Abstract
Aims: Percutaneous left atrial appendage (LAA) occlusion is an alternative to oral anticoagulation for the prevention of stroke in patients with non-valvular atrial fibrillation (NVAF). Due to the great anatomic variability of the LAA, complete closure may not always be obtained with a single device. We report cases in which adequate closure of the LAA was achieved with implantation of two devices.
Methods and results: Five out of 223 consecutive patients who underwent LAA occlusion without guidance with transoesophageal echocardiography (TOE) had a second device implanted to treat significant residual leaks or uncovered parts of the LAA after first device implantation. All procedures were successful, with no complications. Two patients received two AMPLATZER Cardiac Plugs (ACP); one patient received one ACP and one AMPLATZER Vascular Plug; one patient received one AMPLATZER Septal Occluder (ASO) and one ACP prototype; and one patient received two ASOs. TOE performed at least four months after the procedure showed complete closure of the LAA in all patients, without thrombus formation on the devices. After 14 patient-years there were no strokes, peripheral thromboemboli, or device embolisations.
Conclusions: When necessary, the implantation of two devices to achieve complete LAA occlusion in patients with NVAF is feasible and leads to favourable results during follow-up. Potentially, this technical innovation may widen LAA occlusion indications by permitting occlusion of LAAs with large ostia or complex anatomy.
Introduction
Stroke prevention is a primary goal in atrial fibrillation (AF) treatment. Oral anticoagulation with vitamin K antagonists (VKA) is the standard of care for these patients1. However, the intricate use and the potentially life-threatening bleeding complications associated with VKA lead to underutilisation of this therapy. In patients with non-valvular AF (NVAF), 90% of atrial thrombi originate from the left atrial appendage (LAA)2. Percutaneous LAA occlusion was introduced into clinical practice in 2001 as an alternative to oral anticoagulation in this setting3. Since then, good follow-up results have been demonstrated after LAA closure with the PLAATO device4, AMPLATZER occluders5, the WATCHMAN device6, the AMPLATZER Cardiac Plug7,8 and the Lariat device9. However, one single device may not always fit the great anatomic variability of the LAA. Significant residual leaks or uncovered parts of the LAA may persist as potential residual niches for thrombus formation. Adequate closure may require more than a single device. We report a consecutive series of patients in whom double device LAA occlusion (unplanned in four cases and planned in one case) was performed to achieve adequate closure of the LAA.
Methods and results
Data from 223 consecutive patients with permanent or paroxysmal NVAF, at least one additional risk factor for thromboembolic events, absence of thrombus in the LAA, and contraindication or aversion to chronic oral anticoagulation who underwent LAA occlusion for prevention of stroke were prospectively collected. Five of these 223 patients needed to have a second device implanted, either at the initial procedure (three patients) or during follow-up (two patients), to treat significant residual leaks or uncovered parts of the LAA after implantation of a first device.
Before intervention, pre-evaluation transoesophageal echocardiography (TOE) was performed to exclude thrombi in the LAA and antibiotic prophylaxis with cefuroxime was given. The procedures were performed via the femoral access under local anaesthesia, and were controlled by angiography only (biplane in most cases). At the beginning of the intervention 5,000 units of heparin were given. After transseptal passage, angiography and measurement or estimation of the LAA diameter at the intended implantation site were performed in at least two projections. The second device was chosen to fit best the residual leak to be covered. After the procedure, clopidogrel 75 mg daily was given for one month and acetylsalicylic acid 100 mg for three to five months, or lifelong in the case of significant coronary artery disease. Control transthoracic echocardiography was performed before discharge. The patients received two additional doses of cefuroxime, if discharged home the day after the intervention, and one if discharged the same day. Endocarditis prophylaxis was recommended for a few months and clinical control as well as a TOE was scheduled at three to six months after implantation.
