Abstract
Aims: Coronary revascularisation based upon physiological evaluation of lesions improves clinical outcomes. Angiographic or visual stenosis assessment alone is insufficient in predicting haemodynamic stenosis severity by fractional flow reserve (FFR) and therefore cannot be used to guide revascularisation, particularly in the lesion subset <70%. Accordingly, we sought to identify independent determinants of angiographic intermediate lesions with haemodynamic significance.
Methods and results: We assessed consecutive intermediate lesions for patients from January 2014 to April 2015 at our institution. Independent predictors of FFR positivity (FFR ≤0.8) were identified and a scoring system formulated. Of 1,023 consecutive lesions (883 patients), 314 (31%) were haemodynamically significant. Characteristics associated with FFR ≤0.8 include male gender, higher SYNTAX score, lesions ≥20 mm, stenosis >50%, bifurcation, calcification, absence of tortuosity and smaller reference diameter. A user-friendly integer score was developed with the five variables demonstrating the strongest association. On prospective validation (in 279 distinct lesions), the increasing value of the score correlated well with increasing haemodynamic significance (C-statistic 0.85).
Conclusions: We identified several clinical and angiographic characteristics and formulated a scoring system to guide the approach to intermediate lesions. This may translate into cost savings. Larger studies with prospective validation are required to confirm our results.
Abbreviations
ACC: American College of Cardiology
AHA: American Heart Association
FFR: fractional flow reserve
PCI: percutaneous coronary intervention
QCA: quantitative coronary angiography
Introduction
Fractional flow reserve (FFR) is defined as the ratio of maximal achievable blood flow in a coronary artery in the presence of a stenosis to the hypothetical maximal achievable blood flow in that same epicardial artery in the absence of the stenosis. The data available at this time suggest that FFR-guided PCI not only decreases the combined rate of death and MI, but also translates into significantly fewer stents deployed and significantly less contrast used1-3, salutary clinical benefits that translate to lower costs. Current ACC/AHA guidelines place FFR as class IIa to assess angiographic intermediate coronary lesions (50% to 70% diameter stenosis) in patients with stable ischaemic heart disease4. Despite these guidelines, routine FFR assessment in every patient with angiographic intermediate lesions appears economically prohibitive. Many operators still rely, or are forced to rely, solely on the coronary angiogram because of economic restrictions or a lack of reimbursement for FFR in an inpatient setting5. Clinical and angiographic predictors of functional significance may add value in this scenario, particularly in selecting patients who will benefit most from invasive haemodynamic evaluation. This may translate into cost-effective care. To date, there are very few studies that have attempted to determine such predictors6-9. However, they include a homogenous population with evaluation of only limited clinical or angiographic characteristics. In the current study, we have attempted to evaluate the FFR predictivity in a more heterogeneous group with multiple clinical and angiographic characteristics from a richer data source. The unique feature of our study is investigation of the FFR predictors by both visual analysis (“eyeballing”) and quantitative coronary angiography (QCA). While visual assessment is a closer simulation of daily practice, quantitative analysis facilitates the development of a prediction score. We hypothesise that our clinical and angiographic integrative score would have incremental value in predicting haemodynamic significance in angiographic intermediate coronary lesions.
Methods
We assessed consecutive angiograms for patients who had elective or urgent coronary angiography and FFR evaluation from January 2014 to April 2015 at our institution (n=1,063). Patients with cardiogenic shock, significant arrhythmias, unable to tolerate adenosine, left main disease, graft lesions, in-stent restenosis, less than TIMI 3 flow, unable to wire and with angiographic stenosis less than 30% and more than 80% were excluded (n=180 patients). The ACS culprit artery was not included in the analysis (Figure 1). All clinical and procedural data were prospectively stored in a dedicated electronic database and were retrospectively analysed in this study. Using a temporal validation cohort, we subsequently reviewed additional angiograms in a prospective fashion to grade the five variables included in the scoring system (May 2015 up to August 2015). Three hundred lesions were reviewed, of which 279 met the inclusion criteria and were utilised for angiographic analysis.
