Abstract
Aims: The SYNTAX study compared PCI with TAXUS Express stents to CABG for the treatment of de novo 3-vessel and/or left main coronary disease. This study aimed to determine patient characteristics and five-year outcomes after a staged PCI strategy compared to single-session PCI.
Methods and results: In the SYNTAX trial, staged procedures were discouraged but were allowed within 72 hours or, if renal insufficiency or contrast-induced nephropathy occurred, within 14 days (mean 9.8±18.1 days post initial procedure). A total of 125 (14%) patients underwent staged PCI. These patients had greater disease severity and/or required a more complex procedure. MACCE was significantly increased in staged patients (48.1% vs. 35.5%, p=0.004), as was the composite of death/stroke/MI (32.2% vs. 19%, p=0.0007). Individually, cardiac death and stroke occurred more frequently in the staged PCI group (p=0.03). Repeat revascularisation was significantly higher in staged patients (32.8% vs 24.8%, p=0.035), as was stent thrombosis (10.9% vs. 4.7%, p=0.005).
Conclusions: There is a higher incidence of MACCE in patients undergoing staged compared to single-session PCI for 3-vessel and/or left main disease over the first five years of follow-up. However, these patients had more comorbidities and more diffuse disease.
Introduction
Multivessel coronary artery disease is a frequent finding at angiography1. In patients with stable angina, the prevalence of multivessel disease has remained between 40 and 50% over the past three decades2. Percutaneous coronary intervention (PCI) is often used to treat patients with complex multivessel disease and in patients with significant comorbidity. In patients who are felt to be suitable for multivessel PCI, a decision on the best procedural strategy is required, and operators must choose between treating all lesions at one sitting or bringing the patient back to the cardiac catheterisation laboratory for a staged procedure. In the setting of primary PCI for ST-elevation myocardial infarction, professional societal guidelines support treating the culprit vessel initially and staging PCI for the remaining disease3-6. There is less evidence on the best way to manage stable patients with multivessel disease. One study has shown that either a one-step or a staged treatment strategy (four to eight weeks later) can be employed with high procedural success rates and a low incidence of complication7. The Society for Cardiac Angiography and Interventions recommend that the treatment strategy be flexible in these patients depending on contrast and radiation doses as well as patient and operator conditions8. The SYNTAX study was a prospective, multicentre, multinational randomised trial of 1,800 patients with de novo 3-vessel or left main stem disease, who were randomised to either CABG or stenting with paclitaxel-eluting TAXUS® stents (Boston Scientific, Marlborough, MA, USA)9. The five-year results of this trial have now been published10. Three-vessel and/or left main disease was required for trial inclusion and the mean number of lesions treated per patient was 3.6±1.6. Staged PCI was discouraged by the protocol. One hundred and twenty-five (14%) patients in the randomised cohort of the SYNTAX trial underwent staged PCI. The objective of this study was to assess the differences in five-year outcomes between 3-vessel and/or left main stem disease patients who received staged versus single-session PCI with the TAXUS Express paclitaxel-eluting stent in the SYNTAX study.
Methods
The SYNTAX study was an “all-comers” prospective trial of patients with de novo 3-vessel coronary disease and/or left main stem disease. If considered eligible by a Heart Team meeting of local interventional cardiologists and cardiac surgeons, consenting patients were randomised to receive either CABG or PCI with the TAXUS Express paclitaxel-eluting stents. The study was conducted in 62 European centres and 23 centres in the United States of America. Full details of the methods have already been published in the original paper and supplementary appendix9.
