The current issue of EuroIntervention publishes a paramount article by Ding et al about the use of optical flow ratio (OFR) to guide percutaneous coronary interventions (PCI)1. In the Chinese year of the Ox, this study combining data from "Ox"-ford and Besançon is definitely an expression of the Chinese sense of humour. Nonetheless, a serious and relevant study is hidden behind that playful wink that might definitively designate optical coherence tomography (OCT) as the preferred tool for PCI guidance.
The inception of invasive computational physiology was outlined in 2014, in a shear stress study highlighting the importance of the outgoing flow through the side branches2. We realised that, in being able to calculate the complex loco-regional map of shear stress, the computation of the average fluid pressure throughout the vessel would be a piece of cake; "this information is clinically relevant for virtual fractional flow reserve (FFR) calculations on the basis of computational fluid dynamics and coronary imaging"2. The principle was initially tested in coronary angiography, thus resulting in the development of the quantitative flow ratio (QFR), and was recently improved to take into account the fractal geometry of the coronary tree3, the latter being a landmark of this research group from the very beginning2. OCT had to wait until 2019 for its own FFR computation, dubbed optical flow ratio (OFR). The computational algorithm was fine-tuned in retrospective data sets4 and the final OFR software was then simultaneously validated in a retrospective5 and pivotal prospective study6. The studies confirmed OFR as the most accurate computational method to date5,6, with a diagnostic accuracy of 93% when a dedicated acquisition protocol is applied6. OFR can overcome the classical limitations of angiography, like foreshortening, vessel overlap or calcification6, although it can be affected by cardiac motion artefact7.
Ding et al present a novel method of virtual stenting for OFR, dubbed simulated residual OFR (SR-OFR), and validate both SR-OFR and OFR post-PCI, versus the gold standard of wire-based FFR post-PCI. The only criticism is that a purported study of agreement should not simply consist of correlation and comparison of means, as this approach can be misleading (Figure 