS
Patients in the TVF group had significantly higher frequencies of haemodialysis, family history of cardiovascular disease, and multivessel disease. They also had a significantly lower left ventricular ejection fraction (LVEF) than those in the non-TVF group (Table 1).
Regarding post-PCI 3D-QCA and QFR analysis, significantly higher %DS and lower post-PCI QFR in the entire vessel, as well as higher %DS and ΔQFRNCS in the NCS, were observed in the TVF group than in the non-TVF group (Table 2).
Post-PCI OCT findings are shown in Table 3. The TVF group had a significantly smaller minimum lumen area (MLA) in the target vessel than the non-TVF group. The in-stent MLA was significantly smaller in the stented segment, and the prevalence of irregular protrusions and thrombus was significantly higher in the TVF group than in the non-TVF group. The prevalence of suboptimal stent deployment was not significantly different between the 2 groups (p=0.49).
Regarding OCT findings of the reference segment, the TVF group had a significantly higher frequency of stent edge dissection, thrombus, LRP, and TCFA at the proximal reference than the non-TVF group.
Regarding the OCT findings of the NCS, the TVF group had significantly longer lesion lengths and smaller MLA than the non-TVF group. The frequencies of LRP and TCFA were significantly higher in the TVF group than in the non-TVF group.
FACTORS ASSOCIATED WITH TARGET VESSEL FAILURE
The results of univariate and multivariate Cox regression analyses for clinical factors, QFR, and OCT findings associated with TVF are summarised in Table 4 and Supplementary Table 2. Multivariate model 1 showed that LVEF, post-PCI QFR, MLA in the NCS, and TCFA levels in the NCS were independently associated with TVF. Multivariate model 2 also showed that ΔQFRNCS, thrombus levels in the stented segment, and TCFA levels in the NCS were independently associated with TVF. The MLA in the NCS was not associated with TVF.
Receiver operating characteristic analysis showed that the cutoff value of post-PCI QFR and ΔQFRNCS for identifying patients with subsequent TVF were 0.88 (sensitivity: 57.1, specificity: 88.3, the area under the curve [AUC]: 0.783, 95% confidence interval [CI]: 0.70-0.87) and 0.046 (sensitivity: 61.9, specificity: 92.6, AUC: 0.790, 95% CI: 0.70-0.88), respectively (Supplementary Figure 5). The incidence of TVF according to post-PCI QFR, ΔQFRNCS, and TCFA in the NCS is summarised in Supplementary Figure 6. Furthermore, the vessel subgroup with TCFA in the NCS and a low post-PCI QFR had a significantly higher incidence of TVF (75%) than the other subgroups, and patients with TCFA in the NCS and a high ΔQFRNCS had a significantly higher incidence of TVF (86%) than the other patients (Central illustration). Furthermore, those with TCFA in the NCS and a high ΔQFRNCS had a significantly higher incidence of non-TLR TVR (43%). A detailed relationship between TCFA in the NCS and a high ΔQFRNCS and non-TLR TVR is shown in Supplementary Figure 7.
Table 4. Multivariate Cox regression analyses of factors associated with TVF.
