Abstract
Aims: We aimed to assess the impact of B-type natriuretic peptide (BNP) on short-term outcomes in patients undergoing transcatheter aortic valve implantation (TAVI).
Methods and results: Of 500 consecutive patients with severe aortic stenosis undergoing TAVI at our institution, we studied 340 patients who had a BNP assessment prior to TAVI. Patients were divided into tertiles - low: BNP ≤201 pg/mL (n=114), mid: BNP 202-595 pg/mL (n=113) and high: BNP ≥596 pg/mL (n=113). The primary endpoint was all-cause mortality, cardiac death and major adverse cardiac and cerebrovascular events (MACCE; death, major stroke and myocardial infarction) at 30 days. Compared with low tertile, high tertile patients were at higher baseline surgical risk (STS score 5.5±3.0 vs. 7.4±4.1, p=0.002). On echocardiography, high tertile patients had smaller valve areas (0.74±0.21 vs. 0.66±0.23 cm2, p=0.008), higher left ventricular (LV) mass indices (123.40±33.66 vs. 168.22±47.96 g/m2, p<0.001) and lower LV ejection fractions (61.59±7.18 vs. 42.65±15.41%, p<0.001) as compared with low tertile patients. At 30 days, a significantly higher incidence of death (hazard ratio [HR] 7.41, p=0.001) cardiac death (HR 5.82, p=0.006) and MACCE (HR 9.04, p<0.001) was observed among high as compared to low tertile patients.
Conclusions: In TAVI patients, higher BNP values at baseline are associated with an increased risk for an adverse event periprocedurally and after 30 days, respectively.
Introduction
Transcatheter aortic valve implantation (TAVI) is a disruptive technology that has transformed the management of inoperable patients with severe symptomatic aortic stenosis1. It is also a viable alternative to surgical aortic valve replacement (SAVR) among patients at high operative risk2. Patient selection is crucial to the success of this procedure, and an important component of this process is appropriate risk assessment3. To date, risk algorithms used to predict outcomes following cardiac surgical procedures have been found largely to overestimate the procedural risk of TAVI due to suboptimal discrimination and calibration4. Hence, there is an unmet clinical need for variables that may further help to predict patient risk accurately. Recent reports have identified a number of baseline variables associated with mortality in patients undergoing TAVI, including low body mass5, left ventricular dysfunction6, low-flow, low-gradient severe aortic stenosis7, chronic obstructive pulmonary disease8 and natriuretic peptides9,10. B-type natriuretic peptide (BNP) is released by the heart in response to pressure and volume overload11. Among patients undergoing SAVR, BNP was found to predict postoperative survival12. Whether or not BNP predicts adverse events following TAVI is controversial9,10. Therefore, the aim of this study was to determine whether pre-procedural (baseline; BL) BNP was associated with adverse clinical outcomes in the short term following TAVI.