PATIENTS
Of 4,337 patients screened to participate in the study, 1,800 were randomised. Patients considered to have only one treatment option were included in either a PCI or a CABG registry. SYNTAX scores were calculated at a core laboratory (Cardialysis, Rotterdam, The Netherlands) blinded to the patient’s treatment arm. Analysis of biochemistry was also performed at an independent blinded core laboratory (Covance, Indianapolis, IN, USA, and Geneva, Switzerland). Patients had to give written informed consent for the study. PCI or CABG was undertaken to achieve equivalent revascularisation of all vessels over 1.5 mm in diameter with at least a 50% stenosis. The number of lesions treated/pt was 3.6±1.6 mean±SD, the number of stents implanted 4.6±2.3 mean±SD, total length implanted 86.1±47.9 mm mean±SD (range 8-324 mm), and 33.2% of patients had stenting of >100 mm. The surgical or PCI technique adopted was at the discretion of the operator. A staged PCI procedure was allowed in the study provided it was performed within 72 hours of the index procedure and during the same hospital stay. In patients with renal insufficiency or contrast-induced nephropathy post procedure, staging could be performed; however, the second procedure had to be completed within 14 days. Dual antiplatelet therapy was administered following stent implantation as recommended by the directions for use of the TAXUS Express stent.
ENDPOINTS
We recorded and compared the incidence of major adverse cardiovascular and cerebrovascular events (MACCE: death from any cause, CVA, MI or repeat revascularisation) at five years in the single-session PCI group and those who had staged PCI procedures. The clinical reason for patients undergoing staged PCI was also recorded.
STATISTICS
Continuous variables were measured as mean±standard deviation and were compared using the Student’s t-test. Binary variables are expressed as percentages and were compared using the chi-square test.
Results
Of the 903 patients randomised to PCI, 125 (13.8%) received a staged procedure. The baseline characteristics of both groups are shown in Table 1. The incidence of hypertension, chronic obstructive pulmonary disease (COPD) and renal failure (creatinine >200 μmol/L) was significantly higher in the staged PCI group of patients. In addition, the Parsonnet and SYNTAX scores were significantly higher in the staged PCI group, indicating more comorbidity and coronary disease of greater severity.
Differences in procedural characteristics are highlighted in Table 2. The staged PCI group had a significantly higher incidenceof most of the anatomical features which increase the difficulty of percutaneous coronary inventions including: greater number of lesions; lesions of length >20 mm, coronary calcification, triple-vessel disease only, left main stem disease, chronic total occlusion and bifurcation lesions. The mean combined procedure time was almost double in the staged PCI group compared to the single-session group. Following the procedure(s), the staged PCI group of patients had a significantly longer length of in-patient hospital stay. The single-session PCI group received fewer stents (4.4±2.2 vs. 6.1±2.4, p<0.0001) and had less total implanted stent length
(82.0±46.1 vs. 110.7±51.0 mm, p<0.0001). The proportion of patients requiring over 100 mm of stents implanted was significantly less (29.8% vs. 53.6%, p<0.0001). There was no difference in maximum implanted stent diameter between the two groups (3.5±0.5 vs. 3.46±0.48 mm, p=0.35). Despite the greater number and length of stents used in the staged PCI group, those patients who had single-session PCI had the highest incidence of complete revascularisation.
In 47 (38%) cases, there was more than one reason for adopting a staged procedure strategy. In 40 (32%) cases, a staged strategy was planned in advance of the first procedure due to the medical status of the patient. A staged strategy was adopted in 54 (43%) cases due to the volume of contrast used, and in 14 (11%) cases due to known renal insufficiency. A long fluoroscopic time led to a staged procedure in 29 (23%) cases, and operator fatigue during long complex procedures contributed in 13 (10%) cases. A variety of other reasons led to a staged procedure in 22 (18%) cases. These data are highlighted in Figure 1. Differences in baseline characteristics between those patients who underwent a planned staged versus an unplanned staged procedure are shown in Table 3. No p-values are shown due to the small sample size in the planned staged group. We have presented the percentage difference with 95% confidence intervals. Planned staged as opposed to unplanned staged procedures occurred more frequently in males, patients with peripheral vascular disease and in those with Parsonnet scores ≥15. There were very few differences in procedural characteristics between those with planned and those with unplanned staged procedures; however, there was a higher percentage of patients with total occlusions (9.0% [–9.0, 27.1]) and bifurcations (9.7% [–3.0, 22.5]).