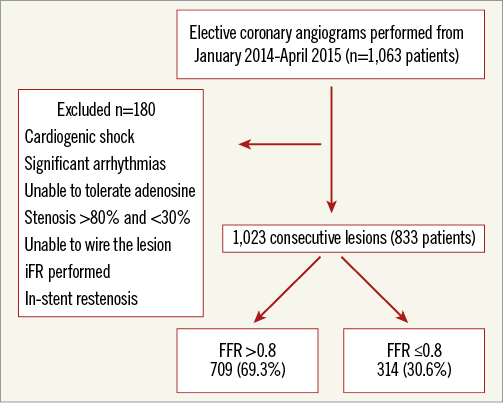
Figure 1. Patient disposition. Flow chart depicting patients and lesions to arrive at the target population for risk score development.
Qualitative and quantitative angiographic analyses of every lesion were performed with determination of specific characteristics, including lesion percentage stenosis (30-50%, 50-70%, >70%), lesion length (<10 mm, 10-20 mm, 20-40 mm, >40 mm), vessel tortuosity proximal to the lesion (mild, moderate or severe), angiographic grade of calcification (none-mild, moderate, severe), presence of bifurcation lesion (presence of side branch stenosis of ≥50% with vessel diameter ≥1.5 mm) and reference vessel diameter (<2.5 mm, 2.5-3 mm, 3-3.5 mm, >3.5 mm), presence of collaterals from the lesion vessel, presence of aorto-ostial disease, dominance pattern, presence of multivessel coronary artery disease (CAD) and SYNTAX score. For each procedure, a SYNTAX score was calculated that included lesions with at least 50% stenosis based upon anatomic and morphologic details entered into the electronic catheterisation reporting system. Additional QCA of 942 lesions for reference vessel diameter, lesion percentage stenosis and lesion length was recorded. QCA was performed for target lesions before intervention using dedicated software (QAngioXA 7.3; Medis, Leiden, the Netherlands) to calculate reference lumen diameter, percent diameter stenosis and lesion length. A standard analytic protocol developed in collaboration with Medis was used by experienced analysts (NS and UB).
Coronary pressure was measured using a 0.014” sensor-tipped percutaneous intervention guidewire manufactured by St. Jude Medical. The wire was introduced through a 5 to 7 Fr guiding catheter, equalised in the aorta, and advanced distal to the stenosis. The FFR value was measured after administering adenosine to induce maximal hyperaemia intravenously (≥140 µg/kg/min) for a maximum of three minutes. Administration of adenosine through a peripheral intravenous line was performed uniformly in the study. Stenoses with FFR measurements ≤0.80 were considered ischaemia-causing lesions.
STATISTICAL ANALYSIS
Baseline characteristics were summarised as means (standard deviations) or counts (percentage) and compared across FFR groups using the Student’s t-test or chi-square test. Independent predictors of a positive FFR were identified using multivariable logistic regression with backward elimination using an exit criterion of 0.1. For these models, candidate covariates included any parameter demonstrating a significant (p<0.05) difference between FFR groups, including age, gender, dyslipidaemia, prior MI, QCA percent stenosis, QCA lesion length, bifurcation, tortuosity (moderate/severe vs. none/mild), calcification (moderate/severe vs. none/mild), QCA reference vessel diameter, lesion location (proximal versus non-proximal) and presence of collaterals. The strength of association between each independent parameter and outcome was quantified using the Wald chi-square statistic. To account for intra-patient correlation, patient was introduced as a random effect. As a sensitivity analysis, we repeated model development restricted to a single lesion per patient, which yielded the same predictors as our primary analysis.