Methods
PATIENT POPULATION
We performed a retrospective analysis of prospectively collected data within a dedicated database that included all patients with severe native valve aortic stenosis (AS) (indexed AVA [iAVA]) ≤0.6 cm2/m2 or mean gradient [MG] >40 mmHg), who underwent TAVI at Bern University Hospital between August 2007 and April 2012 (n=500). All patients were deemed inoperable or at high surgical risk for conventional surgical aortic valve replacement by a multidisciplinary team comprising interventional cardiologists and cardiac surgeons. Patient flow is shown in Figure 1. Those included in this study were all consecutive patients with symptomatic severe native valve AS (iAVA ≤0.6 cm2 and/or MG >40 mmHg) undergoing TAVI who had a BNP sample taken within seven days prior to TAVI (n=340). Patients were subdivided into the following tertiles:
Group 1: low BNP tertile (0-201 pg/mL) (n=114)
Group 2: mid BNP tertile (>201-595 pg/mL) (n=113)
Group 3: high BNP tertile (>595 pg/mL) (n=113)
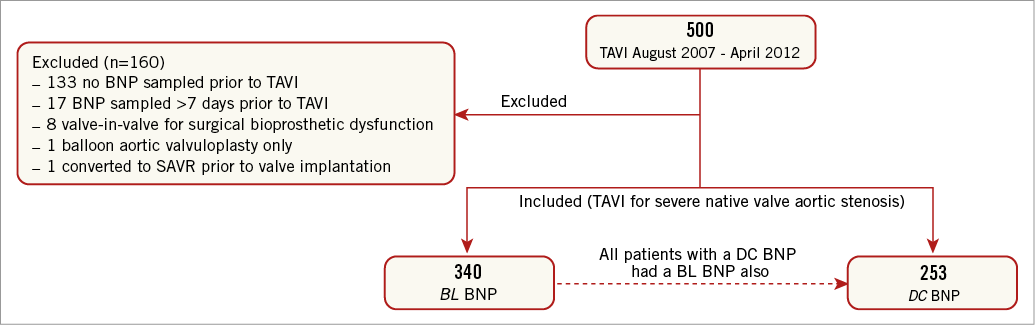
Figure 1. Patient flow. TAVI: transcatheter aortic valve implantation; SAVR: surgical aortic valve replacement; BNP: B-type natriuretic peptide; BL: baseline; DC: discharge
BNP SAMPLES
Blood samples for BNP were drawn from the antecubital vein into chilled EDTA acid test tubes at the time of admission prior to TAVI (mean 1.5±1.3 days, range 0-7 days; baseline) and on the day of hospital discharge (6.3±2.8 days post TAVI, range 1-23 days post TAVI). BNP levels were determined at baseline (n=340) and discharge (n=253) from an EDTA blood sample using a chemiluminescent microparticle immunoassay (CMIA) (ARCHITECT BNP assay; Abbott Laboratories Diagnostics Division, Abbott Park, IL, USA).
TRANSTHORACIC ECHOCARDIOGRAPHY
Baseline transthoracic two-dimensional echocardiography was performed using commercially available ultrasound systems (Vivid 7 and E9; GE Medical Systems, Horten, Norway). Left ventricular (LV) assessment was performed as recommended and LV mass calculated using the Devereux formula and indexed to body surface area13. Mitral, aortic and tricuspid valve regurgitation were evaluated using spectral and colour Doppler images and semiquantitatively graded as mild, moderate and severe, as recommended14. Aortic valve area was assessed using the continuity equation and indexed to the body surface area15. Mean valve gradient was measured using continuous wave Doppler acquisitions in the apical 5-chamber view15.
TAVI PROCEDURE
TAVI was performed using standard techniques as previously described16. Vascular access was transfemoral using the Medtronic CoreValve Revalving System (MCRS) (Medtronic, Inc., Minneapolis, MN, USA) or the Edwards SAPIEN valve (ESV) (Edwards Lifesciences, Irvine, CA, USA), transapical for the ESV or trans-subclavian using the MCRS.
CLINICAL FOLLOW-UP
Adverse events were assessed in hospital, and regular clinical follow-up was performed. All suspected events were adjudicated by an unblinded clinical events committee comprising a cardiac surgeon and an interventional cardiologist. Baseline clinical and procedural characteristics and all follow-up data were entered into a dedicated database, held at an academic clinical trials unit (CTU Bern, Bern University Hospital, Bern, Switzerland) responsible for central data audits and maintenance of the database.
DEFINITIONS
Clinical endpoints were defined according to the criteria proposed by the Valve Academic Research Consortium (VARC)17.
STUDY ENDPOINTS
The primary endpoint was all-cause mortality, cardiovascular death and major adverse cardiovascular and cerebrovascular events (MACCE) (composite of all-cause mortality, major stroke and myocardial infarction) at 30 days. Secondary endpoints included cerebrovascular events (major stroke, minor stroke, transient ischaemic attack) and myocardial infarction at 30 days.
