Abstract
Aims: The aim of this study was to assess the clinical value of biomarkers to identify TAVI patients at high risk for adverse outcome, to assess whether these biomarkers provide prognostic information beyond that of established clinical risk scores, and to assess whether a combined multi-marker strategy can improve clinical decision making.
Methods and results: In 683 TAVI patients, biomarkers reflecting various pathophysiologic systems were measured before TAVI. The primary endpoint was one-year all-cause mortality. Other outcomes were recorded according to the VARC-2 criteria. Thirty-day and one-year mortality was 2.9% and 12.0%, respectively. Non-survivors at one year had higher risk scores and increased median biomarker levels. Logistic EuroSCORE in combination with hs-CRP had the highest predictive value for 30-day (AUC 0.740 [95% CI: 0.667-0.812], p=0.1117) and one-year mortality (AUC 0.631 [95% CI: 0.569-0.693], p=0.0403). In multivariate regression analysis, logistic EuroSCORE in combination with hs-CRP showed the strongest association with one-year mortality. Combinations of increasing medians of logistic EuroSCORE results and hs-CRP levels allowed the stratification of the TAVI patients into subgroups with one-year mortality rates ranging from 6.6% up to 18.2%.
Conclusions: hs-CRP alongside the logistic EuroSCORE was an independent predictor of one-year all-cause mortality in TAVI patients. A combination of both might help to predict procedural risk and outcome better.
Abbreviations
EuroSCORE: European System for Cardiac Operative Risk Evaluation
hs-CRP: high-sensitivity C-reactive protein
STS-PROM: Society of Thoracic Surgeons Predicted Risk of Mortality
VARC: Valve Academic Research Consortium
Introduction
Although surgical aortic valve replacement (SAVR) still remains the gold standard for patients with severe symptomatic aortic stenosis (AS), transcatheter aortic valve implantation (TAVI) has emerged as the treatment of choice for many patients at increased surgical risk1-3. Currently, interdisciplinary Heart Teams base their treatment choice on the expected perioperative or in-hospital mortality as calculated by predictive risk algorithms such as the logistic EuroSCORE, the EuroSCORE II and the Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) score. These scoring systems, however, were developed for use in surgical patients only; their applicability for TAVI patients is questionable as they are strongly based on certain comorbidities that are related to outcome in standard surgical risk populations4 but do not address the particularities influencing outcome in TAVI procedures. Attending physicians are hence recognising the need to establish a reliable and standardised decision-making process specifically designed to address the particularities of TAVI procedures as opposed to SAVR. At present, different attempts with varying success have been made to develop clinical risk scores tailored to TAVI patients, e.g., the German Aortic Valve (GAV) score5 and the recently developed STS/ACC-TAVR risk score6. Others have tried to use cardiac biomarkers as diagnostic parameters for risk stratification in AS patients7,8. Especially for “next-generation” transcatheter heart valves (THV), there are only scarce data about the role of biomarkers in predicting prognosis in TAVI patients and about their significance compared to established risk scores. Although these approaches were able to show some promising initial results, to date no fully validated and reliable risk assessment strategy exists for patients scheduled for TAVI.
The aim of the present study was to determine whether circulating biomarkers representing different pathophysiologic systems, such as renal function (creatinine), inflammatory response (high-sensitivity C-reactive protein [hs-CRP]), haemodynamic stress (NT-proBNP), and myocardial necrosis and ischaemia (hs-troponin I), could be used to identify TAVI patients at higher risk for adverse clinical outcomes, to assess whether these provide prognostic information beyond that of established predictive risk algorithms in a TAVI patient cohort treated with the most recent THV device, and to explore how risk prediction by clinical risk scores could be combined appropriately with biomarker measurement for risk stratification.
Methods
STUDY PROTOCOL
Between January 2014 and August 2017, 683 consecutive patients suffering from severe, symptomatic AS underwent TAVI at our institution, and were included in this observational study. The present study complies with the Declaration of Helsinki and was approved by the local ethics committee of the University of Bonn. Written informed consent was obtained from all patients.