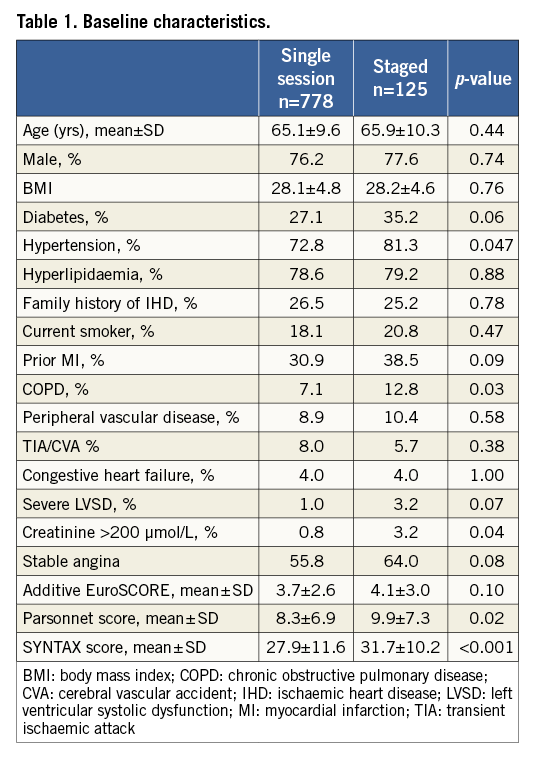
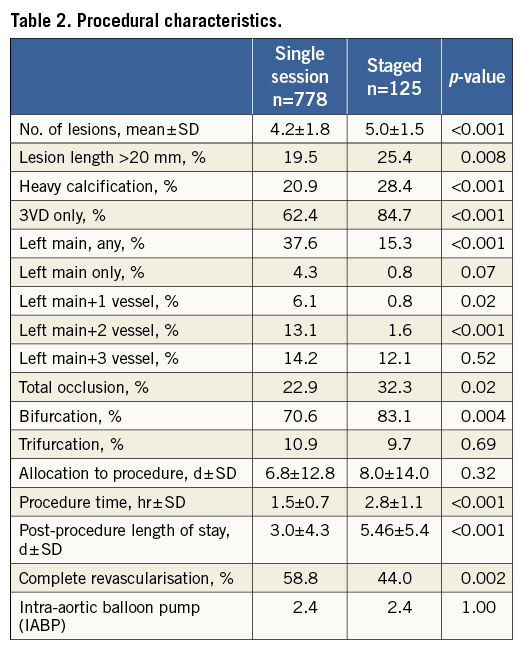
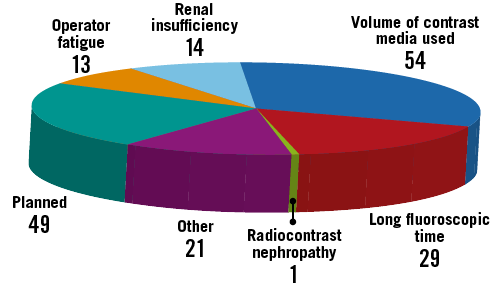
Figure 1. Reasons for adopting a staged PCI procedure strategy.
