Abstract
Aims: To assess the long-term outcome of patients who underwent radioactive stent (RS) implantation.
Methods and results: The RS study population consisted of 133 consecutive patients who underwent RS implantation between November 1997 and July 2000. They were matched using the propensity score method with 266 patients who underwent bare metal stenting (BMS) in the same span. Long-term survival status and information on MACE (death, non-fatal myocardial infarction or any re-intervention) was retrospectively obtained. Eight-year cumulative survival (90.2% vs. 87.4%, p=0.57) was similar between the RS and BMS group respectively, while 8-year cumulative MACE-free survival was significantly lower in RS patients (42.1% vs. 64.3%, p<0.001) due to the difference in events (mainly target lesion revascularisations [TLRs]) during the first year of follow-up (cumulative 1-year MACE-free survival: 59.4% vs. 86.7%, p<0.001); there was no difference in the MACE rate after the first year (p=0.71). The TLR rate at six months in the RS group was 29.3%, mainly due to edge restenosis and at one year 36.2% (control group: 9.5%, p<0.001).
Conclusions: A high incidence of MACE and re-intervention was observed during the first year following RS implantation, mainly related to TLR for edge restenosis. After the first year, the clinical outcome of RS patients was similar to the control group indicating that there are no late adverse effects related to low dose-rate intracoronary radiation therapy.
Introduction
Radioactive stents (RS) were evaluated as a treatment for restenosis prevention. Preclinical evaluation in two animal models showed discordant results, with reduction of neointimal formation in a dose-related manner in the rabbit iliac artery, but more complex dose relationship in the pig coronary artery1-3. Initial human studies with low activity (0.75-1.5 µCi) RS showed that their use was feasible and safe, but ineffective for the prevention of in-stent restenosis4. Dose finding studies with intermediate activity (3-12 µCi) RS, proved their efficacy in preventing intrastent restenosis, but simultaneously revealed their major limitation related to the development of stent edge restenosis, the so-called “edge effect” or “candy wrapper”5,6. Efforts to eliminate edge restenosis, either with high or low activity RS (12-21 µCi)7, stent edge activity modification (cold-end, hot-end RS)8-10 or the use of dedicated edge non-traumatic square shouldered balloons failed11.
The aim of the present study was to describe the long-term clinical outcome after RS implantation in comparison to a matched control group treated with bare metal stents (BMS). Although no longer in clinical use, these results might improve our understanding of the potentially long lasting interaction between localised radiation therapy and vascular response in humans.
Methods
Patient population
Between November 1997 and July 2000, 133 patients received one or two radioactive stents in our institution. The patients were part of five different studies. The design and short-term outcome of the studies have been previously reported. An overview of the studies is presented in Table 1.
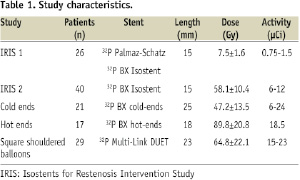
Briefly the IRIS 1 study was a safety and feasibility study and IRIS 2 was a European dose finding study4,5. The cold end8,9, the hot end10 and the square shouldered balloons11 were studies with dedicated RS and balloons to overcome the problem of edge stent restenosis observed with this therapeutic modality.
In the same span, 2,912 patients underwent BMS implantation for stable or unstable angina in our institution. The propensity score methodology, as previously described and reported12, was used to identify a subgroup of BMS patients with comparable baseline characteristics to those of the RS patients. The matched control group was selected to be double in size (i.e., 266 patients) compared to the RS group. Antiplatelet therapy after stent implantation in RS patients was based on the protocol of each separate study (aspirin 80 mg daily indefinitely and ticlopidine 250 mg BID or clopidogrel 75 mg daily for one to six months according to the study), while all BMS patients received aspirin 80 mg daily and ticlopidine 250 mg BID or clopidogrel 75 mg daily for one month.
Follow-up
The Thoraxcenter is a tertiary cardiology centre, serving a group of 14 local hospitals for percutaneous coronary interventions in the region of Rotterdam. As required by the local medical system organisation, all baseline procedures were performed in this tertiary facility, as well as the vast majority of re-interventions.
In all RS studies follow-up angiography was performed at six months and one year as mandated by the protocol; a follow-up angiography in RS patients with a target lesion revascularisation at six months was not performed again at one year. Routine angiographic follow-up was not available in any patient of the BMS group. Long-term survival status was assessed by written inquiries to the Municipal Civil Registries. Questionnaires were sent to all living patients focusing on the occurrence of major adverse cardiac events (MACE) such as, myocardial infarction, and repeat intervention (surgical and percutaneous). The referring physician and institutions as well as the general practitioners were directly approached whenever necessary.
