Precision percutaneous coronary intervention (PCI) is a constantly evolving field, which is redefining the standards for indicated and optimised procedures. Physiological assessment of coronary stenoses is recommended by clinical practice guidelines as a tool to investigate the presence of ischaemia-generating lesions and to assist in making decisions on coronary revascularisation1. Imaging-guided PCI is associated with a more favourable prognosis than an angio-guided approach, especially in complex coronary settings (i.e., left main stem disease, chronic total occlusion, long lesions with severe calcifications)2. The utilisation of either physiology or imaging post PCI to optimise the procedural result is associated with improved outcomes2,3. Against this background, a single tool able to provide both imaging and functional information is particularly appealing and may improve the penetration of both physiology and imaging. Indeed, despite strong evidence coming from randomised clinical trials and registries, physiology and intracoronary imaging are still underused, because the main barrier, more than economic and technical issues, is the persistence of confidence in the angio-guided approach by a significant number of operators4,5.
In the present issue of EuroIntervention, Huang et al present a retrospective analysis to evaluate the diagnostic performance of an optical coherence tomography (OCT)-based functional assessment (optical flow ratio [OFR])6.
The authors compared OFR with angio-based functional assessment, utilising fractional flow reserve (FFR) as standard. In the 212 vessels analysed from 181 patients, OFR showed significantly better correlation with FFR than quantitative flow ratio (QFR), both in myocardial infarction (MI) and in non-MI-related vessels6. At receiver operating characteristic (ROC) analysis, the area under the curve (AUC) in identifying physiologically significant stenosis was excellent (0.97; 95% CI: 0.93-0.99) for OFR, and higher than QFR (difference=0.05, p=0.017). Taken together, these results suggest that OFR could outperform QFR in predicting the FFR result, although the analysis is retrospective and non-conclusive about OCT-OFR superiority over QFR. First, the reported diagnostic accuracy of QFR in comparison with FFR is similar to the one shown by previous studies7. Second, an ongoing dedicated study has been designed with this aim, namely the FAVOR III EJ (Functional Assessment by Virtual Online Reconstruction III Europe Japan), which will provide a definitive answer regarding QFR non-inferiority to FFR in terms of clinical outcomes (NCT03729739).
The main advantage of OCT-OFR is to provide contemporary imaging and functional assessment of the instrumented vessel utilising only one tool. In particular, its main advantage is to provide a simultaneous and integrated imaging and functional reconstruction of the vessel. A single OCT-OFR scan permits the identification of the functional drops of the vessel, as already demonstrated with FFR pullback8 and, at the same time, associates the functional drop with imaging information (calcium, eccentric plaque, bifurcation, diameter, length, etc.). The main drawbacks of this technology are the poor worldwide penetration of OCT technology and the lack of demonstration of an additional clinical value as compared to the available tools, translating into uncertainty regarding its clinical application.
In the present paper, the authors included patients with a high a priori likelihood of PCI and suggest the same population as a target for its application. However, in the present analysis, around 60% of patients had a negative functional assessment and consequently did not receive PCI4. For this reason, the application of OCT-OFR is highly unlikely in a pre-PCI setting as an alternative to hyperaemic, resting and angio-based systems due to the high number of negative functional assessments that would make this strategy not cost-effective in most healthcare systems.
On the other hand, in the setting of complex high-risk and indicated procedures (CHIP), OCT-OFR could represent a game changer. The operator could use pre-PCI OCT information both to evaluate the need for atherectomy, laser or intravascular lithotripsy as well as to evaluate the sizing and length of the stent. In addition, pre-PCI OFR provides a physiological map of the vessel which is helpful when deciding how long to stent. Then, an OCT-OFR scan could be optimal for a meticulous procedural plan, and it could potentially predict the final functional result. Post-PCI OCT-OFR could confirm a good final result from both an imaging and a physiology point of view or, in case of a suboptimal functional result, it could permit a tailored optimisation thanks to the integration of imaging and physiology (Figure 1).