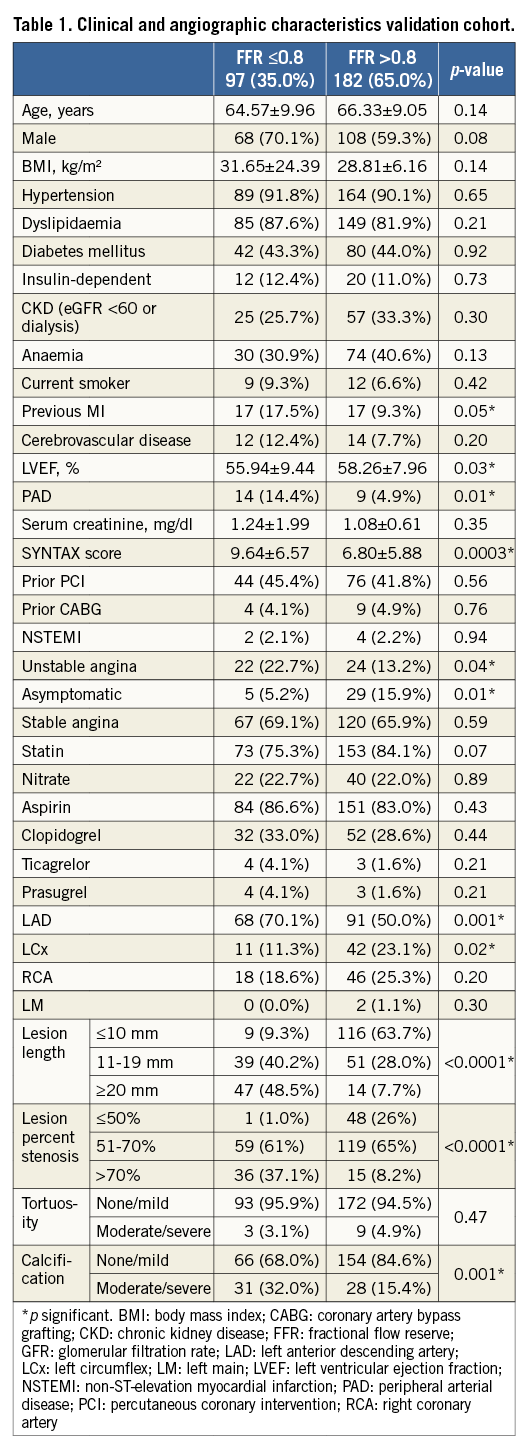
To develop a simple user-friendly integer risk score, we first generated a parsimonious model that only included those parameters demonstrating the strongest associations, as assessed by the Wald chi-square statistic, with the dependent outcome of positive FFR. Integer scores were calculated using the method of Sullivan et al, which is a common approach to generate scoring systems such as the Framingham risk model. In this approach, model-based parameter estimates are converted to integers after being weighted by the adjusted regression coefficients. Thus, regression coefficients are converted to user-friendly integers that may be summed to generate an overall score10. The distribution of the risk score was plotted and visualised for the entire population. Patients were grouped by risk score quartile, and the frequency of predicted and observed positive FFR values was compared across groups. Model discrimination for positive FFR was quantified as the area under the receiver operating characteristic curve (C-statistic), and calibration was assessed using the Hosmer-Lemeshow goodness of fit test. The same analysis was performed for a separate prospective cohort for the time period of May 2015 up to August 2015 for validation purposes. We have presented the clinical and angiographic characteristics of this cohort in Table 1. This group comprised patients with an average age of 65 years, primarily males, with a predominance of hypertension (90%), dyslipidaemia (87%) and diabetes mellitus (DM) (44%), consistent with the derivation population.