| Multivariable | ||||
|---|---|---|---|---|
| Model 1* | Model 2* | |||
| Variables | HR (95% CI) |
p-value | HR(95% CI) | p-value |
| Baseline characteristics | ||||
| LVEF | 0.97 (0.94-0.99) |
0.01 | 0.99 (0.96-1.01) |
0.31 |
| Target vessel | ||||
| Post-PCI QFR (per 0.1 increase) | 0.49 (0.39-0.62) |
<0.001 | ||
| Stented segment | ||||
| Thrombus | 1.42 (0.72-2.79) |
0.32 | 1.85 (0.94-3.63) |
0.07 |
| Reference segment | ||||
| Stent edge dissection at proximal reference | 0.94 (0.35-2.49) |
0.91 | 1.85 (0.40-2.93) |
0.87 |
| Non-culprit lesion | ||||
| ∆QFRNCS (per 0.01 increase) | 1.15(1.10-1.21) | <0.001 | ||
| MLA | 0.82 (0.71-0.96) |
0.01 | 0.88 (0.75-1.03) |
0.12 |
| LRP | 0.97 (0.44-2.15) |
0.93 | 1.29 (0.60-2.76) |
0.51 |
| TCFA | 4.15 (1.67-10.3) |
0.002 | 3.47 (1.46-8.24) |
0.005 |
| HR corresponds to an increase of 0.1, 0.01 unit for each variable except for QFR, ∆QFRNCS. *We used 2 patterns of multivariable models based on the distinct qualities of post-PCI QFR and ∆QFRNCS. CI: confidence interval; HR: hazard ratio; LRP: lipid-rich plaque; LVEF: left ventricular ejection fraction; MLA: minimum lumen area; NCS: non-culprit segment; PCI: percutaneous coronary intervention; QFR: quantitative flow ratio; QFRNCS: QFR in the NCS; TCFA: thin-cap fibroatheroma; TVF: target vessel failure | ||||

Central illustration. Risk stratification of ACS patients by morphofunctional assessment using OCT and QFR. A) The NCS was an untreated, non-significantly stenotic segment outside the stented segment. *indicates presence of TCFA. The yellow dotted arrow indicates the stent location. The red dotted arrow indicates the location of the NCS. B) The vessel subgroup with TCFA in NCS and a low post-PCI QFR had a higher incidence of TVF (75%) than the other subgroups, and patients with TCFA in NCS and a high ΔQFRNCS had a higher incidence of TVF (86%) than the other patients. C) Integration of TCFA in NCS, post-PCI QFR and ΔQFRNCS with traditional risk factors improved discriminatory and reclassification ability in identifying patients with subsequent TVF. ACS: acute coronary syndrome; CI: confidence interval; HR: hazard ratio; IDI: integrated discrimination index; NCS: non-culprit segment; NRI: net reclassification index; OCT: optical coherence tomography; PCI: percutaneous coronary intervention; QFR: quantitative flow ratio; QFRNCS: QFR in the NCS; TCFA: thin-cap fibroatheroma; TVF: target vessel failure
DISCRIMINATORY DIAGNOSTIC ABILITY OF POST-PCI QFR AND ΔQFRNCS TO IDENTIFY PATIENTS WITH SUBSEQUENT TARGET VESSEL FAILURE
The Central illustration shows Harrell’s C-index, net reclassification index (NRI), and relative integrated discrimination index (IDI) values for the four models. Compared with model 1 (traditional risk factors: age, male sex, body mass index, comorbidities of hypertension, dyslipidaemia, diabetes mellitus, smoking, and chronic kidney disease), model 2 (model 1 plus presence of TCFA in the NCS) showed a higher discriminatory ability (C-index: 0.61 vs 0.67; p=0.07) and higher reclassification ability (NRI: 0.391; p=0.005; relative IDI: 0.059; p=0.005) in identifying patients with subsequent TVF. Compared with model 2, model 3 (model 2 plus post-PCI QFR) showed a significantly higher discriminatory ability (C-index: 0.67 vs 0.79; p=0.002) and higher reclassification ability (NRI: 0.98; p=0.001, relative IDI: 0.217; p<0.001). Compared with model 2, model 4 (model 2 plus ΔQFRNCS) showed a significantly higher discriminatory ability (C-index: 0.67 vs 0.82; p<0.001) and higher reclassification ability (NRI: 1.06; p<0.001, relative IDI: 0.262; p<0.001).
FACTORS ASSOCIATED WITH A LOW POST-PCI QFR (<0.88) AND A HIGH ΔQFRNCS (>0.046)
Multivariate logistic regression analysis showed that in-stent thrombus, stent edge dissection at the proximal reference, and lesion length of the NCS were independently associated with a low post-PCI QFR (<0.88). Moreover, lesion length and minimal lumen area at the NCS were independently associated with a high ΔQFRNCS (>0.046) (Supplementary Table 3).