Before TAVI, the diagnosis of severe AS was confirmed by transthoracic echocardiography according to the current guidelines of the European Society of Cardiology. The procedure was performed as previously described9. Blood samples were obtained the evening before the TAVI procedure within a given period of time between 17:00 hrs and 20:00 hrs. Each measurement was part of the routine laboratory assessment and performed immediately after blood collection. No single sample was missing.
hs-CRP levels did not have any influence over whether or not a patient was recommended to undergo TAVI. However, in case of elevated hs-CRP, the appropriate measure was taken to exclude an acute and active inflammation in these patients and anti-bacterial therapy was started, if indicated.
The primary endpoint of the present study was one-year all-cause mortality. Other outcomes were recorded according to the VARC-2 criteria. Follow-up data were collected during routine outpatient visits, from hospital discharge letters, or via telephone interviews with the referring cardiologists or primary care physicians.
Calculation of mortality according to clinical scoring systems is shown in Supplementary Appendix 1. Analysis of biomarkers is shown in Supplementary Appendix 2.
STATISTICAL ANALYSIS
Data are given as mean±standard deviation if normally distributed, or as median and interquartile range if not normally distributed. Continuous variables were tested for normal distribution with the Kolmogorov-Smirnov test. For comparison between two groups, a Student’s t-test was performed for continuous variables if normally distributed, and a Mann-Whitney U test was performed for continuous variables if not normally distributed. When comparing more than two groups, ANOVA or the Kruskal-Wallis test was used. Categorical variables are given as frequencies and percentages. For categorical variables, the χ2 test was used for further analysis.
Associations of the logistic EuroSCORE/biomarkers with the primary endpoint were assessed by univariate and multivariate Cox regression analyses. To limit the influence of extreme observations, biomarker values were indicated as per 1 SD (standard deviation) increase. In order to identify independent predictors of cumulative mortality, as a first step logistic EuroSCORE, creatinine, hs-CRP, NT-proBNP and hs-troponin I were included in a univariate regression analysis. Predictors with p≤0.05 on univariate analysis were entered in a stepwise multivariate logistic regression model. We determined the area under the curve (AUC) by using receiver operating characteristic (ROC) curve analysis to assess the discriminatory performance of risk scores and individual biomarkers.
The unadjusted cumulative event rates were estimated by the Kaplan-Meier method, and statistical assessment was performed by the log-rank-test. For this, biomarker levels and risk score results were categorised into tertiles (all results as follows: Q1 vs. Q2 vs. Q3): logistic EuroSCORE: ≤10.89% vs. 10.89-20.15% vs. >20.15%; creatinine: ≤1.00 mg/dL vs. 1.00-1.40 mg/dL vs. >1.40 mg/dL; hs-CRP: ≤2.60 mg/L vs. 2.60-8.20 mg/L vs. >8.20 mg/L; NT-proBNP: ≤1,515.00 pg/mL vs. 1,515.00-3,928.00 pg/mL vs. >3,928.00 pg/mL; hs-troponin I: ≤0.02 ng/mL vs. 0.02-0.04 ng/mL vs. >0.04 ng/mL. To allow risk stratification into subgroups, both logistic EuroSCORE and hs-CRP levels were stratified according to the median.
Statistical significance was assumed when the null hypothesis could be rejected at p<0.05. Statistical analyses were conducted with PASW Statistics, Version 22.0 (IBM Corp., Armonk, NY, USA) and MedCalc version 11.6.1.0 (MedCalc Software, Mariakerke, Belgium). The investigators initiated the study, had full access to the data, and wrote the manuscript. All authors vouch for the accuracy and completeness of the data and all analyses, and confirm that the study was conducted according to the protocol.