Results
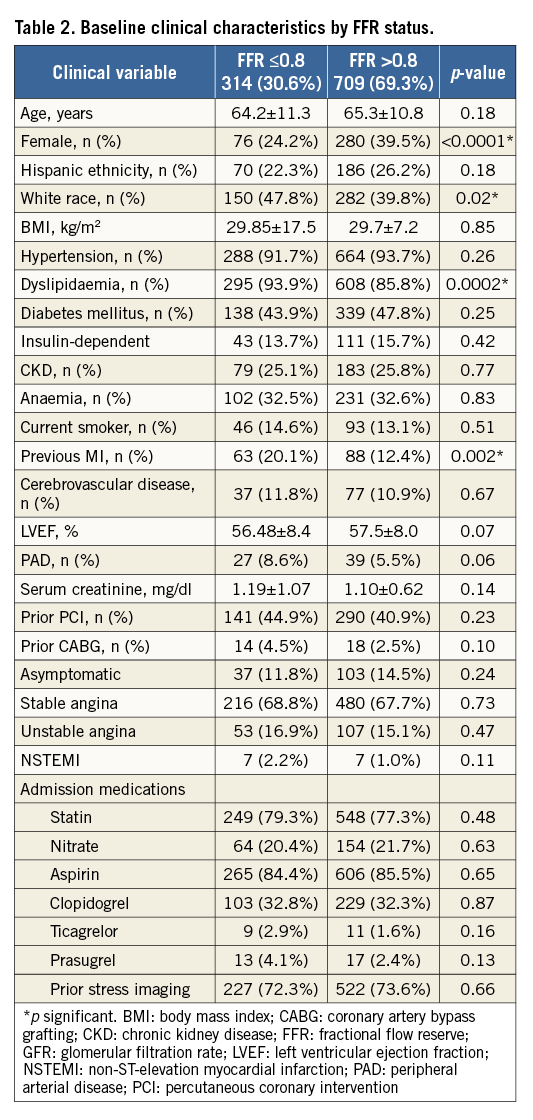
One thousand and twenty-three consecutive lesions were identified in 883 patients, of which 314 (31%) lesions were haemodynamically significant. Baseline characteristics stratified by the presence or absence of positive FFR are presented in Table 2. Patients with a positive FFR were more often male, with a higher prevalence of dyslipidaemia, prior MI and peripheral artery disease compared to their counterparts with a negative FFR. In contrast, there were no significant differences between groups in age or prevalence of DM.
Almost a third of the lesions were bifurcation lesions, 13% were moderately to severely tortuous and almost a fourth were moderately to severely calcified. Triple-vessel disease was seen in 10% and collateral supply in 3.5% of lesions; 90% were right dominant.
Based upon our analysis, the clinical parameters which were more likely associated with haemodynamic significance (Table 2) in angiographic intermediate lesions were female sex (24.2% versus 39.5%), presence of dyslipidaemia (93.9% versus 85.8%) and previous myocardial infarction (MI) (20.1% versus 12.4%). A trend towards functional significance was seen in the absence of DM (44% versus 48%). No significant effect was seen with patient height, weight, presence of hypertension, chronic renal insufficiency, known peripheral arterial disease, prior cerebrovascular events, prior MI, prior coronary artery bypass grafting, anaemia or smoking status.
The presence of bifurcation (42% versus 57.5%) and moderate to severe calcification (36% versus 20.3%) at the lesion site was associated with an FFR value ≤0.8 (Table 3). Smaller reference vessel diameter lesions, presence of multivessel coronary artery disease and collaterals from the lesion were all associated with haemodynamic significance. Lack of tortuosity proximal to the lesion was associated with significant FFR. Dominance had no impact on the haemodynamic significance of the lesion. Table 4 summarises the covariates for haemodynamically significant intermediate angiographic lesions in our study.