STATISTICS
Continuous data are presented as means±standard deviations (SD), and categorical variables are depicted as percentages and numbers. Categorical variables were compared by means of the chi-square test (or Fisher’s test for two-group comparisons), and continuous variables were compared using ANOVA (or unpaired t-test for two-group comparisons). P-values for a trend across the BNP tertiles were calculated using regression (normally distributed variables), logistic regression (binomial variables) or multinomial regression (categorical variables with three or more categories) analysis. BNP was compared before and after TAVI using the paired samples t-test. Time-to-first event data were analysed using Cox’s regression testing for a trend across the three tertiles, and presented with the Harrell’s concordance statistic (c-index). In case two tertiles had no event, only a p-value from a Fisher’s exact test was calculated. All p-values and 95% confidence intervals (CIs) are two-sided. Two-sided p-values <0.05 were considered statistically significant. All analyses were performed with STATA, version 12 (StataCorp, College Station, TX, USA).
Results
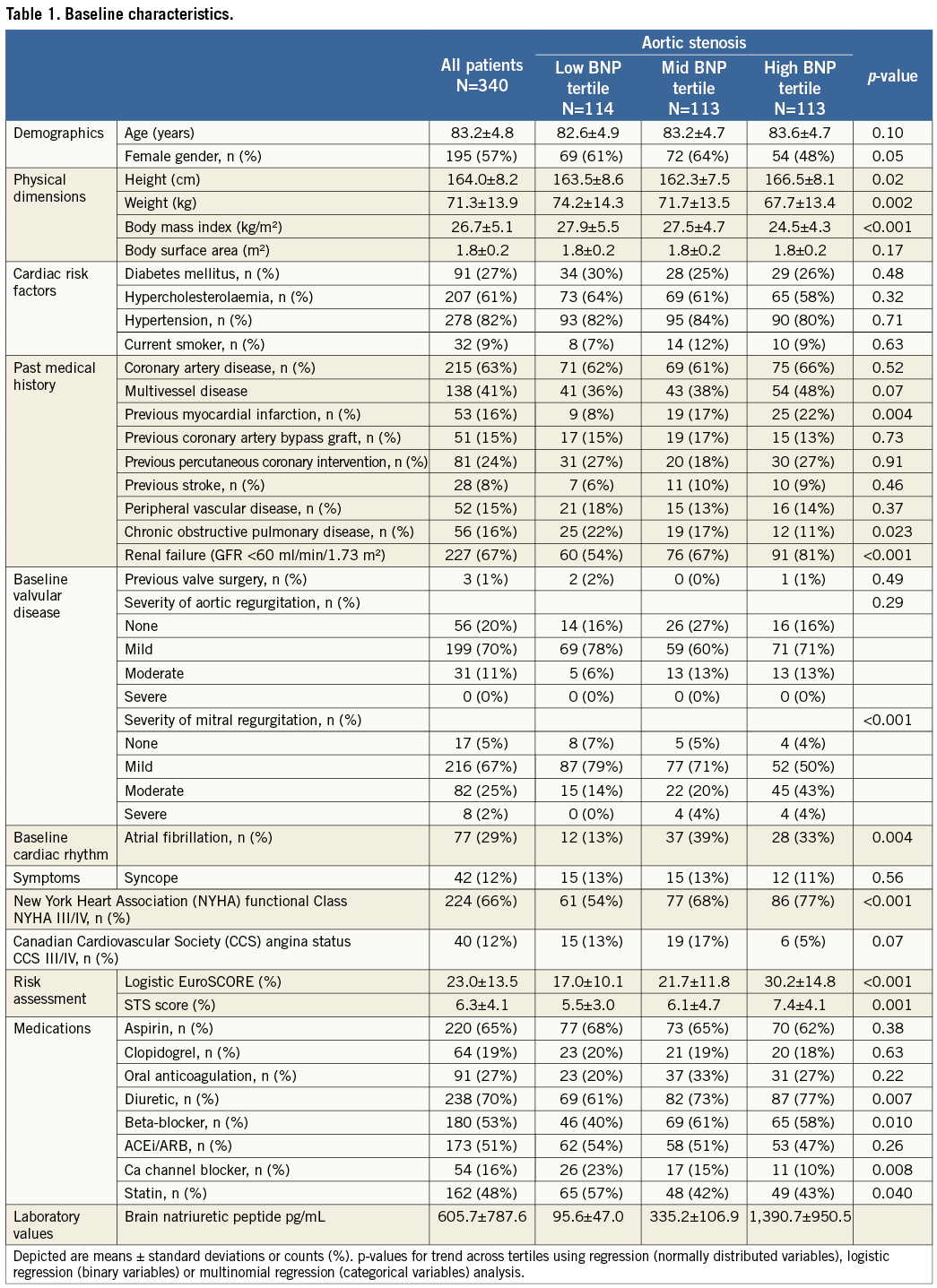
PATIENT CHARACTERISTICS
Baseline characteristics of the patient population are shown in Table 1. Mean age was 83.2±4.8 years and there was an observed trend towards more males in the high as compared with the mid BNP tertile group. As compared with the low BNP