Results
BASELINE CHARACTERISTICS
Baseline characteristics are summarised in Supplementary Table 1. The study cohort was, on average, 81 years (80.8±6.0 years) old, and 48.9% of the patients enrolled were male. All patients suffered from severe AS with an average aortic valve area (AVA) of less than 1 cm2 (0.72±0.16 cm2) and a mean gradient >40 mmHg (41.7±15.1 mmHg).
In patients who presented with elevated hs-CRP levels above the median (>4.4 mg/L), a high prevalence of classic cardiovascular risk factors such as overweight, diabetes, atrial fibrillation, chronic obstructive pulmonary disease (COPD), pulmonary hypertension, impaired left ventricular ejection fraction and renal failure could be demonstrated (Supplementary Table 2).
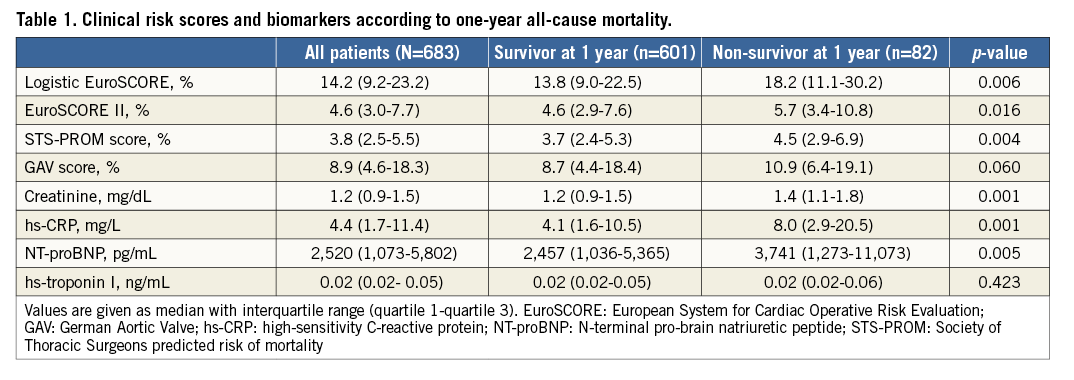
Patients who died within the first year following TAVI presented with significantly higher median clinical risk score results (non-survivors vs. survivors – logistic EuroSCORE: 18.2 [11.1-30.2]% vs. 13.8 [9.0-22.5]%, p=0.006; EuroSCORE II: 5.7 [3.4-10.8]% vs. 4.6 [2.9-7.6]%, p=0.016; STS-PROM: 4.5 [2.9-6.9]% vs. 3.7 [2.4-5.3]%, p=0.004; GAV score: 10.9 [6.4-19.1]% vs. 8.7 [4.4-18.4]%, p=0.060) and increased median biomarker levels (creatinine: 1.4 [1.1-1.8] mg/dL vs. 1.2 [0.9-1.5] mg/dL, p=0.001; hs-CRP: 8.0 [2.9-20.5] mg/L vs. 4.1 [1.6-10.5] mg/L, p=0.001; NT-proBNP: 3,741 [1,273-11,073] pg/mL vs. 2,457 [1,036-5,365] pg/mL, p=0.005) compared to those who did not (Table 1).
PERIPROCEDURAL CHARACTERISTICS
Periprocedural characteristics of the study cohort are shown in Supplementary Table 3. Ninety-nine percent (99.0%) of the patients underwent TAVI via the transfemoral route.
Patients who died within the first year following TAVI had to undergo conversion to open heart surgery at a significantly higher rate (2.4% vs. 0.0%, p<0.001).
CLINICAL OUTCOMES
Clinical outcomes are summarised in Supplementary Table 4. In our study cohort, 30-day and one-year all-cause mortality was 2.9% (20/683) and 12% (82/683), respectively. Furthermore, post-procedural stroke (4.9% vs. 1.3%, p=0.022), myocardial infarction (3.7% vs. 0.0%, p<0.001) and acute kidney injury (24.4% vs. 5.0%, p<0.001), irrespective of the degree, occurred more frequently in patients who died within the first year following TAVI.
