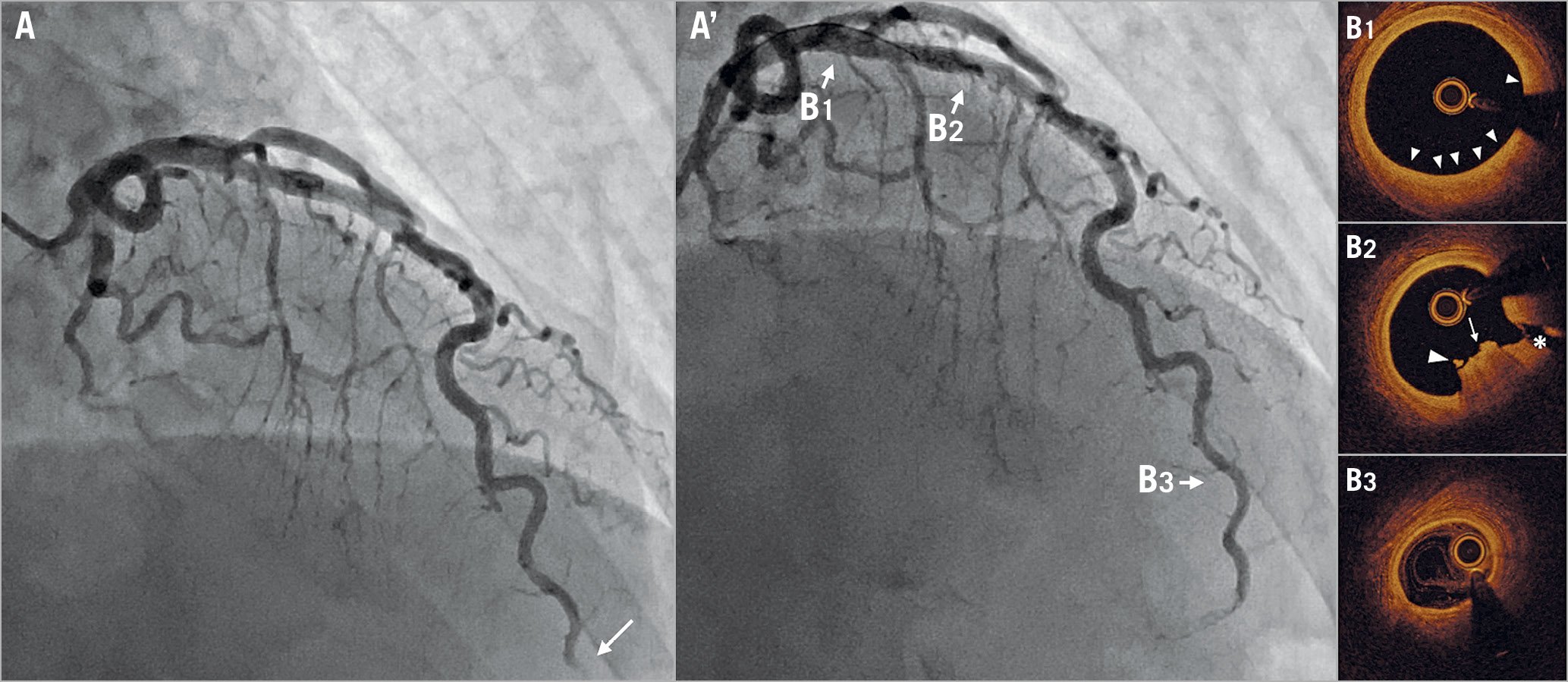
Figure 1. Coronary angiography and OCT images after thrombus aspiration from the distal portion of the LAD. Initial coronary angiography (A, Moving image 1) showed total occlusion at the distal portion of the LAD (arrow). Coronary flow was recovered after thrombus aspiration (A’). OCT pullback was from distal to proximal of the LAD. OCT pullback was performed twice to investigate the long lesions of the LAD. The first pullback was from the distal to the middle portion and the second pullback was from the middle portion to the guiding catheter (Moving image 2, Moving image 3). At the proximal segment, there was intimal hyperplasia (B1), and plaque erosion with thrombus (arrows), and the side branch (asterisk) were observed (B2). At the distal portion, three layers of coronary artery wall were maintained (B3).
A 56-year-old male, a current smoker with dyslipidaemia, was admitted to our hospital because of anterior ST-segment elevation myocardial infarction (STEMI). An echocardiogram showed akinesis in the apex of the left ventricle, and the ejection fraction was 55%. There was no evidence of atrial fibrillation, cardiac shunts or any cardiac thrombus. He had no history of emotional stress, cocaine intake or thrombophilia. Also, there was no episode to indicate suspected coronary spasm. After administration of aspirin 200 mg and prasugrel 20 mg, an emergent coronary angiogram (CAG) was performed. This showed total occlusion at the distal portion of the left anterior descending artery (LAD) (Figure 1A, Moving image 1). Manual thrombus aspiration was performed, and small red thrombi were aspirated.
After manual thrombus aspiration, a coronary angiogram showed Thrombolysis In Myocardial Infarction (TIMI) 3 flow; then optical coherence tomography (OCT) was performed on the LAD (Moving image 2, Moving image 3). Because the occluded site was far distal, the OCT catheter could not reach there. The OCT image showed intimal hyperplasia at the proximal portion of the LAD (Figure 1A’-B1). Plaque erosion with thrombus was also observed at the proximal site of the LAD (Figure 1A’-B2). There was no evidence of the embolic source at the distal portion (Figure 1A’-B3).
According to the OCT findings, it was speculated that the aetiology of STEMI in this case was spontaneous distal embolism (DE) from the proximal plaque erosion. Based on the OCT findings, no other procedures were added because the angiogram showed residual stenosis <50%. After the end of the procedure, dual antiplatelet therapy (aspirin 100 mg/day and clopidogrel 75 mg/day) was started. He was able to be discharged without a heart attack after the procedure. Antiplatelet therapy without stenting might be an effective optional therapy for STEMI patients with plaque erosion and residual stenosis <70%1. DE from erosion or ruptured plaque occurs spontaneously in acute coronary syndromes, or iatrogenically during percutaneous coronary interventions2. DE refers to the detachment of atherothrombotic fragments from the atherosclerotic plaque and their dislodgement downstream from the peripheral portion of the coronary tree. This consequently induces microvascular obstruction. Patients with DE, including procedural and/or spontaneous DE, have a worse prognosis than those without DE3. OCT is a useful tool not only for the diagnosis of DE for patients without significant stenosis at the proximal portion of the infarct-related artery, but also to facilitate treatment strategies.
Conflict of interest statement
T. Akasaka has received lecture fees and research grants from Abbott Vascular Japan. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Initial coronary angiogram. Total occlusion at the distal site of the left descending artery.
Moving image 2. OCT pullback from the distal to middle portion of the LAD after manual thrombus aspiration. There was no evidence of the embolic source.
Moving image 3. OCT pullback from the middle portion of the LAD to the guiding catheter after manual thrombus aspiration. Plaque erosion was observed at the proximal portion of the LAD.