Case 1
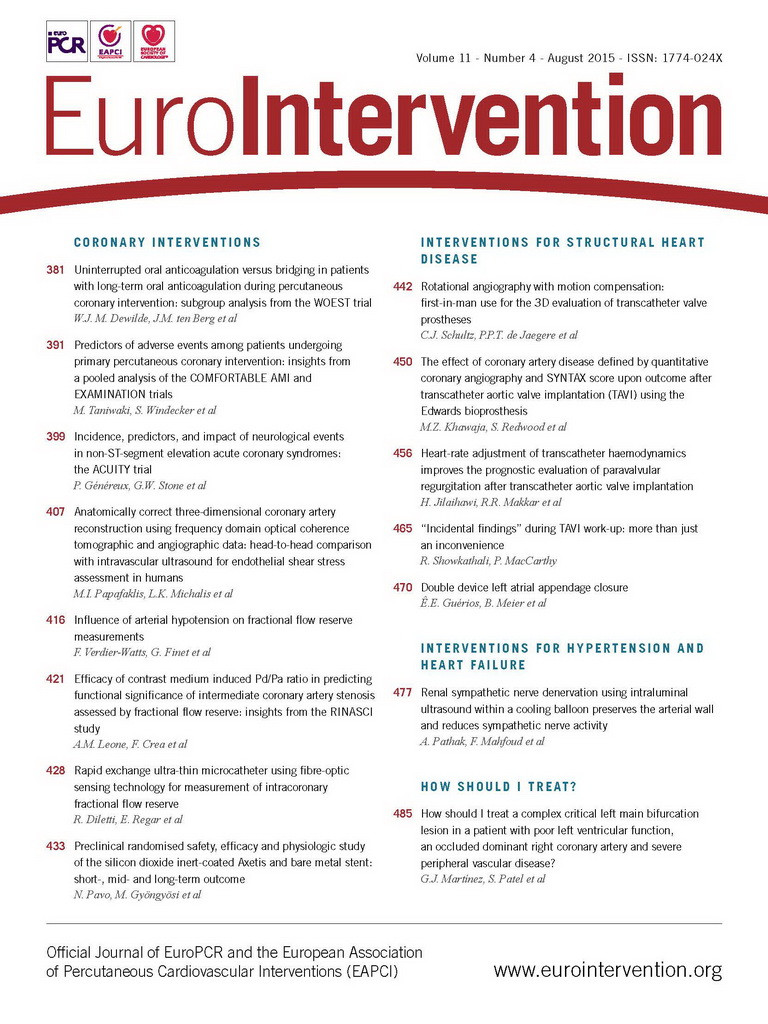
A 66-year-old woman was admitted in 2005 for LAA occlusion due to paroxysmal AF, a CHADS2 score of 3 and a history of intracranial bleeding while using VKA. A 19 mm AMPLATZER™ Septal Occluder (ASO) (St. Jude Medical, St. Paul, MN, USA) with discs of 31 and 29 mm was implanted in the LAA (with a landing zone of 20 mm) through a patent foramen ovale (PFO) without evident residual leak. At the end of the procedure the PFO was occluded with a 25 mm AMPLATZER™ PFO Occluder (St. Jude Medical). As per protocol, she was discharged on acetylsalicylic acid 100 mg daily for five months and clopidogrel 75 mg daily for one month. Six years later she was readmitted for a stroke. A TOE showed no thrombus in the left atrium, complete closure of the PFO, but incomplete closure of the LAA with a 2 mm gap permitting continued flow between the inferior part of the LAA and the left atrium (Figure 1). This could have been causing the recurrent stroke. As the patient had a high risk for oral anticoagulation, a second intervention to complete LAA closure was proposed. The interatrial septum was punctured below the PFO device. Left atrial angiography confirmed the partial LAA patency. The remaining channel in the LAA was entered using a regular 0.035” guidewire and a right Judkins 4 diagnostic catheter inside a long 9 Fr sheath. A 25 mm AMPLATZER PFO Occluder was successfully deployed sandwiching the discs of the previously implanted device and totally occluding the LAA. The patient was again placed on acetylsalicylic acid 100 mg daily and clopidogrel 75 mg daily for five months and one month, respectively. The follow-up was uneventful. A TOE performed after four months showed good position of both devices, with no evidence of residual shunt.
