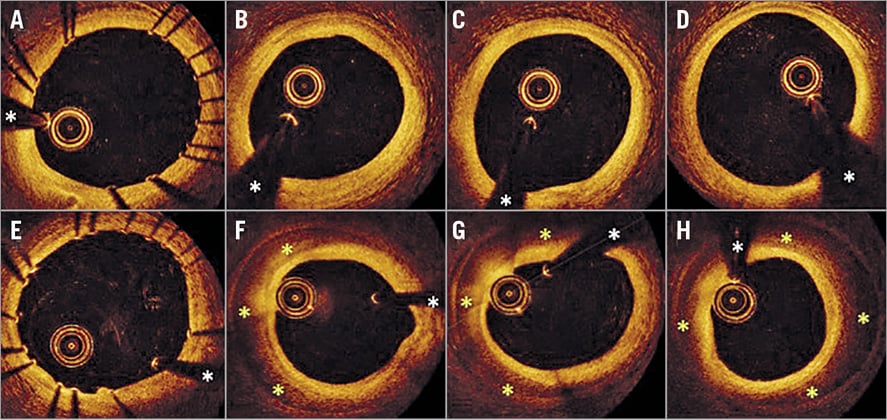
Figure 1. OCT findings. A) - D) Images obtained immediately after DES implantation. A) Distal edge of the stent. B) - D) Distal reference vessel (at 3 mm intervals) with intimal thickening and a mild fibrotic plaque. E) - H) OCT findings at repeat imaging. E) Distal edge of the stent. F) - H) An IMH (yellow *) with a preserved coronary lumen is clearly depicted. *wire artefact.
A 55-year-old man presented with an inferior myocardial infarction successfully treated with fibrinolysis. Elective coronary angiography revealed a tight lesion at the most proximal segment of the right coronary artery (Moving image 1). Following lesion predilation, a drug-eluting stent (DES) was implanted and subsequently optimised using optical coherence tomography (OCT) guidance (Moving image 2). OCT confirmed an excellent final result. In particular, the distal edge of the stent was nicely expanded and apposed against the vessel wall and no edge dissections were detected (Figure 1A-Figure 1D, Moving image 3). Six hours after the procedure, however, the patient presented abrupt prolonged angina with transient inferior ECG ST-elevation, which resolved after nitroglycerine administration. Urgent coronary angiography demonstrated an excellent appearance of the DES. However, the segment immediately distal to the DES showed a very subtle lumen narrowing that persisted despite repeated intracoronary nitroglycerine administration (Moving image 4). OCT revealed the presence of a novel intramural haematoma (IMH), starting at the distal edge of the stent with a length of 14 mm and a wide residual coronary lumen (Figure 1E, Figure 1F, Moving image 5). No entry tear could be identified. Since there was no significant coronary obstruction and the patient remained asymptomatic, conservative treatment was undertaken. Subsequently the patient had an uneventful clinical course.
Edge dissections or IMH may complicate stent implantation1-3. In many cases these are very subtle on angiography although they may eventually progress and cause severe ischaemia. In this setting, intravascular ultrasound and, more recently, OCT provide unique insights for the accurate diagnosis of edge dissections or IMH, helping in the clinical decision-making process2-4. It has been reported that about one third of IMH identified by intravascular imaging show no angiographic abnormalities4. However, the “delayed” appearance of IMH in a patient with optimal OCT results immediately after DES implantation has not been reported previously. Although its aetiology remains unknown, delayed intramural bleeding as a result of the previous barotrauma might be implicated. Leaking microvessels could not be detected. However, bend location or hinge phenomena might have been implicated. Transient associated vasospasm could also have played a role in the clinical manifestations. This unique entity should be kept in mind in patients with recurrent ischaemia after intervention.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Post-fibrinolysis coronary angiography showing a severe thrombotic lesion at the proximal segment of the right coronary artery.
Moving image 2. Immediate post-PCI coronary angiogram.
Moving image 3. Final OCT pullback immediately after stent implantation and optimisation. Bookmarks: 1: side branch; 2: subtle intima irregularity; 3: white thrombus intrastent prolapse.
Moving image 4. Six hours after PCI, right coronary angiography showing a very subtle lumen narrowing distal to previous stent.
Moving image 5. OCT pullback performed six hours after stent implantation unravelling distal edge IMH. Bookmarks: 1: minor side branch; 2: distal IMH; 3: proximal IMH; 4: distal stent edge.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Post-fibrinolysis coronary angiography showing a severe thrombotic lesion at the proximal segment of the right coronary artery.
Moving image 2. Immediate post-PCI coronary angiogram.
Moving image 3. Final OCT pullback immediately after stent implantation and optimisation. Bookmarks: 1: side branch; 2: subtle intima irregularity; 3: white thrombus intrastent prolapse.video3
Moving image 4. Six hours after PCI, right coronary angiography showing a very subtle lumen narrowing distal to previous stent.
Moving image 5. OCT pullback performed six hours after stent implantation unravelling distal edge IMH. Bookmarks: 1: minor side branch; 2: distal IMH; 3: proximal IMH; 4: distal stent edge.