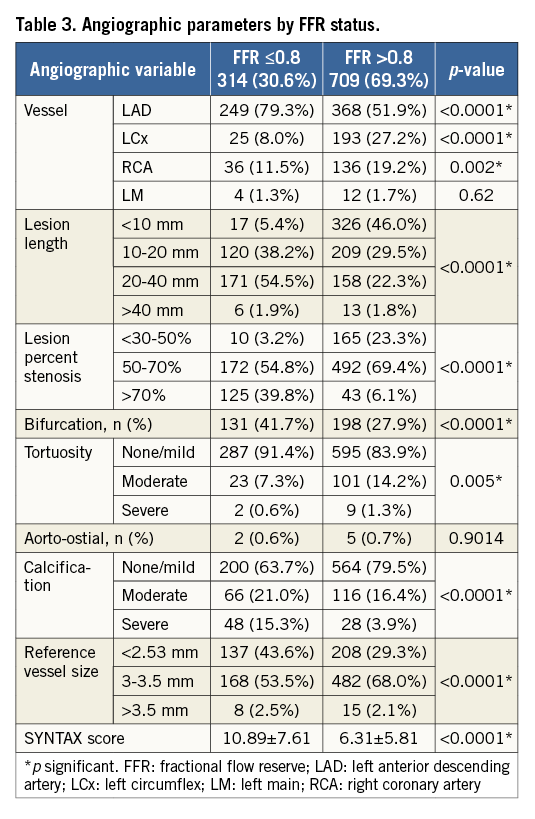
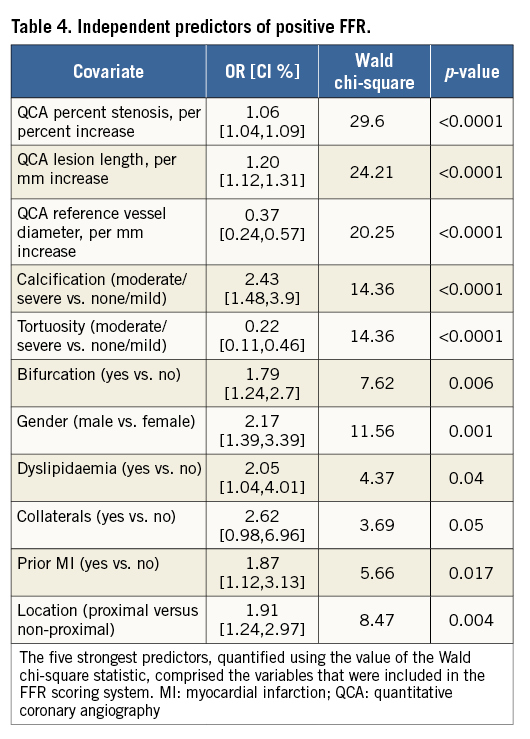
Based upon the analysis, percent stenosis, lesion length, presence of calcification, smaller reference vessel diameter and absence of tortuosity emerged as being most predictive of haemodynamic significance (Table 5). Table 6 details the point scoring system to predict positive FFR. As the score of the lesion based upon our scoring system increased, the frequency of haemodynamic significance was increased. Figure 2 represents distribution of the score in the population. We divided all the lesions into four quartiles (Q1-4) based upon the score (Q1: 3-16, Q2: 17-18, Q3: 19-23, Q4: 24-39) (Figure 3). While 14% of lesions with a score of 316 (quartile 1) were FFR positive, almost 52% were haemodynamically significant in the highest quartile (score 24-39). The observed frequency of positive FFR was comparable to the probability-based estimates, indicating adequate model fit. On prospective validation, the increasing value of the integer-based risk score correlated well with increasing haemodynamic significance, as demonstrated in Figure 4. Furthermore, to show the utility of our scoring system to discriminate FFR positivity, we also generated receiver operating characteristic (ROC) curves for the derivation and validation cohorts showing the C-statistics in both populations (Figure 5A, Figure 5B). Discrimination C-statistics were 0.81 and 0.85, respectively. A scatter plot depicting the score values with FFR (r=-0.33) can be found in Figure 6.
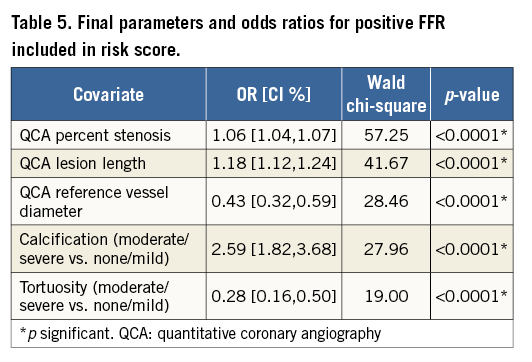
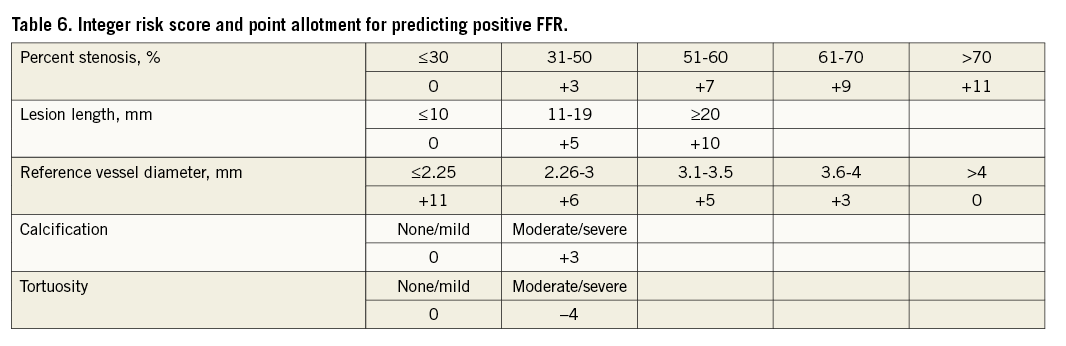
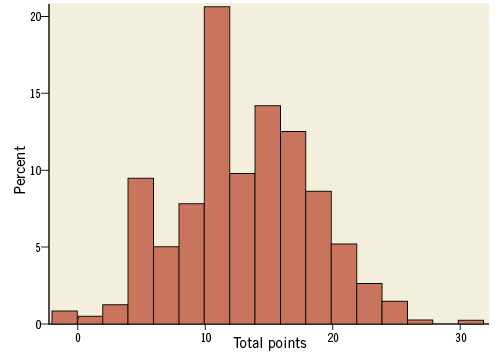
Figure 2. Risk score histogram. Histogram showing distribution of integer risk scores in the development cohort.