tertile group, mid and high BNP tertile groups had a significantly higher incidence of previous myocardial infarction, renal failure, moderate mitral regurgitation, atrial fibrillation, NYHA Class III/IV symptoms and logistic EuroSCORE. The mean (±standard deviation) BNP values were 95.6±47.0, 335.2±106.9 and 1,390.7±950.5 pg/mL in the low, mid and high BNP tertile groups, respectively.
TRANSTHORACIC ECHOCARDIOGRAPHIC CHARACTERISTICS
The transthoracic echocardiographic characteristics of the patient population are shown in Table 2. As compared with the low BNP tertile group, high BNP tertile patients had significantly smaller aortic valve areas, lower LV ejection fractions, higher LV mass indices and larger LV cavities.
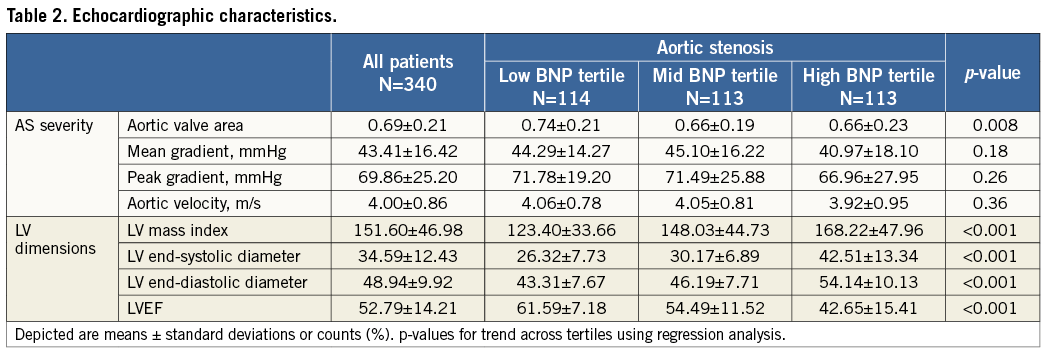
PROCEDURAL CHARACTERISTICS
Procedural characteristics are shown in Table 3. All patients underwent TAVI using either the Medtronic CoreValve (n=309 [63%]) or Edwards SAPIEN (n=127 [37%]) prosthesis via the transfemoral (n=309 [91%]), transapical (n=27 [8%]) or trans-subclavian (n=4 [1%]) route. High BNP tertile patients were significantly more likely to receive the Medtronic CoreValve as compared to low BNP tertile patients. In total 29% of patients underwent either staged or concomitant revascularisation. Overall device success was 85% and absence of device success was mainly due to the presence of aortic regurgitation ≥2+ but not because of a failure to implant the device successfully.