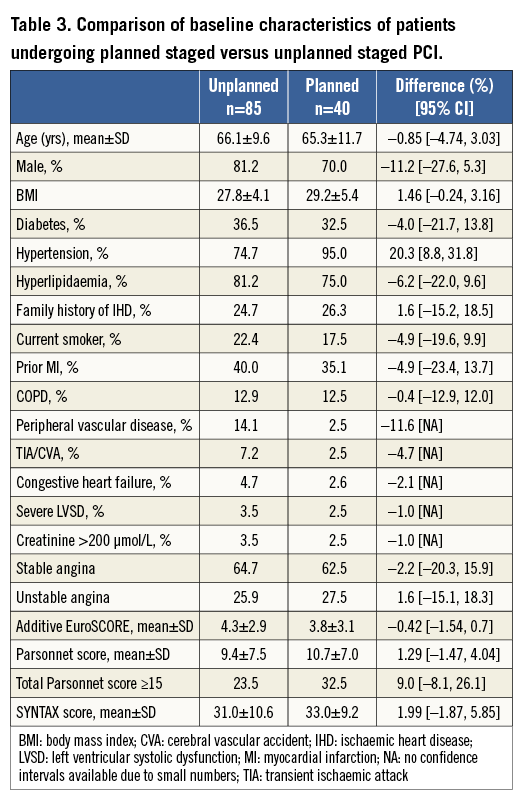
Figure 2 shows the five-year incidence of MACCE and the separate components of all-cause mortality, MI, CVA and repeat revascularisation. MACCE was significantly greater in the staged PCI group, as was a composite of death, stroke and MI (32.2% vs. 19.0%, p=0.0007). All-cause death was significantly higher in the staged PCI group: this was largely driven by increased cardiac death (14.3% vs. 8.1%, p=0.03). There was no significant difference between the two groups in terms of vascular death (1.9% vs. 0.6%, p=0.16) and non-cardiovascular death (7.1% vs. 4.3%, p=0.19). The increase in MACCE was also partially driven by a greater need for repeat revascularisation in the staged PCI group: 149 (20.4%) patients in the single-session PCI group required repeat PCI compared to 34 (28.4%) in the staged group (p=0.02). CABG was required following PCI in 45 (6.3%) single-session PCI patients compared to nine (8.0%) of the staged PCI group (p=0.48). As shown in Figure 2, stroke also occurred with a significantly higher frequency in the staged PCI group. The incidence of post-procedural stent thrombosis was also significantly greater in the staged PCI group with 13 (10.9%) patients experiencing this complication compared to 34 (4.7%) patients in the single-session PCI group (p=0.0045).
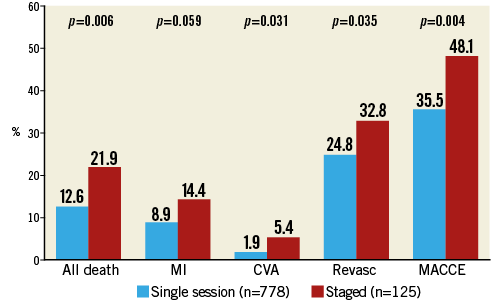
Figure 2. Five-year MACCE in patients with single-session and staged procedures.
A comparison of the five-year incidence of MACCE and its components between the planned and unplanned staged groups is shown in Figure 3. There was no statistically significant difference in all-cause mortality, MI, CVA, repeat revascularisation or MACCE between these two groups.
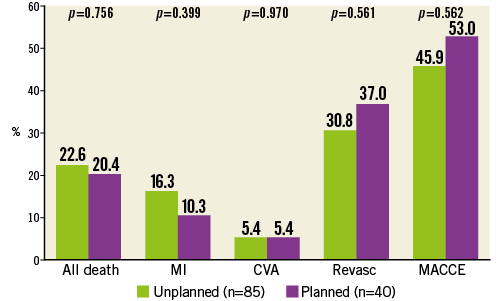
Figure 3. Five-year MACCE in patients who had planned and unplanned staged procedures.