RELATIONSHIP BETWEEN NCS-RELATED FINDINGS AND NON-TLR TARGET VESSEL REVASCULARISATION
Among TVR cases, 19 patients experienced non-TLR TVR due to the development of a new lesion in the culprit vessel, as detailed in Supplementary Table 1. Regarding the relation between NCS findings and the location of non-TLR TVR, within the 19 non-TLR TVR cases, 15 occurrences (79%) were identified at the NCS site. Overall, there were 27 patients with TCFA in the NCS. Among them, 5 patients (19%) experienced non-TLR TVR, all of which occurred at the NCS site. Among 45 patients with a high ΔQFRNCS, 13 patients experienced non-TLR TVR, with 92% of these cases occurring at the NCS site. Furthermore, in the subset of patients presenting both TCFA in the NCS and a high ΔQFRNCS (7 patients), 3 patients (43%) underwent non-TLR TVR, all of which were observed at the NCS site.
Comparisons between the non-TLR TVR group and other groups are presented in Supplementary Table 4 and Supplementary Table 5. Multivariate Cox regression analyses showed that ΔQFRNCS, lesion length at the NCS, and TCFA in the NCS were independently associated with non-TLR TVR (Supplementary Table 6).
Discussion
The main findings of this study are as follows: (1) The TVF group had significantly worse physiological indices, including lower post-PCI QFR and higher ΔQFRNCS. (2) In addition to patient characteristics such as LVEF, the presence of TCFA in the NCS, a low post-PCI QFR, and a high ΔQFRNCS were independently associated with TVF after PCI in patients with ACS. (3) Patients with a high ΔQFRNCS and TCFA in the NCS had the highest TVF rate during a median follow-up of 990 days (86%) after PCI. (4) The addition of morphological OCT findings to cardiovascular risk factors increased the discriminant and reclassification abilities in the identification of subsequent TVF, which were further increased by adding post-PCI QFR or ΔQFRNCS. This real-world cohort study with long-term follow-up clarified the clinical utility of morphofunctional evaluation using QFR and OCT in identifying patients with subsequent TVF in patients with ACS after PCI.
IMPACT OF POST-PCI QFR MEASUREMENT IN PATIENTS WITH ACUTE CORONARY SYNDROME
Previous studies have consistently demonstrated that post-PCI FFR is a predictive marker for long-term cardiovascular events in patients with CCS2. However, reliable physiological assessment during PCI can be challenging in patients with ACS because of microvascular dysfunction caused by capillary swelling and obstruction, distal embolisation, and vasoconstriction. Previous studies have shown elevated FFR values in both the culprit and non-culprit vessels in patients with ACS4, suggesting a potential underestimation of physiological lesion severity when measured during index PCI. The QFR is a physiological index that can be calculated using angiographic data alone. Tang et al assessed the change in the QFR values of the culprit vessel from the index to the staged procedure in patients with ACS. They demonstrated that it is feasible to assess the QFR of culprit vessels immediately after the index PCI5.
Our study identified post-PCI QFR and ΔQFRNCS as powerful independent risk factors for TVF. The Angio-Based Fractional Flow Reserve to Predict Adverse Events After Stent Implantation (HAWKEYE) trial demonstrated that post-PCI QFR was useful in predicting vessel-related cardiovascular events in patients with CCS and non-ST-elevation ACS. They also identified an optimal cutoff value of 0.89 for the post-PCI QFR6. Our study found that the optimal cutoff value for post-PCI QFR was 0.88, consistent with a previous report. These results highlight the significance of post-PCI QFR measurements in patients with ACS, providing a precise method for assessing the severity of residual physiological lesions and predicting clinical outcomes after PCI.
