A 42-year-old diabetic male presented with new onset typical cardiac chest pain. There were no ischaemic ECG changes and troponin was 0.13 ng/ml. Angiography showed a 60-70% lesion in the mid left anterior descending (LAD) artery without other lesions. Fractional flow reserve (FFR) evaluation was performed with a baseline pressure gradient of 0.94 (Figure 1) and FFR 0.89 despite increasing iv adenosine infusion from 140 to 180 mcg/kg/min and additional intracoronary adenosine (120, 240 and 360 mcg). Optical coherence tomography (OCT) showed a large thrombus burden in the mid LAD (MLD 1.27 mm, MLA 1.8 mm2) (Appendix Figure 1, Moving image 1). PCI with a drug-eluting stent was performed.
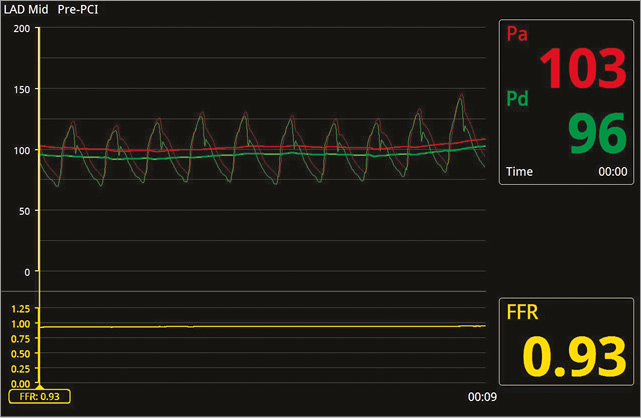
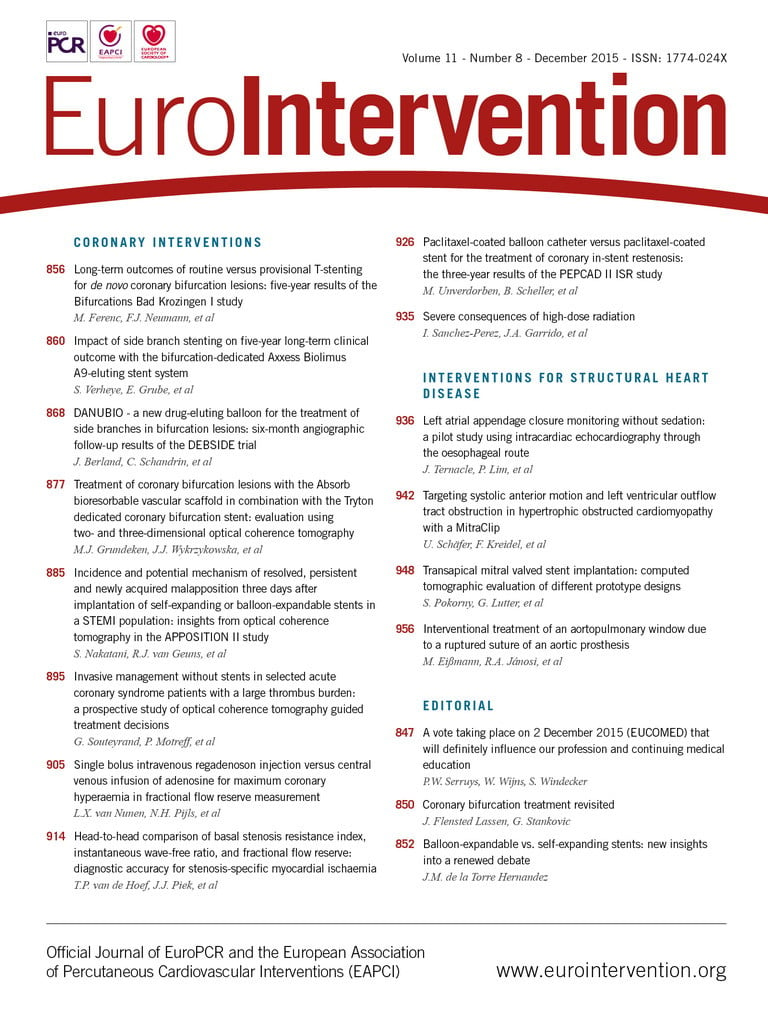
Figure 1. Baseline gradient (Pd/Pa) across mid LAD lesion.
A recent randomised trial suggested a role for FFR-guided management in acute coronary syndrome (ACS). In individual cases, hyperaemic flow may still be adequate to allow a “normal” FFR because other mechanisms have produced ischaemia, such as in the current case where the presence of fresh thrombus produced the ACS with an increased risk of adverse events. Given concerns about FFR measurement in ACS, probably secondary to an inability to achieve maximal hyperaemia, caution is warranted in interpreting FFR in such cases. Intracoronary imaging appears useful in such intermediate ACS cases.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. OCT imaging run of distal to proximal LAD.
Appendix Figure 1. 70% stenosis in mid LAD on angiography. FFR of LAD 0.89. OCT imaging demonstrating normal-appearing vessel with large lumen (MLA 12.6 mm2, MLD 3.8 mm in the proximal LAD [A], and MLA 8.5 mm2, MLD 3.12 mm in the distal LAD [D]). Large red thrombus in the mid LAD (B & C) with significantly compromised lumen (MLA 1.8 mm2, MLD 1.2 mm).
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. OCT imaging run of distal to proximal LAD.