When biomarkers were categorised into tertiles, values in the uppermost tertile for each biomarker were all significantly associated with increased one-year all-cause mortality except for hs-troponin I (Q3 vs. Q2 vs. Q1 - creatinine: 18.4% vs 10.7% vs. 7.7%, p=0.002; hs-CRP: 17.9% vs. 10.0% vs. 8.3%, p=0.004; NT-proBNP: 17.6% vs. 7.9% vs. 10.5%, p=0.004; hs-troponin I: 13.4% vs. 12.8% vs. 11.1%, p=0.707). Moreover, a logistic EuroSCORE result in the uppermost tertile was also associated with significantly increased one-year all-cause mortality (15.9% vs. 11.8% vs. 8.3%, p=0.047) (Figure 1A-Figure 1E).
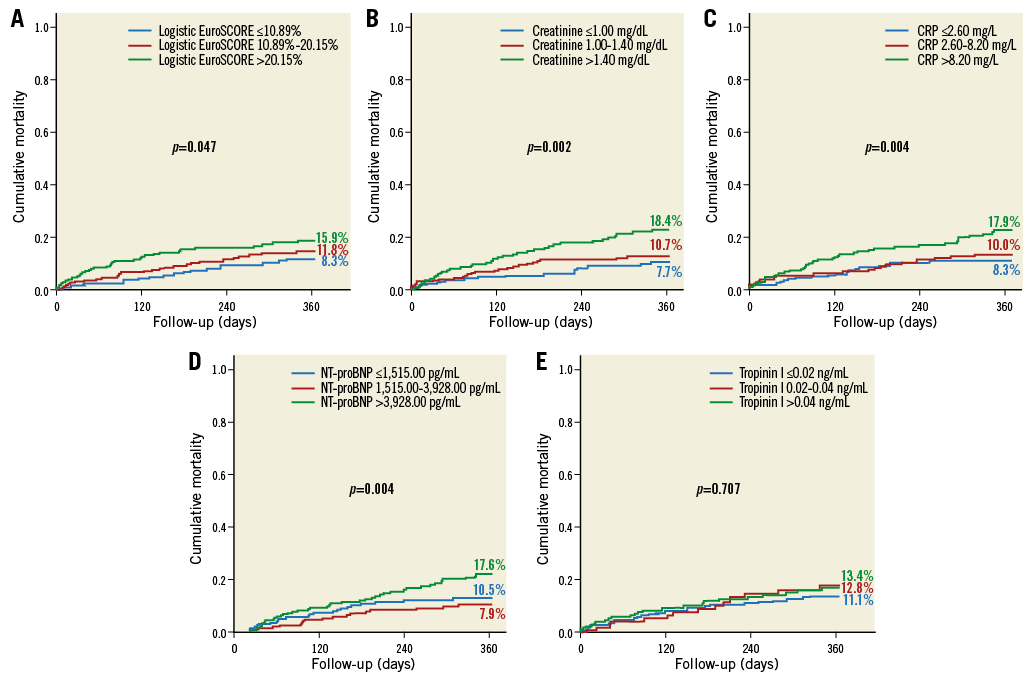
Figure 1. The association between one-year all-cause mortality and values stratified into tertiles for logistic EuroSCORE and each biomarker. A) Logistic EuroSCORE. B) Creatinine. C) hs-CRP. D) NT-proBNP. E) hs-troponin I. Values in the uppermost tertile were all significantly associated with increased one-year all-cause mortality except for hs-troponin I.
PREDICTORS OF CUMULATIVE MORTALITY
Univariate regression analysis (based on the hazard ratios per 1 SD increase) revealed that the surgical risk scores (logistic EuroSCORE: HR 1.380 [1.153-1.652], p<0.001; EuroSCORE II: HR 1.338 [1.177-1.520], p<0.001; STS-PROM score: HR 1.364 [1.202-1.547], p<0.001) and hs-CRP (HR 1.171 [1.016-1.349], p=0.030) were associated with an increased risk for cumulative one-year mortality (Supplementary Table 5, Figure 2A). The logistic EuroSCORE (HR 1.367 [1.144-1.635], p=0.001) and hs-CRP (HR 1.161 [1.002-1.345], p=0.047) also remained independent predictors in multivariate analysis and showed the strongest associations with one-year all-cause mortality (Supplementary Table 5, Figure 2B).