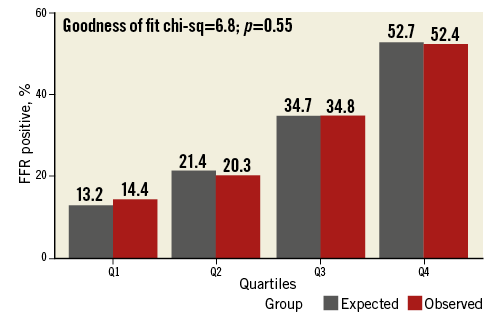
Figure 3. Observed and predicted positive fractional flow reserve by integer. Bar graph depicting the frequency of observed and predicted positive FFR in the development cohort as a function of integer risk score quartile (Q1: 3-16, Q2: 17-18, Q3: 19-23, Q4: 24-39).
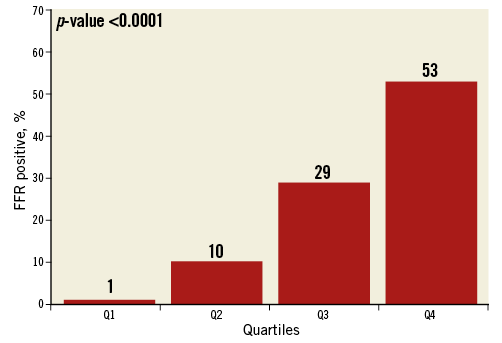
Figure 4. Integer risk score validation. Frequency of positive fractional flow reserve value by integer risk score quartile in prospective validation cohort.
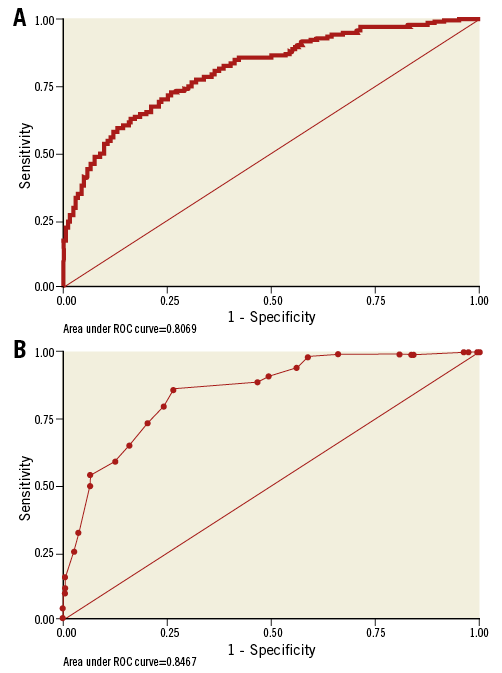
Figure 5. Receiver operating characteristic curves for positive fractional flow reserve (FFR) based upon risk model and integer risk score in the derivation (A) and validation (B) cohorts, respectively.