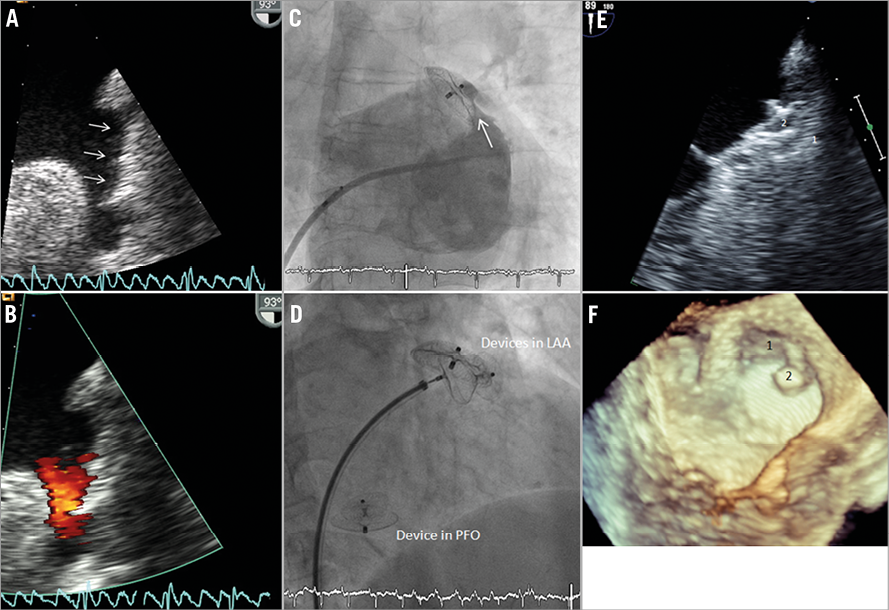
Figure 1. A) & B) Transoesophageal echocardiogram (TOE) showing a residual leak in the left atrial appendage (LAA) six years after previous implantation of a 19 mm AMPLATZER™ Septal Occluder (arrows). C) Left atrial angiography after transseptal puncture adjacent to the lower rim of the 25 mm AMPLATZER™ PFO Occluder confirming the partial patency of the LAA (arrow). D) Implantation of an additional 25 mm AMPLATZER PFO Occluder, sandwiching the discs of the previously implanted device. E) Two-dimensional, and F) three-dimensional TOE four months after the second implantation showing complete closure of the LAA and good position and freedom from thrombus of devices 1 and 2.
Case 2
A 77-year-old male patient underwent closure of a bilobulated LAA due to permanent AF, a CHADS2 score of 2, CHA2DS2-VASc score of 3, and recurrent gastrointestinal bleeding under VKA. The inferior lobe originated directly at the large ostium of the LAA precluding adequate landing of the lobe of the AMPLATZER™ Cardiac Plug (ACP) (St. Jude Medical) (Figure 2). In a single intervention, the upper lobe of the LAA (with a landing zone of 17 mm) was closed by implantation of a 22 mm ACP, and the lower lobe by implantation of a 16 mm AMPLATZER™ Vascular Plug I (St. Jude Medical). The patient was placed on clopidogrel 75 mg daily for one month after the intervention and acetylsalicylic acid 100 mg daily indefinitely. TOE control after four months showed complete closure of the LAA without thrombus on the devices. Nine months after the intervention the patient was readmitted due to chest pain. TOE showed a haemodynamically non-significant pericardial effusion. It confirmed complete occlusion and absence of residual flow in the LAA, making the diagnosis of late bleeding unlikely. The patient was managed conservatively. The effusion regressed within days and the further course was uneventful.
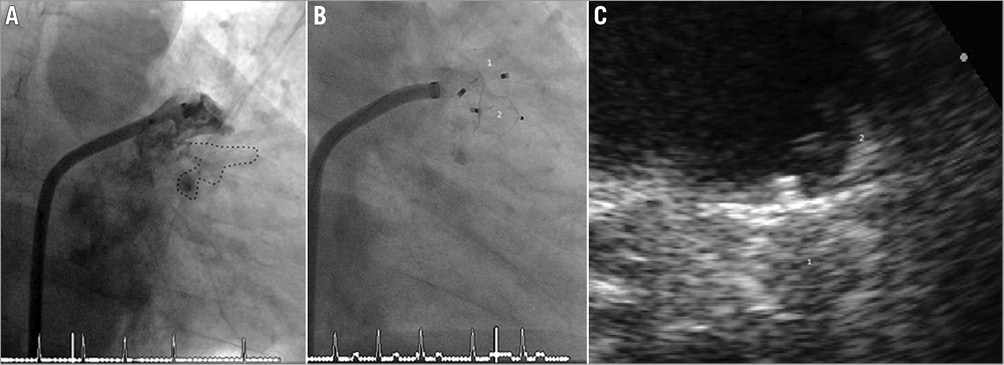
Figure 2. A) Bilobulated left atrial appendage (LAA) with a large ostium. B) Closure by implanting a 22 mm AMPLATZER Cardiac Plug (ACP) (1) in the upper lobe and a 16 mm AMPLATZER Vascular Plug I (2) in the lower lobe. C) Follow-up transoesophageal echocardiogram at four months showing complete closure by devices 1 and 2 without thrombi on the devices.