Definitions
Major adverse cardiac events were defined as: 1) death, 2) non-fatal myocardial infarction (MI), 3) repeat revascularisation. Target lesion revascularisation (TLR) was defined as any surgical or percutaneous re-intervention due to restenosis within the RS or in the 5 mm proximal or distal peri-stent segments (edge restenosis). Target vessel revascularisation was defined as any re-intervention driven by lesions located in the treated vessel. By protocol, in all studies, RS implantation in more than one vessel was prohibited.
Total occlusion was defined as stent occlusion documented by coronary angiography. Subacute thrombosis was defined as angiographically documented total occlusion ≤ 30 days. Late total occlusion was defined as angiographically documented total occlusion > 30 days post-intervention. The definition of very late total occlusion was applied for patients who had a patent artery at six months follow-up and subsequently presented with total occlusion at the same site. Thrombotic occlusion was defined as any occlusion that resulted in an acute coronary syndrome (MI or unstable angina)13.
Statistical analysis
Categorical variables (presented as counts and percentages) were compared between groups using the chi-square test or Fisher’s exact test and continuous variables (presented as their mean ± standard deviation) were compared using the Student’s t-test. Survival and event-free survival rates were estimated by Kaplan-Meier curves and differences between groups were assessed with the use of the log-rank test of significance. Statistical significance of all tests was defined at the p<0.05 level. The SPSS statistical software package (version 13.0 for Windows, SPSS Inc. Chicago, IL, USA) was used for the analysis.
Results
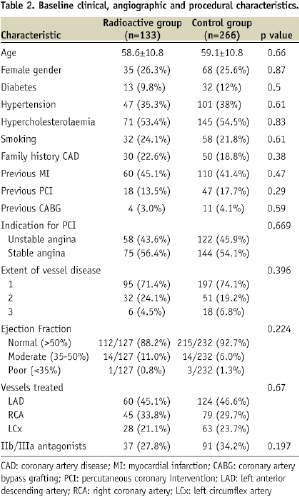
Complete clinical follow-up was achieved in all (100%) RS patients and in 255 (95.9%) patients in the control group. Mean follow-up duration was 6.37±1.44 years and 6.4±1.61 years in the RS and the control group respectively. Table 2 summarises the baseline clinical, angiographic and procedural characteristics of the two patient groups.
Clinical outcome
Cumulative 8-year survival (90.2±2.7% in the RS group vs. 87.4±2.7% in the control group, p=0.569) and MI-free survival (90.1±2.8% in the RS group vs. 92.4±1.7% in the control group, p=0.508) were similar between the two groups. Twelve RS patients suffered an MI. Four were referred for primary percutaneous coronary intervention. Angiographic total occlusion of the RS was documented in two (in one 1,276 days after the index procedure) and severe in-stent restenosis in the third. In the fourth patient the infarction was due to occlusion of a vessel other than that in which the RS was implanted. The remaining eight patients were initially treated with thrombolysis; elective angiography showed edge restenosis of the RS in six and in-stent restenosis in the other two. All patients were treated successfully.
Cumulative 8-year MACE-free survival was significantly lower in the RS group (42.1±2.7% [73 events] in the RS group vs. 64.3±3.6% [83 events] in the control group, p<0.001; Figure 1A) due to the difference in events (mainly TLRs) during the first year (cumulative 1-year MACE-free survival: 59.4% vs. 86.7%, p<0.001). However, cumulative post-1-year MACE-free survival was similar between the two groups (70.8±7.2% in the RS group vs. 74.3±3.7% in the control group, p=0.714; Figure 1B).
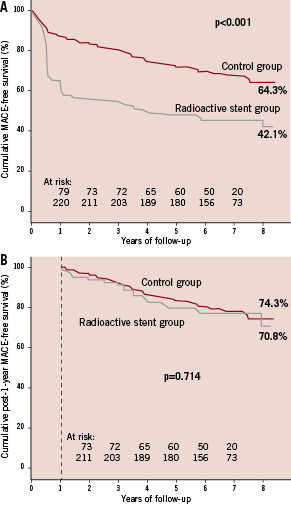
Figure 1. A. Cumulative 8-year MACE (major adverse cardiac events; death, MI, revascularisation) –free survival curves for the radioactive stent (RS) and control groups. In the RS group up to six months, a relapse is clearly visible followed by a sharp decrease related to the first angiographic control. From six months up to one year the curve remains stable. Around one year a second sharp decrease occurs in the RS group related to the second angiographic control. B. From one year and up to eight years there is no difference in MACE-free survival between the two groups.
Re-intervention
Cumulative 8-year revascularisation-free survival was significantly lower in the RS group (48.1±5.6% [64 events] vs. 76.8±3.2% [52 events], p<0.001). The majority of re-interventions were TLRs for both the RS (n=55; 86% of the events) and the control group (n=42; 81%). Cumulative TLR rate at six months in RS patients was 29.3% and directly related to the first angiographic follow-up (8.7% for the control group). A second wave occurred at one year related to the second angiographic follow up (cumulative TLR rate at one year in RS patients: 63.8% vs. 9.5% for the control group, p<0.001). The average time to the first TLR was 279±235 days in the RS group. Clinical and angiographic characteristics related to the first TLR are presented in Table 3.