CHANGE IN BNP BEFORE AND AFTER TAVI
A significant reduction in BNP (baseline 538.94±701.16 vs. discharge 387.89±455.58 pg/mL, p<0.0001) was observed following TAVI (Figure 2).
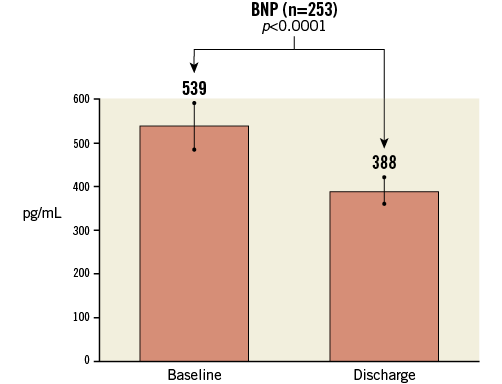
Figure 2. Mean decrease in B-type natriuretic peptide (BNP) following transcatheter aortic valve implantation among the 253 patients with both a baseline and a discharge BNP value available.
CLINICAL OUTCOMES
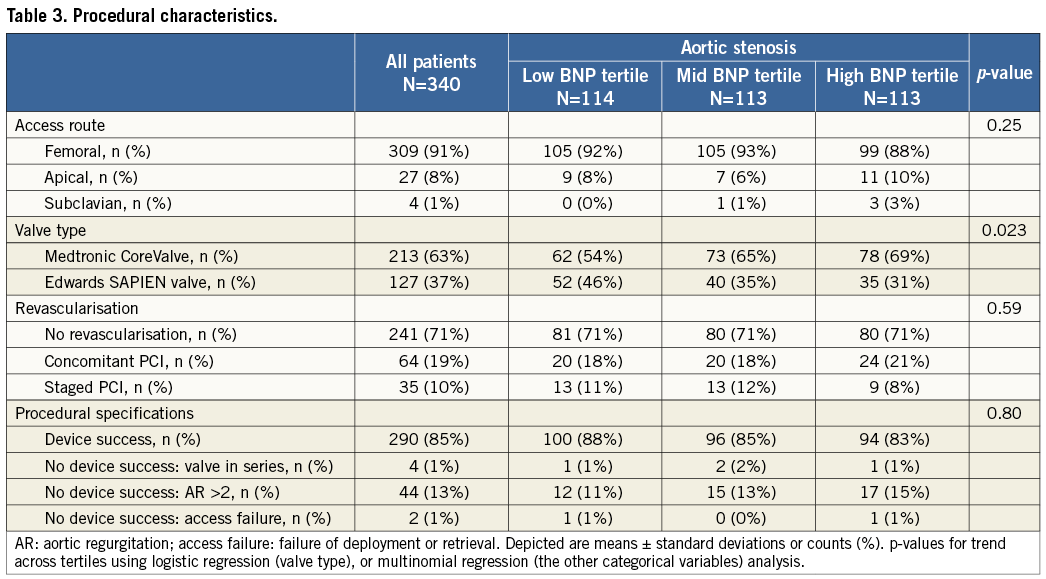
Event rates with hazard ratios (HR) for all major clinical endpoints at 30 days are provided in Table 4.