Case 3
A 65-year-old man with permanent AF, previous stroke, a CHADS2 score of 3, CHA2DS2-VASc score of 5, and hepatic disease precluding the use of VKA underwent LAA closure. After transseptal puncture a bilobulated LAA with a landing zone of 17 mm and a large ostium was demonstrated by angiography (Figure 3). Accordingly, a 20 mm ACP was implanted into the upper lobe of the LAA. After verifying good device position and stability, the prosthesis was released, but the 24 mm disc did not adequately cover the LAA ostium. It had moved deeply into the LAA neck, leaving the lower LAA lobe patent. For complete LAA occlusion a second ACP 26 mm (32 mm disc) was implanted into the proximal third of the LAA. It was well anchored by some of its hooks gripping the first device and completely occluded the LAA ostium. A control TOE after four months showed good position of both devices, with total occlusion of the LAA and no thrombus. One year after the intervention the patient remained free of symptoms on acetylsalicylic acid 100 mg daily indefinitely.
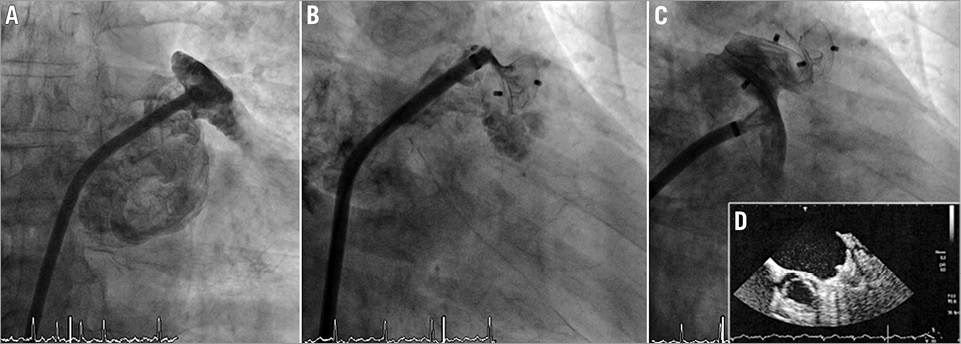
Figure 3. A) Pre-implant contrast medium injection, showing a bilobulated left atrial appendage (LAA). B) A 20 mm ACP selectively occludes the upper lobe of the LAA. The lower lobe remains uncovered. C) Complete occlusion of the LAA after implantation of a 26 mm ACP at its ostium. D) Follow-up transoesophageal echocardiogram at four months showing complete closure without thrombi on the devices.
Case 4
A 62-year-old male underwent percutaneous occlusion of a bilobulated LAA due to persistent AF and aversion to VKA. A 15 mm ASO was implanted in the LAA without complications (Figure 4). After device implantation, a residual leak was detected but considered acceptable. The patient remained asymptomatic, but a later control TOE showed persistent flow in the lower lobe of the LAA. In a second intervention after 13 months, this lobe (with an ostium of 15 mm) was closed by implantation of an 18 mm hookless ACP prototype (Figure 4). The patient used acetylsalicylic acid 100 mg daily and clopidogrel 75 mg daily for five months and the control TOE performed at six months showed complete occlusion and no thrombus.