In addition to FFR, prior studies have already demonstrated an association between morphological evaluation of non-culprit lesions and subsequent adverse events. In the PROSPECT study, Stone et al demonstrated that MLA (≤4 mm2) in non-culprit lesions was an independent predictor of major adverse cardiovascular events (MACE) associated with non-culprit lesions in ACS patients7. However, in our study, MLA in the NCS was not associated with TVF when adjusted by ΔQFRNCS. Similarly, in the EMERALD study, Lee et al also demonstrated that the local pressure gradient (Δcomputed tomography-derived FFR [FFRCT]) had the highest discriminatory ability for subsequent coronary events compared to other indices, including %DS8, which is consistent with the results of our study. We currently speculate that the local physiological pressure gradient is a more important factor in plaque progression compared with single cross-sectional quantitative measurements such as MLA.
Furthermore, Takagi et al demonstrated an improved discrimination ability of translesional FFRCT gradient compared to a standard diagnostic strategy of coronary CT angiography in predicting future revascularisation in patients with CCS9. On the other hand, our study focused not only on the prognostic potential of a high QFR gradient but also on elucidating the prognostic implications of morphofunctional assessment using QFR and OCT. Our results revealed that the combination of the presence of TCFA and translesional QFR gradient (or vessel-level QFR) significantly enhanced the accuracy of predicting TVF after PCI in patients with ACS. Of note, the median ΔQFR value of lesions with subsequent TVF was 0.06, with a cutoff value of 0.046 – considerably lower than those reported by Takagi et al (average translesional FFRCT gradient: 0.24, cutoff: 0.13). However, when combined with the presence of TCFA, our approach demonstrated an approximately 80% TVF rate during the median follow-up of 990 days after the initial PCI. Although we acknowledge the need for confirmation through a future, prospective, large-scale study, we firmly believe that our data demonstrated the potential benefit of angio-based physiological assessment in predicting future clinical outcomes, especially when combined with morphological evaluation by OCT.
RELATIONSHIP BETWEEN THE COMBINED APPROACH OF QFR AND OCT AND CLINICAL OUTCOMES
Several studies have highlighted that the presence of TCFA on OCT is related to subsequent cardiac events in patients with coronary artery disease. In the recent prospective COMBINE OCT-FFR study, Kedhi et al investigated the impact of OCT-detected TCFA on the clinical outcomes of medically treated, angiographically intermediate, but FFR-negative patients with diabetes10. They demonstrated that TCFA-positive patients had a 5-fold higher rate of MACE despite the absence of ischaemia. However, the cumulative MACE rate was only 13.3% during the 18-month follow-up. In a recent single-centre retrospective study that enrolled 1,378 patients, Kubo et al demonstrated that OCT-based plaque characterisation is useful for detecting vulnerable plaques leading to ACS11. However, the positive predictive values of LRPs and TCFA were limited to 11% and 19%, respectively.
Recently, several investigators have demonstrated the potential utility of combining morphological and physiological assessments to predict subsequent cardiac events. Hong et al conducted a retrospective study enrolling 604 patients with ACS who underwent OCT imaging in ≥1 non-culprit vessel during index coronary angiography12. They demonstrated that a comprehensive morphofunctional evaluation of non-culprit vessels was significantly associated with the risk of non-culprit vessel-related MACE, identifying a subgroup of patients with a 43-fold higher risk of recurrent events at the 2-year follow-up. We also reported that adding OCT-derived FFR measurements to post-PCI morphological OCT findings in ACS culprit vessels better discriminated patients with subsequent TVF after PCI for ACS13. Although these studies implied the potential utility of combining morphological and physiological assessments over morphological evaluation alone, they calculated physiological indices from OCT images, limited the evaluation range to scanned segments, and excluded segments outside the range. In contrast, QFR enables physiological assessment of the entire vessel without additional procedures or adverse haemodynamic effects due to hyperaemia induction, which is needed for invasive FFR measurement.
QFR offers the advantage of providing vessel-level FFR measurements and enabling segmental physiological evaluation. In our study, we found that patients with TCFA in the NCS and a low post-PCI QFR (<0.88: vessel-level analysis) had a 19.4-times higher risk of subsequent TVF, while those with TCFA in the NCS and a high ΔQFRNCS (>0.046: lesion-level analysis) had a 31.1-times higher risk of subsequent TVF. These findings suggest that lesion-level physiological assessments may be more effective than vessel-level physiological assessments for predicting subsequent cardiac events after PCI. Therefore, we recommend evaluating post-PCI QFR and ΔQFRNNCS simultaneously and considering additional procedures in patients with a high ΔQFRNCS.