Total occlusions
The incidence of total occlusions in RS patients (7.5%) was significantly higher (p=0.028) compared to the control group (2.4%; Table 4).
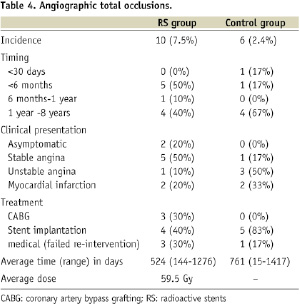
No subacute thrombosis was observed in the RS group. The incidence of late total occlusion in RS patients was 3.8% and that of very late total occlusion was also 3.8%. In three RS patients (2.2%) the occlusion resulted in an acute coronary syndrome (late thrombotic occlusion), but no death occurred. Two RS patients underwent TLR for edge restenosis, with BMS implantation, before the vessel was finally occluded.
Discussion
Edge effect
Radioactive stents were proposed as a therapy for restenosis prevention. During safety-feasibility and dose finding studies they proved to be efficient for preventing in-stent restenosis but edge restenosis, called the edge effect, became clearly apparent as their limitation14. Intravascular ultrasound studies demonstrated that this effect is a combination of negative remodelling and plaque progression at the stent edges6. The fall of the dose at the stent edges in combination with balloon injury which systematically occurs was considered to be the cause. This is a well established phenomenon in catheter based brachytherapy, called geographical miss, responsible for the development of edge restenosis15,16. Animal studies with half RS confirmed this hypothesis17.
Attempts to resolve the problem, by making the edges of the stents non-radioactive (cold-end RS) to prevent negative remodelling, or by increasing the activity at the edges (hot-end RS) to avoid under-dosage, failed8-10. A last attempt with the use of square shouldered balloons aiming to minimise injury outside the stent edges was also not successful11 and RS never found a place in routine clinical use18,19.
Effect of the angiographic control
The MACE-free rate in RS group (42%) eight years after the implantation was significantly lower in comparison to both the control group and literature data regarding the expected outcome after the implantation of a non-radioactive stent20. The angiographic control at six months and one year affected the re-intervention rate since 20% of the TLRs were performed in asymptomatic patients. This probably influenced the time distribution of the re-interventions and the relative composition of the MACE rather than the event-free survival rate. All these patients had severe angiographic restenosis, and it is highly likely that they would have developed symptoms if they remained untreated.
Comparison with non-radioactive stents and catheter based brachytherapy
Lumen deterioration after conventional stent implantation occurs mainly in the first three months with minimal change between six months and one year and actual regression of neointimal hyperplasia between one and three years after stenting21,22. A non-significant increase in the incidence of MACE and re-intervention was observed in our population between six months and one year. This might well be attributed to the second angiographic control, although there is evidence that RS, in contrast with the promising results observed at 28 days, promote the formation of “atheromatous” neointima in a porcine atherosclerotic coronary model at six months23. Our group reported a significant increment in the in-stent neointimal hyperplasia between six months and one year (13-26 half-lives of the P32 isotope) in RS with activity 6 to 12 µCi, by means of intravascular ultrasound24. These results may indicate that the TLRs between six and 12 months were a result of late neointimal formation (delayed healing response). After the first year, the clinical outcome following RS implantation is stable and comparable to non-radioactive stents indicative that there are no long-term adverse effects after low dose rate irradiation18,25.
The long-term outcome after brachytherapy for de novo lesions has not yet been reported. Angiographic analysis from the SCRIPPS trial (gamma radiation for in-stent restenosis) at three years showed a reduction of the minimum lumen diameter in irradiated patients, but not in the placebo group, with further increase in the TLR rate in the irradiated patients only between three to five years26,27. An increase in the revascularisation rate between six months and three years in the irradiated group only of the WRIST trial (gamma radiation for in-stent restenosis) was also observed28. The difference in the time frame of the restenosis process between radioactive stenting and catheter-based gamma-radiation therapy may be a function of the biological response to the type and dosage of radiation administered.
Limitations
This is a single-centre retrospective study and therefore the results are limited by the shortcomings inherent to this type of studies. However, the propensity score matching between the RS and the control group addresses the design limitations of this study. Furthermore, RS patients do not come from one single study, but from different studies with iteration of the RS technology and variability in terms of antiplatelet therapy duration. The lack of angiographic follow-up in the BMS control group is another limitation which might have influenced the time of TLR occurrence.
Conclusions
A high incidence of MACE and re-intervention was observed during the first year after RS implantation that led to this technique being abandoned. After that period, the long term clinical outcome is stable and comparable to non-radioactive stents, indicating that there are no late adverse cardiac effects related to low dose-rate intracoronary radiation therapy.