Over the last three decades, developments in intravascular ultrasound (IVUS) and optical coherence tomography (OCT) have advanced our understanding of coronary disease pathophysiology and improved outcomes of percutaneous coronary intervention (PCI) procedures. Although in daily clinical practice most imaging utilisation relies on a simple, two-dimensional display of cross-sectional coronary images, real-time three-dimensional (3D) visualisation of coronary arteries with OCT offers advantages over and above simple vessel sizing and plaque characterisation.
Fourier domain OCT, with superior axial (10-15 µm) and lateral (20-40 µm) resolutions and a faster image acquisition rate (180 scans/second), as well as quicker pullback speeds (18 or 36 mm/second), permits clear and interactive 3D reconstructions of the coronary anatomy and its relationship with intraluminal devices. Since the first report on 3D OCT coronary images in 20081, the field has rapidly evolved. Appealing imaging applications have emerged2,3, particularly in coronary bifurcation PCI, where 3D images can be used to confirm wire recrossing through the distal stent cell into a side branch4, the status of side branch ostia jailed by a main branch stent can be understood5, and modifications created in the stent geometry after kissing balloon inflation can be evaluated2,6. While these are a valuable add-on for the high-volume expert user, none of such advanced 3D applications has been shown to affect PCI outcomes, and trials testing such a hypothesis will likely never occur. Nevertheless, as the field continues to evolve, there will always be a drive for new 3D OCT imaging applications.
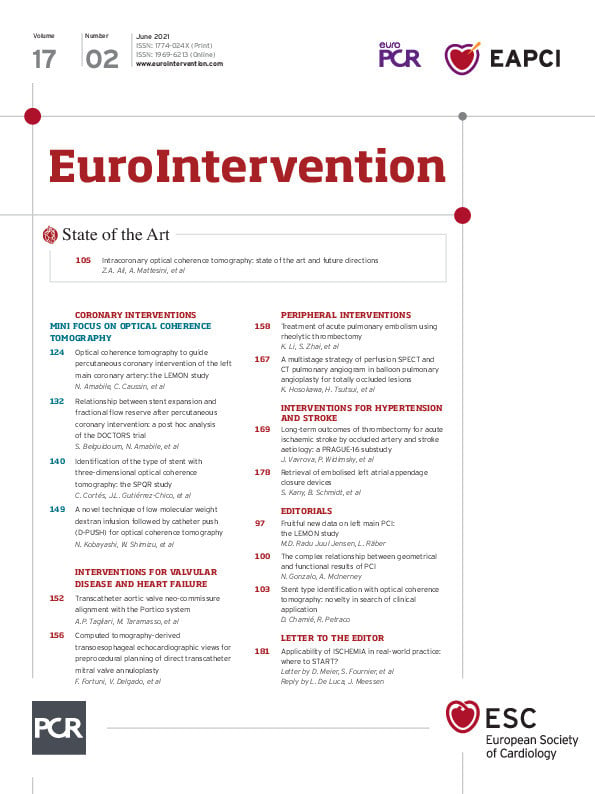
In the current issue of EuroIntervention, Cortés et al present the results of the SPQR study7, in which 294 metallic stent or scaffold platforms were analysed by two imaging experts aiming to identify the precise stent/scaffold type correctly based on its 3D appearance in commercially available OCT consoles (ILUMIEN™ OPTIS™ E5; Abbott Vascular, Santa Clara, CA, USA).
The investigators propose a predefined four-step approach, of which three depend upon automatic strut detection, and two rely on additional imaging post-processing. Information gathered from the 3D visualisation of stent patterns is then used to identify the stent type. By following such a protocol, the investigators correctly identified 96.9% of the stents (κ=0.965) with an excellent interobserver agreement (κ=0.988). These results illustrate the high-quality images provided by the current OCT system as well as the expertise of the investigators.
Perhaps not surprisingly, the identification performance was slightly better in recently implanted stents when compared with stents implanted more than three months before (κ=0.993 vs κ=0.915). This finding reflects the limitations of the current algorithm in detecting struts buried deeply into tissue in restenotic cases. In this situation, the 3D tissue view, which does not apply automatic strut detection and relies mainly on the shadows cast by metallic struts onto the vascular surface, is also of limited utility. Although the authors demonstrated that only a small segment of a stent away from thick neointimal coverage is sufficient for correctly identifying the stent type, the current system remains limited in providing quantitative 3D metrics on stent expansion in restenotic sites.
Another interesting finding was the better stent recognition performance in OCT images acquired with a pullback speed of 18 mm/s (0.1 mm sampling rate) when compared to 36 mm/s (0.2 mm sampling rate) (κ=0.969 vs κ=0.940). Slower pullback speeds generate more refined 3D rendering at the expense of more frequent cardiac motion artefacts3. As just a small segment of a stent was necessary for type identification, the presence of motion artefacts did not affect the ability of experienced observers to label the stents correctly. Less experienced OCT users would probably find it more challenging to differentiate such motion artefacts from true stent geometry distortions.
The authors undeniably present a breathtaking imaging atlas of a large number of stent platforms7. However, questions remain as to the feasibility of their proposed approach in real-world clinical practice. Firstly, it is likely that their sample suffered from selection bias in order to include most stent platforms in the study. The study also failed to provide independent separate training and validation data sets for their approach to be tested. Almost certainly, in daily practice where their algorithm would be exposed to an “all-comers” population of stents and disease processes, stent type recognition would not be as accurate. Also, it is nearly impossible for interventional cardiologists to remember all stent design characteristics, particularly since some stent platforms have very similar designs. Most operators would have to review their proposed steps for stent type recognition during PCI, compare them against a large imaging repository, and still end up with uncertainties, adding delays and possibly costs to the procedure. In this scenario, considering the extensive catalogue of existing stent types (and the new ones yet to come), a machine learning approach to stent identification might be better suited for the job. A system based on artificial intelligence (AI) would allow the knowledge of OCT experts to be automatically available to interventional cardiologists of all levels of imaging expertise.
Identification of potential mechanisms of stent failure with intravascular imaging is crucial and recommended by international guidelines8. However, the key question is whether the identification of the precise stent type would add any practice-changing value to the mechanistic information already provided by standard OCT runs. Would the specific knowledge of stent type help operators in cases of stent thrombosis or restenosis? Individualised decisions on using the same or a different stent platform might sound intuitive, but data supporting specific strategies are scarce8. Until we find a niche role for its utilisation and the process becomes automatic and operator-independent, 3D OCT-derived stent type identification will remain an exciting novelty in search of an actual clinical application.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.