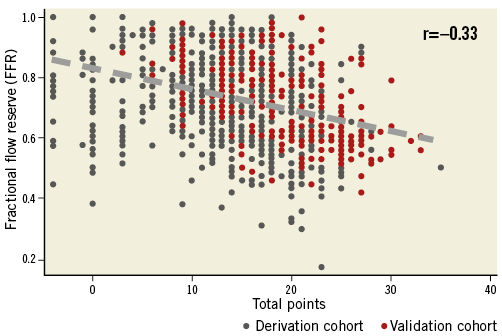
Figure 6. A scatter plot depicting the score values with FFR (r=–0.33).
Discussion
In this study comprising 883 patients and 1,023 coronary lesions, we identified angiographic and clinical correlates of haemodynamic significance in intermediate lesions on coronary angiography. In addition, we also derived a simple, user-friendly integer risk score that includes variables with the strongest association to haemodynamic significance.
Several previous studies have examined predictors of haemodynamic significance in angiographic intermediate lesions. The limitations of previous reports include modest sample size, limited number of variables and a homogenous patient population6-9. In contrast, we conducted a detailed, lesion-level quantitative and qualitative analysis in 1,023 consecutive coronary lesions. This is a relevant strength of our study, as even experienced interventional cardiologists have been shown to overestimate intermediate stenoses on visual assessment11, emphasising the importance of QCA. Moreover, we also considered many clinical variables as candidate predictors.
The lesion-specific angiographic predictors recognised in our analysis correspond to findings from prior studies6-9. Presence of multivessel disease, longer lesions and lesions with higher visual percentage stenosis were more likely to be functionally significant. Lesion length is an important geometric variable positively correlated with the trans-stenotic pressure gradient. This finding corresponds to the fact that, under conditions of maximal hyperaemia, a direct relationship exists between the expected flow and the extent of myocardium supplied. This would also explain haemodynamic significance with supply of collaterals.
Novel findings from our analysis include the presence of bifurcation lesions and moderate to severe calcification as independent predictors of haemodynamic significance, associations that have not previously been reported. Bifurcation may contribute to flow divergence proximal to a stenotic segment, and calcification could be a representation of the plaque burden. Lack of tortuosity proximal to the lesion was associated with lower FFR. Dominance had no impact on the haemodynamic significance of the lesion.
Interestingly, while clinical parameters were recognised, the magnitude of their association was not as high as for angiographic predictors, a finding that is consistent with prior studies. One possible explanation is that the clinical predictors of haemodynamic significance may be mediated by the characteristics of the underlying lesion and vessel-specific parameters, thereby attenuating observed associations with clinical variables.
In addition to recognising predictors of haemodynamic significance, we also derived a risk score from a logistic regression model that only included those parameters with the strongest association with positive FFR. This may facilitate more selective use of FFR for those lesions most likely to demonstrate haemodynamic significance. Such utilisation might reduce costs, and avoid exposing patients to additional contrast media and anticoagulation. Nevertheless, such benefits are speculative at present.
Limitations
Some limitations of our study should be acknowledged. This is a retrospective, single-centre study. Minimal luminal diameter by QCA analysis was not collected as a data element in the current study. Improvement in functional indices during angioplasty has been shown to translate into functional improvement in LV function in patients with prior MI12. We recognise that we did not make an assessment as a part of this study to ensure viability of the subtended myocardium by the lesion under evaluation. There are data showing that there is validity of established FFR cut-off values for patients with chronic infarction and that, for a similar degree of stenosis, the value depends upon the mass of viable myocardium13,14.
Conclusions
We identified several clinical and angiographic characteristics and formulated a scoring system to guide the approach to intermediate lesions. Our scoring system will facilitate stratification of angiographic intermediate lesions. We have prospectively validated our results. This approach may translate into economic savings. While our findings are hypothesis-generating, larger studies are required to confirm our results.
| Impact on daily practice Careful attention to clinical and angiographic parameters may guide interventionists in haemodynamic stratification of angiographic intermediate lesions. Our scoring system may serve as a quick reference to facilitate clinical decision making in the utilisation of FFR in daily practice. |
Conflict of interest statement
The authors have no conflicts of interest to declare.