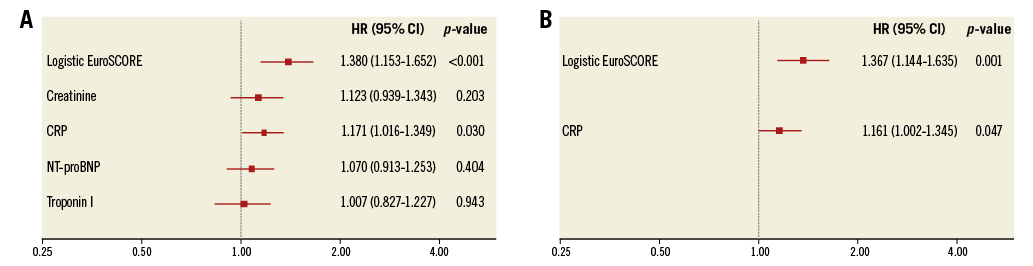
Figure 2. Forest plots for the prediction of one-year mortality. A) Univariate regression analysis, based on the hazard ratios per 1 SD increase, revealed that logistic EuroSCORE and hs-CRP were associated with an increased risk for cumulative one-year mortality. B) Multivariate analysis also showed a strong association with one-year all-cause mortality for logistic EuroSCORE and hs-CRP.
PROGNOSTIC VALUE OF BIOMARKERS AND CLINICAL RISK SCORES IN PREDICTING CUMULATIVE SHORT-TERM AND MIDTERM ALL-CAUSE MORTALITY
For the prediction of 30-day all-cause mortality, ROC curve analysis showed that the logistic EuroSCORE (AUC 0.672 [95% CI: 0.561-0.783]) had a better predictive value than the tested biomarkers (creatinine: AUC 0.560 [95% CI: 0.437-0.683], p=0.1801; hs-CRP: AUC 0.643 [95% CI: 0.518-0.768], p=0.7814; NT-proBNP: AUC 0.532 [95% CI: 0.395-0.669], p=0.0914; hs-troponin I: AUC 0.530 [95% CI: 0.393-0.667], p=0.1234). The combination of logistic EuroSCORE and hs-CRP offered a slight improvement in model performance with the highest overall AUC for the prediction of the procedural result in the form of 30-day all-cause mortality (AUC 0.740 [95% CI: 0.667-0.812], p=0.1117), and also had significant added value for the prediction of one-year all-cause mortality (AUC 0.631 [95% CI: 0.569-0.693], p=0.0403) (Table 2). Different combinations of logistic EuroSCORE and the other biomarkers did not result in an advantage (data not shown).