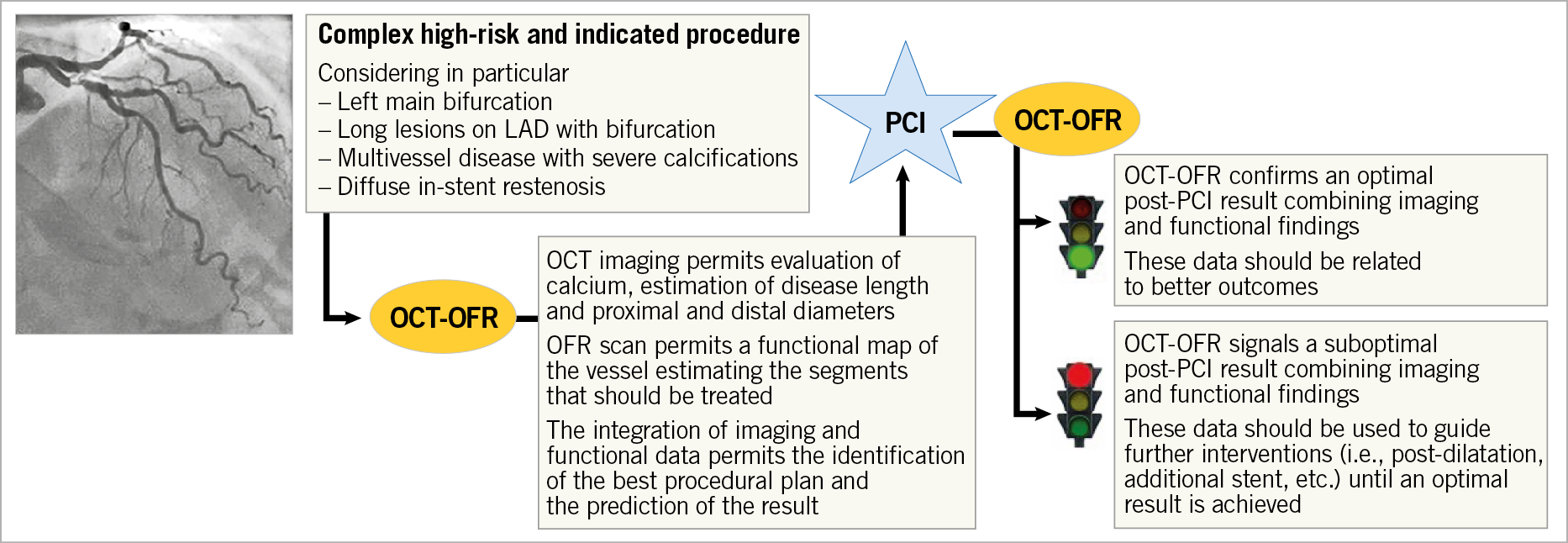
Figure 1. Implementation of OCT-OFR in a complex high-risk indicated procedure. LAD: left anterior descending; OCT: optical coherence tomography; OFR: optical flow ratio; PCI: percutaneous coronary intervention
Another interesting application could be in the evaluation of non-culprit lesions in patients with multivessel disease in the acute coronary syndrome setting. OCT may be helpful in the treatment of the culprit lesion, whereas OCT-OFR could be helpful to guide a functional complete revascularisation of non-culprit lesions.
Finally, OCT-OFR could be helpful in in-stent restenosis (ISR) evaluation, as suggested by the numerical differences, although not statistically significant, in this subset of patients in the present analysis6. OCT-OFR could be particularly helpful to combine imaging with physiology to ascertain the location and mechanism of ISR.
In summary, OCT-OFR is a promising technology. Currently, the main limitation of PCI practice is the low penetration of tools for intracoronary imaging and physiology, which have consistently been shown to improve patients’ outcome. All developments and efforts that may translate into a higher penetration of imaging- and/or physiology-guided PCI should be commended. Similarly, any tool that may optimise post-PCI outcome should be appreciated. This preliminary retrospective report suggests that OCT-OFR is probably better than QFR in predicting FFR. However, whether OCT-OFR can really increase the worldwide use of imaging/physio-guided PCI or improve post-PCI outcome remains to be determined, especially considering the non-negligible cost of OCT and the issues of reimbursement in some healthcare systems. Only future randomised clinical trials will permit an understanding of the real advantage of an OCT-OFR-based approach.
Conflict of interest statement
G. Campo has received research grants from AstraZeneca, Boston Scientific, Medis, SMT, and Siemens. S. Biscaglia has received research grants from Medis, SMT, and Siemens.
Supplementary data
To read the full content of this article, please download the PDF.