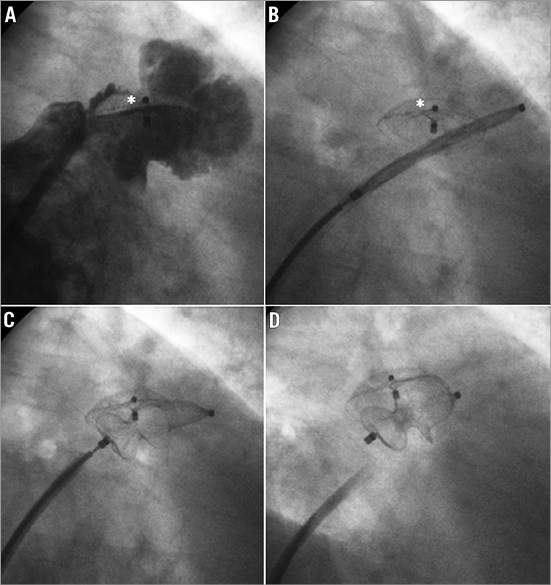
Figure 4. A) Persistent flow in the lower lobe of the left atrial appendage (LAA) 13 months after implantation of a 15 mm AMPLATZER Septal Occluder (asterisk). B) Positioning of a hookless ACP prototype in the lower lobe of the LAA past the initial occluder (asterisk). C) Deployment of the ACP prototype. D) Total occlusion of the uncovered part of the LAA.
Case 5
A hypertensive 69-year-old male with a history of coronary artery bypass grafting and persistent AF had a CHA2DS2-VASc score of 5 and a history of ischaemic stroke six years earlier in spite of VKA. After transseptal puncture, left atrial angiography demonstrated a large trilobulated LAA with a 46 mm ostium (Figure 5). Knowing that two devices would be necessary, the largest available ACP (30 mm) was placed at the entrance of the biggest superior lobe. It occluded two of the three lobes but left a smaller inferior lobe with an 11 mm ostium uncovered. The subsequent implantation of an additional 16 mm ACP achieved complete occlusion of this large LAA. The follow-up was uneventful.
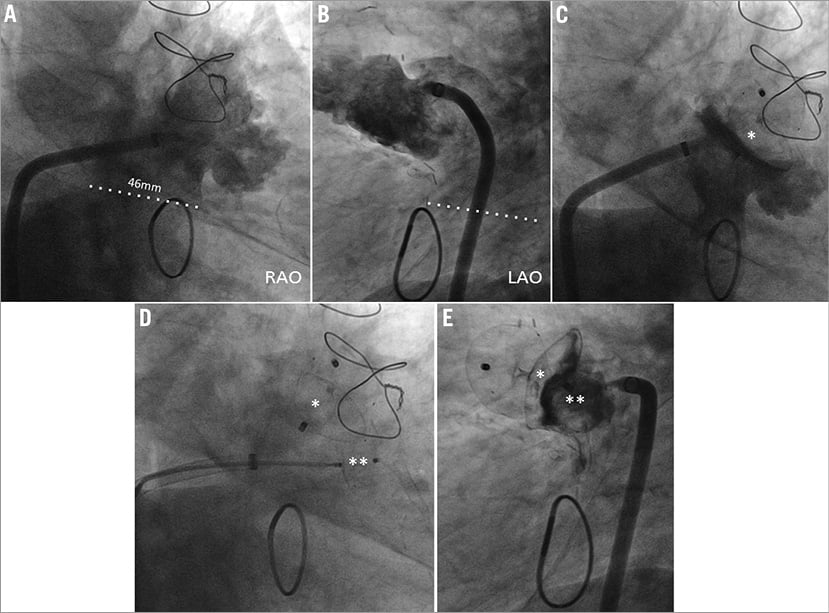
Figure 5. Angiography in right anterior oblique (RAO, A) and left anterior oblique (LAO, B) projections depicting a trilobulated left atrial appendage (LAA) with a large ostium (dotted line). C) A 30 mm ACP with a 36 mm disc (asterisk) occluding two of the three lobes but leaving the inferior lobe uncovered. D) Placement of a 16 mm ACP into the inferior lobe (double asterisk). E) Final complete occlusion of the LAA.
Discussion
The randomised PROTECT AF trial proved the concept of LAA closure for stroke prevention in AF by demonstrating non-inferiority to anticoagulation with VKA6. The benefits of the intervention were sustained at 1,500 patient-years of observation. LAA occlusion was, in fact, more effective than VKA in the long term when considering patients in whom final deployment of the closure device was successful10. The late net clinical benefit of LAA occlusion is enhanced among patients with a previous history of ischaemic stroke and in patients with CHADS2 scores ≥211.