Discussion
This substudy of the SYNTAX trial aimed to examine the reasons why staged PCI procedures were undertaken in a group of patients with complex coronary disease, and to look at the procedural differences and outcomes compared to those completing their index PCI in a single session. As one might expect, we have shown that patients undergoing staged PCI had more comorbidity: in particular, renal dysfunction with a creatinine >200 µmol/L, COPD and hypertension were more prevalent in this group. There was also a trend towards more diabetes mellitus, previous MI and poor LV function in the staged PCI group of patients. Renal disease was found to be a frequent reason for adopting a staged PCI approach. The risk of contrast-induced nephropathy in patients with renal disease is between 20 and 30%, and it is therefore important in these patients to minimise exposure and entirely appropriate to stage complex procedures11. In addition, patients with renal disease have a higher likelihood of having other cardiovascular risk factors such as hypertension and diabetes mellitus. Coronary disease in patients with diabetes mellitus is often more diffuse and likely to involve longer and more extensive revascularisation procedures12. There was a trend to more diabetes in the staged PCI cohort in this study with over a third of staged PCIs being performed in diabetic patients. This also contributed to the significantly higher SYNTAX score in the staged PCI group. COPD was significantly more prevalent in patients undergoing staged PCI. Coronary artery disease and COPD share a common risk factor in cigarette smoking, and this increased prevalence amongst the staged PCI group may result in an inability to tolerate a prolonged period of lying flat for a complex procedure13.
The SYNTAX score was higher in those patients undergoing staged PCI. Various components of the SYNTAX score are highlighted in Table 2, indicating that there were not only more lesions in the staged PCI group but that these were also longer, more calcified and more likely to involve the left main stem or a bifurcation. Chronic total occlusion was also significantly more common. All of these factors contribute to longer procedure times and the occurrence of operator fatigue. Operators may also have been mindful of their and the patient’s radiation exposure during long and difficult cases. Given the increasingly complex nature of the coronary disease in those patients undergoing staged PCI, it is not surprising that complete revascularisation was achieved in significantly fewer patients in this group, and this may have contributed to the significantly higher incidence of major cardiac events in patients undergoing staged PCI over the first five years of follow-up. Despite the use of drug-eluting stents, complex lesions have a higher risk of developing restenosis, and this will also have contributed to a higher incidence of repeat revascularisation in the staged PCI group14. Other factors associated with increased restenosis relevant to the staged PCI group include: total stent length, lesion length and diabetes mellitus15,16. A further contributory factor to repeat revascularisation in the staged PCI group is the higher incidence of stent thrombosis. Predictors of stent thrombosis have been extensively published with premature discontinuation of dual antiplatelet therapy being the most significant17. The staged PCI group in SYNTAX had more renal failure, bifurcation lesions and diabetes mellitus, all of which may have contributed to the higher rate of stent thrombosis18. In addition, staged patients had a greater number of lesions treated with a significantly greater length of stented segment and despite this were ultimately less completely revascularised when compared to the single-session group. With more lesions and more stents there will be an increased risk of unapposed stent struts, increasing the risk of this complication. There was also a trend towards more severe left ventricular systolic dysfunction (LVSD) in the staged PCI group. All of these factors will have contributed additionally to the greater incidence of stent thrombosis. All-cause death, and in particular cardiac death, was significantly higher in the staged PCI group of patients. This is likely to be a reflection of the more extensive coronary disease, increased comorbidities and more extensive vascular disease in this group of patients. The risk of stroke was also increased in the staged cohort of patients, and again we suspect this is a reflection of the greater comorbidity in this group, in particular hypertension and a trend towards a greater incidence of diabetes. It is therefore likely that this group had more undiagnosed cerebrovascular disease and thus over this extended follow-up period had more events.
Our substudy of the SYNTAX trial has provided a good insight into the reasons for staging, and for whom this should be considered. Our staged patients had more comorbidity and complex coronary disease. Patients with multiple comorbidity often find lying flat for a prolonged period difficult and should therefore be considered for staging upfront. Complex coronary anatomy, such as bifurcation lesions and heavy calcification requiring longer and more complex interventional techniques, should also be considered for staging in multivessel disease where operator fatigue can occur. The volume of contrast medium used and fluoroscopic time should be monitored during the procedure with staging of a lesion for a later date where it is in the patient’s best interests. Patients with pre-existing renal disease should also be considered upfront for staging, especially where significant volumes of contrast are likely to be utilised. Our study has shown that, where staging has occurred (either planned or unplanned during multivessel PCI), there is a higher incidence of MACCE over five years of follow-up. Therefore, operators should carefully weigh up the risks of multivessel PCI versus CABG in this group.