In our study, the median ΔQFRNCS value of lesions with TVF was 0.06, and the cutoff value for predicting TVF was 0.046, indicating that most such lesions were functionally non-significant immediately after PCI. Additionally, the prevalence of a combined high-risk phenotype (TCFA+high ΔQFRNCS) is very low (2%), and the positive predictive value of this finding for non-TLR TVR is limited to 43%. In a retrospective study enrolling patients with ACS who underwent OCT imaging in ≥1 non-culprit vessel12, Hong et al demonstrated that the presence of TCFA was 11%, and the revascularisation or MI rate was 17.2% in patients with TCFA during 24 months of follow-up. Moreover, Kubo et al demonstrated that OCT-based plaque characterisation is useful for TCFA leading to ACS, but the predictive value of this finding was limited to 19%11. In our study, the presence of TCFA alone was 9%, and the cumulative non-TLR TVR rate was 18.5%, consistent with the previous reports. These findings suggest that even in ACS patients, the presence of TCFA in the culprit vessel is not very high, and the presence of TCFA does not always predict future adverse events. On the other hand, our study uniquely demonstrated that the presence of TCFA with a high ΔQFRNCS was only 2%, but this combined approach dramatically increased the positive predictive value of non-TLR TVR (43%) compared with previous studies1112. Although our study does not provide a direct answer to the critical question of whether identification of or preventive treatment for vulnerable, functionally non-significant lesions alters the prognosis of patients, we firmly believe that our data illuminate the potential utility of such preventive measures. The ongoing VULNERABLE study (ClinicalTrials.gov: NCT05599061), a randomised comparison between PCI plus optimal medical therapy (OMT) and OMT alone for the treatment of FFR-negative vulnerable plaques, holds the promise of directly addressing this pivotal question.
Limitations
First, the study was retrospective; therefore, our results were subject to a selection bias. Specifically, including target vessel revascularisation as an endpoint introduces bias, as treating physicians might have been aware of the remaining lesions. Additionally, our results are subject to bias, because this study evaluated only the culprit vessels and could not evaluate non-culprit vessels, which may be associated with clinical outcomes. Furthermore, a prospective study is warranted to determine whether combining OCT and QFR can improve clinical outcomes. Second, the QFR measurements relied on angiographic images and optimal projections. Third, in the acute phase of ACS, factors like myocardial oedema, necrosis, inflammation, vasoconstriction, thrombus formation, or microembolisation during PCI may transiently affect microcirculatory vasodilation, potentially leading to underestimation of the physiological impact of stenotic lesions. This limitation may theoretically apply to QFR measurement in patients with ACS, as QFR simulation relies on an automated frame count for coronary flow assessment. Fourth, the sample size was small, particularly for patients with TCFA in the NCS and a low post-PCI QFR or a high ΔQFRNCS. Further large-scale studies are required to validate these findings.
Conclusions
Post-PCI physiological indices evaluated using QFR provide valuable information for patients with ACS risk stratification. Combining morphological and functional assessments using OCT and QFR allows the identification of patients with ACS at an increased risk of subsequent TVF after PCI. Due to the retrospective nature of the current study, the results should be considered hypothesis-generating, and future prospective studies confirming these findings are needed.
Impact on daily practice
The present study demonstrated that adding the presence of thin-cap fibroatheroma in the non-culprit segment (NCS), post-percutaneous coronary intervention quantitative flow ratio (QFR), and ΔQFR in the NCS to traditional risk factors significantly improved the discriminatory and reclassification abilities for identifying patients with subsequent target vessel failure (TVF). Our results suggested that morphofunctional assessments using optical coherence tomography and QFR allow the identification of patients with acute coronary syndrome at an increased risk of subsequent TVF after PCI.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.