Several devices have been used for percutaneous LAA closure. The first one was the PLAATO, used until 2006. The off-label use of AMPLATZER occluders was established in 20025. Afterwards, dedicated devices such as the WATCHMAN™ device (Boston Scientific, Natick, MA, USA), the Sideris patch12, the ACP, the Coherex WaveCrest® (Coherex Medical, Salt Lake City, UT, USA), and the LARIAT® device9 (SentreHEART, Inc., Redwood City, CA, USA), were introduced in clinical practice. However, there is a myriad of variations of LAA anatomy in terms of shape, axis, volume, number and plane of lobes, and size and shape of orifices13,14, and no single device fits them all.
One of the technical challenges of LAA occlusion relates to the elliptical rather than circular ostium. Deploying a round implant into an oval-shaped orifice may lead to incomplete sealing and residual peridevice leaks, reported in as many as 50% after PLAATO and 32% after WATCHMAN device implantation15,16. Incomplete sealing of the LAA has been linked to a higher risk of cardioembolic events in patients undergoing surgical LAA closure17,18. There has been debate as to whether it can be blamed for recurrent strokes after percutaneous LAA occlusion15,16,19,20 as in case 1. Theoretically, such leaks may maintain significant thrombogenicity of the remnant LAA, particularly if crevasses between pectinate muscles remain uncovered. A potential advantage of the ACP over the other LAA occlusion devices is the presence of a proximal disc (remnant of the initially used non-dedicated AMPLATZER devices5) destined to cover the ostium of the LAA (pacifier principle7,8) to neutralise anatomic variations of its body. However, larger or eccentric ostia may not be fully covered by the disc, as in two of the cases described. The recently launched second-generation ACP (Amulet™) provides larger discs to overcome this limitation21.
In addition to ostial eccentricity, another restriction inherent in single-device LAA occlusion technique concerns the maximum LAA body size suitable for intervention. Even the newest WATCHMAN and ACP devices only fit LAAs with a maximum body diameter of 30 mm21,22. However, there are some LAAs with exceptionally large bodies and ostia (our case 5). They preclude percutaneous occlusion with a single device. Using more than one device, as described earlier8,23, may render these interventions feasible.
The mean CHA2DS2-VASc score of 5 of the studied cohort projects a yearly occurrence of 6.7% of embolic events without VKA24. The patients were followed for a total of 14 patient-years and no embolic event or device embolisation was observed, suggesting clinical efficacy of the double device implantation technique.
Despite the more liberal oversizing technique usually performed at our institution, the lack of intraprocedural TOE guidance may arguably have led to the use of a first device too small for some cases. In our opinion, however, angiography provides all the information needed for LAA occlusion. Only five (2.2%) among 223 patients who underwent angiographically guided LAA occlusion at our institution required a second device. In addition, our results show a low complication rate and consistently high rates of complete closure at late follow-up after LAA occlusion8. Occluding the LAA in this more frugal way is effective and spares general anaesthesia and the requirement of TOE staff in the catheterisation laboratory. However, TOE guidance may be considered, particularly when dealing with LAAs with complex anatomic features.
While we think that this technical innovation can be useful, a word of caution should be issued since late mechanical interaction between the devices is unknown and the number of patients and follow-up duration are limited. The small but existing risk of device embolisation during second device implantation must also be kept in mind.
In conclusion, due to individual anatomic variations, a single percutaneous device may not always adequately seal the LAA. In these cases, implantation of a second device either at the same or at an additional intervention may afford a good anatomical result. Larger cohorts are needed to corroborate the safety and efficacy of this technical innovation.
| Impact on daily practice Complete percutaneous occlusion of the LAA is not always achieved with the implantation of one single device. The technique of multiple device implantation may overcome this limitation and potentially widen LAA occlusion indications, by permitting occlusion of LAAs with large ostia or complex anatomy. |
Conflict of interest statement
B. Meier received research grants to the institution and speaker or proctor fees from St. Jude Medical. A. Khattab and F. Nietlispach received speaker or proctor fees from St. Jude Medical. The other authors have no conflicts of interest to declare.