1). Nonetheless, Bland-Altman, scatter plots and additional analysis indirectly suggest that a proper analysis of agreement would not have substantially overturned the published conclusions in this case. The agreement between virtual stenting and final FFR is only moderate, akin to other studies predicting the effect of stenting8: predicted values pre-PCI tend to be higher than measured values post-PCI due to the residual in-stent pressure drop, which is assumed as zero in the predicted value1,8.
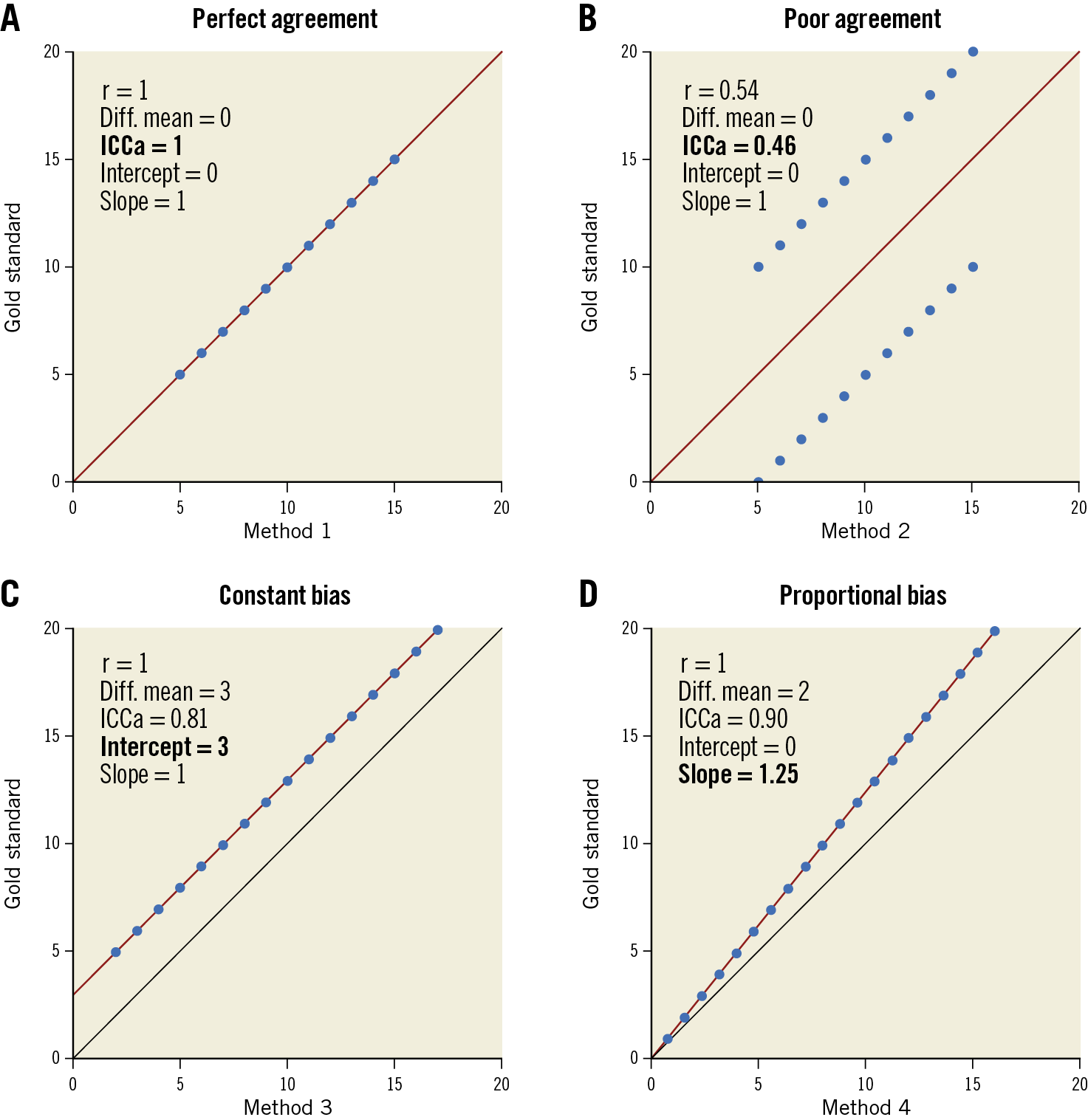
Figure 1. Assessment of agreement with a clear gold standard. Agreement is assessed in this example by ICCa. A) shows an example of perfect agreement. Notice how methods with poor agreement can have paired difference of means = 0 (B) or Pearson’s r = 1. C) & D) Linear regression can assess constant and proportional bias, defined as deviation of the intercept from 0 and of the slope from 1, respectively. Diff. mean: paired difference of means; ICCa: intraclass correlation coefficient for the absolute value; r: Pearson`s correlation coefficient
We had foreseen that OFR would be "particularly interesting for the assessment of lesions with a high a priori likelihood of PCI"6, especially in countries (e.g., Germany) where only a single adjuvant tool for PCI is reimbursed. Operators often face the dilemma of choosing between FFR wires for decision making, or imaging for PCI guidance and optimisation. The current study aids in overcoming that dilemma, proposing OCT as a one-stop-shop that provides both physiology and imaging, while also incorporating the possibility of planning PCI with OFR virtual stenting1. The dilemma is hence over, as no other single adjuvant tool can offer such a comprehensive appraisal.
In summary, in this Year of the Ox (Niu, in Mandarin), this study provides us with “niu” evidence that definitely tips the balance in favour of OCT as the preferred tool for PCI guidance, combining the advantages of accurate OFR physiology and high-definition imaging. The challenge still lies in surmounting the evidence-reality mismatch concerning imaging and physiology in the real world, which will require action from both cardiologists and economy managers9.
Conflict of interest statement
The author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.