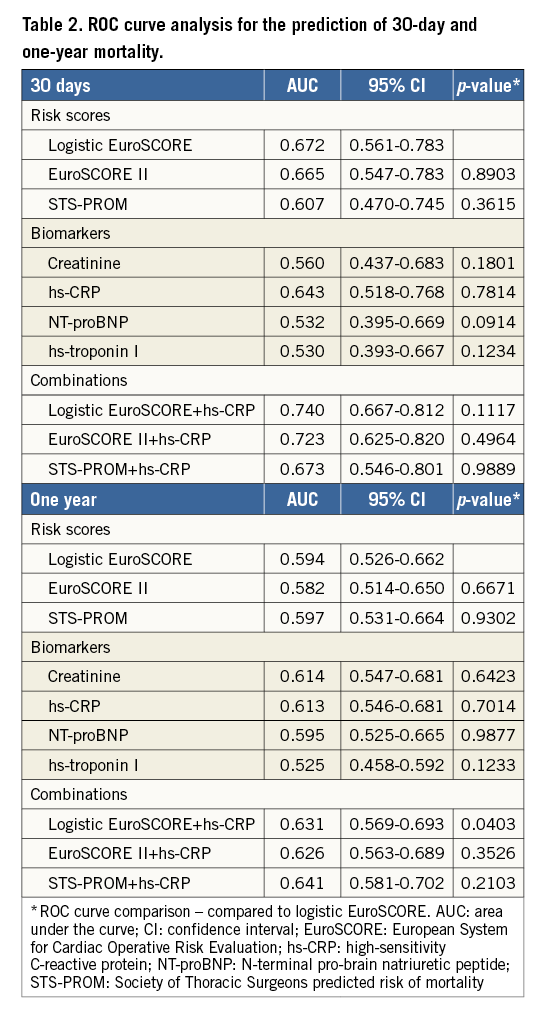
POTENTIAL FOR CLINICAL BENEFIT
To figure out whether a combination of clinical risk scores and biomarkers offers the potential for clinical benefit, logistic EuroSCORE and hs-CRP were combined to identify subgroups with different outcomes following TAVI. For this purpose, we categorised TAVI patients according to the median of their logistic EuroSCORE results and hs-CRP levels. Combinations of the medians of logistic EuroSCORE results and hs-CRP levels allowed the stratification of the TAVI patients into subgroups with one-year mortality rates ranging from 6.6% up to 18.2% (Figure 3, Figure 4).
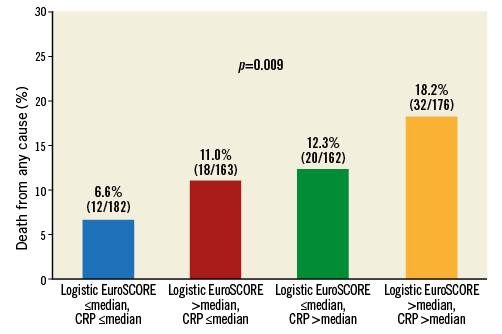
Figure 3. One-year mortality according to the medians of logistic EuroSCORE results and hs-CRP levels. The percentage of patients having an adverse event (N=82) is shown for each column. Combinations of increasing medians of logistic EuroSCORE results (≤14.24%, >14.24%) and hs-CRP (≤4.4 mg/L, >4.4 mg/L) levels allowed the stratification of TAVI patients into subgroups with one-year mortality rates ranging from 6.6% up to 18.2%.
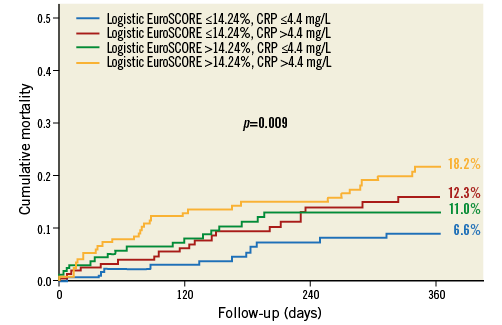
Figure 4. The association between one-year all-cause mortality and values of logistic EuroSCORE and hs-CRP according to the median. Combinations of medians of logistic EuroSCORE results (≤14.24%, >14.24%) and hs-CRP levels (≤4.4 mg/L, >4.4 mg/L) showed mortality rates ranging from 6.6% up to 18.2% (p=0.009).
