Angiography of a 63-year-old male patient with unstable angina revealed a tight stenosis in the mid right coronary artery, proximal to a formerly implanted drug-eluting stent (DES). A motorised pullback of the pressure wire at 1 mm/sec during IV adenosine (140 μg/kg/min) permitted co-registration of the pressure-derived fractional flow reserve (FFR) signal along the angiographic roadmap, and the precise length (12 mm) of the segment where the pressure “jump” was derived. Additional OCT co-registration was performed revealing extensive spiral dissection at the proximal edge of the stent, extending for 23 mm proximally, and not detectable by angiography on any view (Figure 1, Moving image 1). FFR-OCT co-registration, empowered by 3-D QCA software, is currently feasible and has the potential to integrate anatomical and functional data for procedural guidance and treatment decision making.
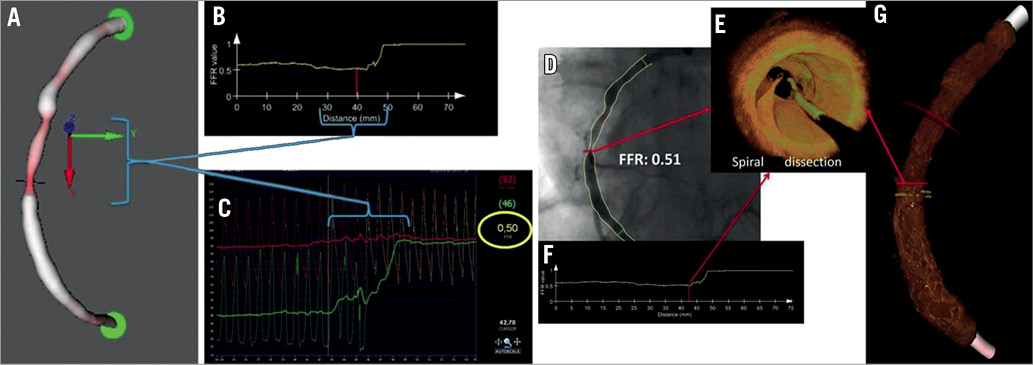
Figure 1. A) 3-D reconstruction of the mid RCA. Horizontal line indicates minimal luminal area. B) Representation of the motorised FFR pullback. The X axis shows the distance in mm from its distal position at the onset of the pullback to the tip of the guiding catheter while the FFR value is shown on the vertical axis. A significant pressure increase is seen while the sensor is pulled away from the stenotic segment. The red line corresponds to the smallest area, as indicated on Panel A. C) Beat to beat high-resolution pressure tracings of both distal and proximal intracoronary pressures. The pressure “jump” starts at the level of minimum area and increases gradually over 12 mm until the pressure gradient nearly disappears. The length of the segment causing the pressure drop is indicated on Panels A, B and C. D) Angiography shows no dissection. The FFR value is indicated at the level of the maximal stenosis of the mid RCA. FFR values are indicated on line as the cursor is moved along the vessel. E) 3-D OCT reconstruction of the segment corresponding to the maximal stenosis which reveals a spiral dissection extending proximally into the vessel. F) Representation of the motorised FFR pullback for correlation with OCT imaging. G) Bent 3-D OCT model of mid RCA (the red arrow indicates the maximal stenosis corresponding to the beginning of the FFR “jump” in Panel F.
Conflict of interest statement
S. Tu is employed by Medis medical imaging systems bv and has a research appointment at the Leiden University Medical Center (LUMC). J.H.C. Reiber is the CEO of Medis medical imaging systems bv, and has a part-time appointment at LUMC. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Combined morphological-functional assessment of the RCA at baseline using three diagnostic modalities (3-D QCA, FFR and OCT). The red marker is moving simultaneously in the different panels and corresponds to functional evaluation by FFR and anatomic evaluation by OCT, along with the epicardial vessel localisation on the 3-D QCA roadmap. The FFR value was 0.51 distally and abruptly increased to near normal levels, 12 mm along the stenosis, as shown by 3-D QCA and OCT. The substrate of the stenosis is recognised by OCT imaging as a spiral dissection, extending from the proximal edge of the previously implanted stent, towards the mid RCA. 3-D QCA: three-dimensional quantitative coronary angiography; FFR: pressure-derived fractional flow reserve; OCT: optical coherence tomography