The SYNTAX study used the paclitaxel-eluting TAXUS Express stent. More modern stent types have been compared with this stent and been shown to have similar clinical efficacy and safety19. The SPIRIT IV study showed less target lesion failure, less target lesion revascularisation, less myocardial infarction and stent thrombosis using an everolimus-eluting stent compared to a paclitaxel-eluting stent20. Using more modern stent technology may result in fewer MACCE, though this benefit would have been seen in both the staged and single-session groups, and it is therefore difficult to predict if the results of the study would have been different. This may be plausible given that the majority of MACCE were due to repeat revascularisation.
Limitations
The main limitation of this study is that patients in the staged PCI and single-session PCI groups had a number of different baseline characteristics which have been highlighted in Table 1. The staged PCI group had a statistically significant higher incidence of hypertension, COPD, creatinine >200 μmol/L, Parsonnet and SYNTAX scores. Staged PCI was discouraged in the study and as such there were no set criteria provided for staging. The decision to stage a procedure was operator-dependent and we therefore cannot exclude an unmeasured selection bias. Patients in the SYNTAX trial had the most complex coronary disease included in a clinical trial and therefore these results cannot be extrapolated to patients with less complex multivessel disease.
Conclusions
Patients in the SYNTAX trial who were treated by staged PCI procedures had more comorbidities and more complex disease compared to the patients in whom PCI was conducted in a single session. The majority of reasons for staging a procedure were related to volume of contrast medium, length of fluoroscopy and renal insufficiency. It should be noted that the SYNTAX trial patients include the most complex coronary disease ever treated in a clinical trial, and this is amplified in the staged PCI group, with a mean stented length of over 110 mm. The outcome of a staged strategy in the part of the SYNTAX population with less complex lesions might be different. In the SYNTAX trial, despite increased procedure times and implanted stent lengths in patients with staged procedures there was more incomplete revascularisation. There is a significantly higher incidence of major cardiac events in patients undergoing staged PCI over the first five years of follow-up. The five-year outcomes in SYNTAX patients with 3-vessel coronary disease have been shown to have a lower MACCE rate for CABG compared to PCI in the most complex patients, consistent with the findings in this staged subgroup. The impact of staging in multivessel coronary disease patients with fewer comorbidities or less complex coronary anatomy requires further study as do the potential benefits of more modern stent technology.
| Impact on daily practice This substudy of the SYNTAX trial has shown us that patients with severe coronary disease requiring more complex intervention are more likely to undergo a staged PCI strategy due to the contrast volume used, longer fluoroscopy time and renal dysfunction. In daily practice, cardiologists should be mindful that patients undergoing staged PCI have a higher incidence of MACCE, a composite of death, stroke and MI, repeat revascularisation and stent thrombosis. This is important when considering revascularisation strategy and consent. |
Guest editor
This paper was guest edited by Ran Kornowski, MD, FESC, FACC; Department of Cardiology, Rabin Medical Center, Petach Tikva, Israel.
Acknowledgements
We would like to thank Kristine Roy of Boston Scientific for her support in the preparation of this manuscript.
Funding
This study was supported by Boston Scientific.
Conflict of interest statement
T. Feldman has received consulting fees, lecture fees and grant support from Boston Scientific and Abbott. K. Leadley is a previous employee of Boston Scientific and remains a shareholder. K.D. Dawkins is a full-time employee and owns equity in Boston Scientific. A. Colombo has received payment for SYNTAX Steering Committee membership made to his institution, coverage of cost for participation in scientific meetings and travel expenses related to the SYNTAX study. The other co-authors and the Guest Editor have no conflicts of interest to declare.