Discussion
In the present study, we assessed the diagnostic value of circulating biomarkers to improve identification of TAVI patients at high risk of adverse clinical outcomes and assessed whether these biomarkers provide prognostic information beyond that of established predictive risk algorithms. Besides the logistic EuroSCORE, baseline hs-CRP was the only biomarker that was an independent predictor of one-year all-cause mortality in a current transfemoral TAVI-patient cohort treated with the most recent THV version. A combination of baseline hs-CRP and logistic EuroSCORE could further enhance risk stratification, and therefore could stimulate the development of a risk assessment strategy tailored for better identification of individual patients who might benefit from therapeutic aortic valve interventions independent of traditional risk indicators and conventional risk prediction scores, and of futile patients who should be treated conservatively. In contrast to previous preliminary studies, we demonstrated that both NT-proBNP and hs-troponin I were not able to predict 30-day and one-year mortality. As NT-proBNP and hs-troponin I are well-known biomarkers for cardiovascular diseases, especially in seriously ill patients, they have repeatedly been shown to facilitate stratification of cardiac risk10. However, in our analysis, neither biomarker had any prognostic value beyond that of established surgical risk scores. This might be, at least in part, explained by the fact that the patient cohort included only patients from 2014 onwards, who were at a median age of 81 years with a median STS-PROM score of only 3.8% and who have been treated according to clinical best practices (CT-based patient evaluation, etc.) with predominantly “next-generation” THVs. In other words, the failure of NT-proBNP and hs-troponin I may be a matter both of less sick patients and of considerable progress in research and techniques.
Risk stratification and outcome prediction in TAVI patients still represents a challenge in daily clinical routine. Several clinical variables and comorbidities, such as the presence of COPD, chronic renal failure, extracardiac arteriopathy, frailty syndrome, impaired left ventricular ejection fraction and pulmonary hypertension have been highlighted as markers of a poor prognosis following TAVI11. Nevertheless, even today, patient selection is still based on more or less standardised instruments of frailty and predictive surgical risk scores that were not explicitly designed for this purpose and that do not capture all of the prognostically relevant indices. However, in spite of the associated disadvantages and known limitations, each of these risk assessment algorithms, either alone or in combination, is regularly used in daily clinical routine and offers some help in the decision-making process. In line with a series of preliminary studies12-14, we were also able to demonstrate that all surgical scoring systems are predictive for one-year all-cause mortality following TAVI. As previously reported15, this finding encourages the assumption that all risk scores, although they have deficits in non-surgical patient populations such as TAVI candidates, consider important baseline clinical variables and comorbidities that are not only related to perioperative risk and in-hospital mortality in open heart surgery patients but also to one-year outcome in TAVI patients. Even though the logistic EuroSCORE itself only represents a “procedural” mortality risk score, it has repeatedly been demonstrated that the risk score is also associated with post-procedural outcome. An explanation as to why the outdated logistic EuroSCORE outperformed the more currently used EuroSCORE II and STS-PROM score in the present study might be that in this specific case it showed very good discriminatory ability (differentiation between survivors and non-survivors) but demonstrated poor calibration (the agreement between the predicted outcomes from the score and the observed outcomes, ultimately resulting in overestimated and/or underestimated risk). The GAV score, however, has been found not to be predictive at all. Given the fact that it was developed in 2008, it may not be applicable to the TAVI candidate from now on since the field is evolving so rapidly. In addition, TAVI patients constituted only a small part of the study population on which the score was initially developed, which might further limit its application to TAVI5. Taken together, there is a need for the development of risk and outcome prediction strategies for better selection of TAVI patients and to identify futile patients.
In this context, the utility of biomarkers, which reflect distinct aspects of cardiovascular or non-cardiovascular pathophysiology, may provide insights into disease dimensions that are not fully captured by clinical risk algorithms. Biomarkers have shown early promise in answering questions of risk stratification in combination with the logistic EuroSCORE in open heart surgery patients16. In the present study, we were able to identify a total of four biomarkers that showed an association with outcome following TAVI and were helpful in sorting out which patients are likely to be exposed to a heightened mortality risk at one year. As expected (and previously shown15), the prognostic power, however, differed substantially. Among all of these biomarkers, baseline hs-CRP showed the strongest association with 30-day and one-year mortality. In line with the preliminary data16, we found that a combination of the logistic EuroSCORE and hs-CRP allowed the discrimination of patients with and without adverse outcome and might facilitate rescheduling patients (who have initially been intended to receive TAVI) to individual and optimal treatment, whether that be conservative (medical therapy only) or interventional (TAVI). The combination of the medians of logistic EuroSCORE results and hs-CRP levels allowed the stratification of TAVI patients into subgroups with strongly differing one-year mortality rates ranging from 6.6% up to 18.2%. Hence, using these two readily available predictive risk parameters enables us to identify patients scheduled for TAVI with either favourable or adverse outcome prior to the planned procedure and to reconsider the decision already made.