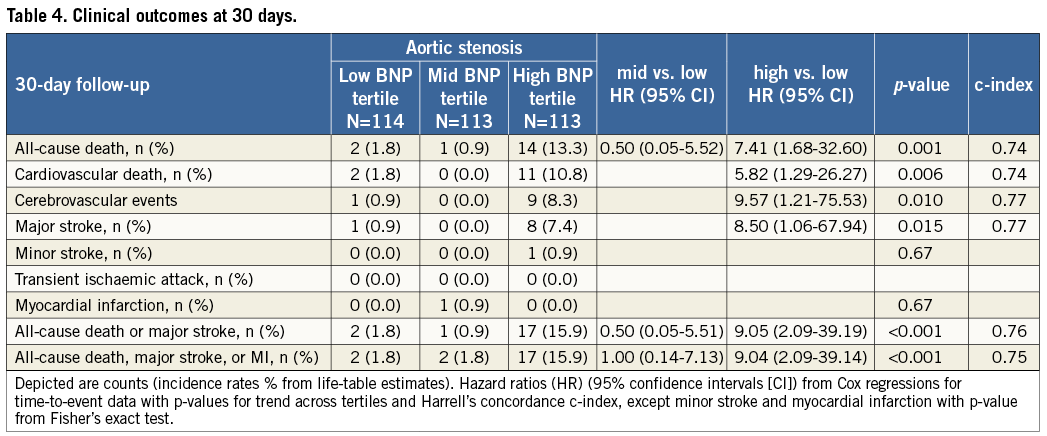
PRIMARY ENDPOINT AT 30 DAYS
As compared with the low BNP tertile group, high BNP tertile patients had a significantly higher incidence of all-cause (hazard ratio [HR] 7.41, 95% confidence interval [CI]: 1.68-32.60, p=0.001) and cardiac (HR 5.82, 95% CI: 1.29-26.27, p=0.006) mortality at 30 days. In addition, there was a significantly higher incidence of MACCE among high BNP tertile patients as compared to low BNP tertile patients (HR 9.04, 95% CI: 2.09-39.14, p<0.001) (Figure 3).
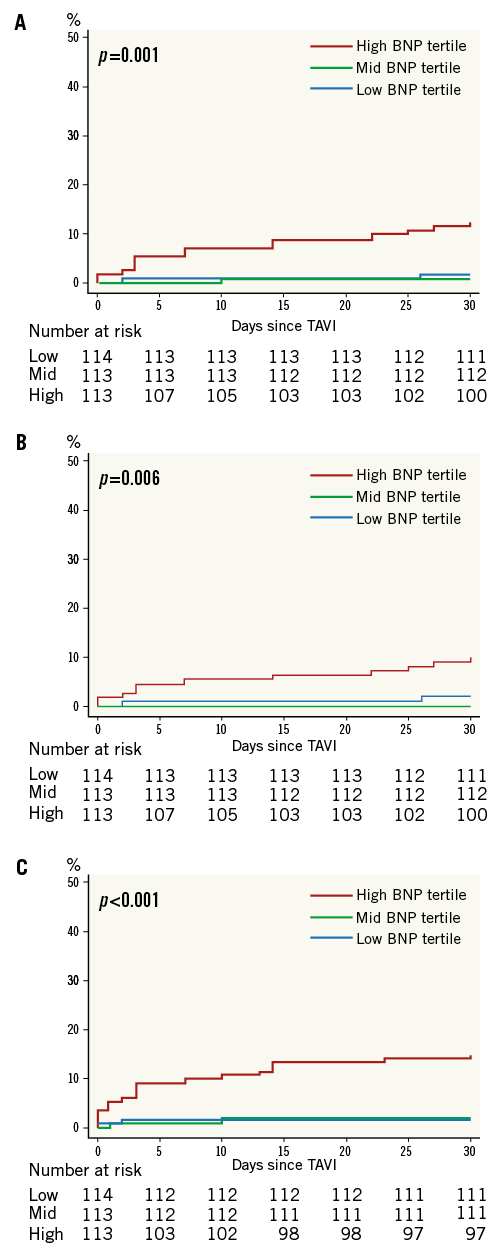
Figure 3. Kaplan-Meier analysis of death (A), cardiac death (B) and major adverse cardiovascular and cerebrovascular events (MACCE; composite of death, major stroke, and myocardial infarction) (C) at 30 days. Low B-type natriuretic peptide (BNP) tertile=0-201 pg/mL; mid BNP tertile >201-595 pg/mL; high BNP tertile >595 pg/mL. TAVI: transcatheter aortic valve implantation
SECONDARY ENDPOINT AT 30 DAYS
High BNP tertile patients had a significantly higher incidence of cerebrovascular events (HR 9.57, 95% CI: 1.21-75.53, p=0.01), which was largely driven by a higher incidence of major strokes (HR 8.50, 95% CI: 1.06-67.94, p=0.015). No significant differences in the rates of myocardial infarction were observed between groups.