hs-CRP is counted as an acute-phase protein whose levels rise in response to local or systemic inflammation17. It is devoid of all specificity, and its levels differ significantly in a variety of diseases such as acute infections of any kind or malignancy. There seems to be an obvious link between elevated levels of hs-CRP and cardiovascular risk factors such as hypertension, overweight, diabetes, and smoking. Moreover, increased hs-CRP levels seem to be associated with advanced age, extensive atherosclerosis, and reduced cardiac function18. Previous studies have provided some evidence that the underlying pathomechanism of atherosclerotic disease and AS may be partly similar, involving inflammatory response and sharing the aforementioned risk factors19. It thus appears logical that hs-CRP may play a pivotal role in cardiovascular diseases. With regard to atherosclerotic coronary artery disease (CAD), previous research found that hs-CRP apparently offers predictive value for adverse cardiac events in this patient group20. In the context of AS, several studies were able to show an association between AS severity and/or progression and hs-CRP levels21,22. Specifically, with regard to the typical TAVI patient, it should also be kept in mind that chronic low-grade inflammation in the elderly is considered to be a risk factor for the development of a multidimensional geriatric frailty syndrome consisting of increased vulnerability to stressors and reduced physiologic reserve that might define the older patient’s potential for recovery following TAVI. In the FRAILTY-AVR study, the authors compared the incremental predictive value of frailty scales and were able to show that the components of the essential frailty toolset (EFT) encompassing lower-extremity weakness, cognitive impairment, anaemia and hypoalbuminaemia have been correlated with higher circulating inflammatory markers, reflecting the biological link between increased inflammatory activity and frailty. Ultimately, both factors have been shown to have a negative impact on outcome following TAVI23.
Study limitations
Several study limitations should be noted. First, the single-centre character is a limitation of the study. For further verification and generalisation of our results, larger studies are needed. Second, there is potential selection bias due to the fact that all patients of our patient cohort were pre-selected for TAVI without conservative or surgical controls. Third, unknown treatment confounding due to missing drug history has to be assumed.
Conclusions
For the prediction of procedural outcome in recent TAVI patients, biomarkers such as NT-proBNP and hs-troponin were not superior to risk scores such as the logistic EuroSCORE. We found that baseline hs-CRP alongside the logistic EuroSCORE was an independent predictor of one-year all-cause mortality in transvascular TAVI patients. A combination of both might help to predict procedural risk and outcome after TAVI better and to identify futile patients.
| Impact on daily practice hs-CRP may be used in conjunction with the established clinical risk scores to help to predict procedural risk and survival of TAVI patients more adequately. It may also serve to identify patients most likely to benefit from TAVI. |
Conflict of interest statement
J-M. Sinning, E. Grube, G. Nickenig and N. Werner receive research grants and speaker honoraria from Medtronic and Edwards Lifesciences. E. Grube works as a proctor for Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix 1. Calculation of mortality according to clinical scoring systems.
Supplementary Appendix 2. Analysis of biomarkers.
Supplementary Table 1. Baseline characteristics.
Supplementary Table 2. Baseline characteristics according to the median of CRP levels.
Supplementary Table 3. Periprocedural characteristics.
Supplementary Table 4. Clinical outcomes according to one-year all-cause mortality.
Supplementary Table 5. Univariate and multivariate regression analysis (prediction of one-year mortality) – hazard ratios with 95% CI per 1 SD increase of risk scores and biomarkers.
To read the full content of this article, please download the PDF.