Discussion
The main results of this study can be summarised as follows. First, baseline BNP levels correlated with patient risk profiles, with high tertile BNP patients having a higher incidence of previous myocardial infarction, moderate mitral regurgitation, atrial fibrillation and higher logistic EuroSCORE and STS scores. Second, there were significant correlations between baseline BNP levels and pre-interventional echocardiographic indices. Patients in the high BNP tertile had smaller valve areas, higher LV mass indices, larger LV cavity sizes and lower LV ejection fractions on echocardiography. Third, a significant reduction in BNP was observed following the TAVI procedure. Finally, high BNP tertile patients had a significantly higher incidence of death, cardiac death, MACCE and cerebrovascular events, including major stroke at 30 days.
PREVIOUS STUDIES
To date, there have been just two studies assessing the impact of BNP on clinical outcomes after TAVI, and these have shown conflicting results9,10. Kefer et al assessed the usefulness of BNP to predict outcomes among 58 patients undergoing either transfemoral (n=34) or transapical (n=24) TAVI with the Edwards SAPIEN valve only9. They found that both baseline and 24-hour BNP were independent predictors of 30-day survival. The present study corroborates these findings in a larger population of patients undergoing TAVI with both the Edwards SAPIEN valve and the Medtronic CoreValve. In addition, we have further extended these findings by demonstrating that baseline BNP is also associated with cardiac death, MACCE, cerebrovascular events and major stroke. More recently, Ben-Dor et al reported that a high BNP level in high-risk patients with severe AS was not an independent marker for higher mortality but that it did reflect heart failure status10. However, this study was limited by the fact that just over one-third of included patients (105/289 [36%]) actually underwent TAVI with the Edwards SAPIEN valve only, with the rest of the study population undergoing either balloon aortic valvuloplasty (n=127), SAVR (n=25) or medical therapy (n=32)10. Conversely, all patients in the present larger study underwent TAVI with either the Edwards SAPIEN or the Medtronic CoreValve.
CLINICAL IMPLICATIONS
BNP is a dynamic biomarker and the value can vary depending on the volume status of the patient. Because our findings suggest that an elevated BNP is associated with a higher 30-day mortality rate, further studies are required to assess whether optimising the volume status of patients in decompensated heart failure prior to TAVI (e.g., using diuretics) may reduce BNP and lead to improved clinical outcomes.
Limitations
First, the present study reports the experience of a single centre only. Second, while the time interval between BNP sampling and TAVI was ≤7 days (mean 1.5±1.3 days), the interval between biomarker sampling and pre-procedural echocardiography was considerably longer (22.2±30.6 days). Third, not all patients undergoing TAVI during the study period had a BNP sampled and therefore this is not a consecutive patient series. In addition, not all patients who had a baseline BNP had a discharge BNP. However, all patients who had a discharge BNP had a baseline BNP available. Finally, BNP levels could be higher in patients with chronic renal impairment11.
Conclusions
Higher BNP values are associated with elevated pre-procedural risk and poorer LV function. An elevated baseline BNP is associated with a higher incidence of death, cardiac death and MACCE at 30 days.
Conflict of interest statement
S. Windecker has received research contracts to the institution from Abbott, Boston Scientific, Biosensors, Cordis, Medtronic and St. Jude. P. Wenaweser has received honoraria and lecture fees from Medtronic and Edwards Lifesciences. C.J. O’Sullivan is the recipient of a research grant from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the European Society of Cardiology (ESC). The other authors have no conflicts of interest to declare.

