Abstract
Aims: Efficacy of combined intravascular ultrasound (IVUS) parameters in functional significance prediction and discrepancy between IVUS and fractional flow reserve (FFR) have not been well defined. This study therefore aimed to: 1) evaluate the diagnostic accuracy of combined IVUS parameters, namely minimal lumen area (MLA) and percent plaque burden (%PB), in functional significance prediction of coronary artery stenosis; and 2) define factors that affect the relation between FFR value and IVUS parameters.
Methods and results: At 11 international centres, IVUS and FFR measurements were concurrently performed in 945 major epicardial coronary artery lesions (886 patients). Functional significance was defined as FFR ≤0.8. MLA and FFR correlated weakly (r=0.289, p<0.001). Diagnostic accuracy of MLA ≤4.0 mm2, %PB >70% and their combination were 50%, 47% and 51%, respectively, with similar area under the curve (AUC) of 0.561, 0.511 and 0.516, respectively. The best cut-off values (BCV) were MLA ≤3.0 mm2 and %PB >75%, with accuracy of 60% for MLA, 50% for %PB and 56% for their combination, and AUC of 0.618, 0.511 and 0.533, respectively. MLA BCV ≤3.0 mm2 had higher predictive power than %PB BCV >75% or their combination. Independent predictors of functional significance were male gender (odds ratio 1.76 [95% confidence interval: 1.19-2.62]), left ventricular ejection fraction (LVEF, 0.98 [0.96-0.99]), LAD lesion (2.52 [1.73-3.67]), reference vessel diameter (0.60 [0.41-0.86]), lesion length (1.04 [1.02-1.06]) and MLA (0.79 [0.69-0.92]). False negative lesion incidence was 24.4% in association with race (for Asians, 0.391 [0.219-0.698]), LAD lesion (2.677 [1.709-4.191]) and LVEF (0.977 [0.957-0.997]). False positive lesion incidence was 17.0% in association with non-LAD lesion (2.444 [1.620-3.686]).
Conclusions: Combined IVUS parameters did not improve the accuracy of functional significance prediction. Discrepancy between IVUS and FFR, which was not rare, should be taken into account in clinical decision making.
Introduction
Although determination of the severity of coronary artery stenosis is the first step in coronary artery disease diagnosis, the accuracy of the available diagnostic tools remains under debate1. The inherent limitation of two-dimensional quantitative coronary angiography (QCA) to define functional severity has propelled the use of other modalities such as intravascular ultrasound (IVUS) which has become become one of most popular imaging techniques to assess angiographically ambiguous stenosis2-4. Although IVUS more accurately assesses lesions than QCA alone, there is no agreement on the accuracy of historical cut-off values for individual IVUS parameters such as minimal lumen area (MLA), percent plaque burden (%PB) and lesion length regardless of patient or lesion characteristics5-9. There have been recent attempts to clarify the IVUS parameter cut-off values that best define haemodynamically significant lesions using fractional flow reserve (FFR)10. Although the combination of MLA and %PB by IVUS appeared to predict functional significance better in small studies11,12, this has not been validated in a larger one. This study therefore aimed to: 1) evaluate the diagnostic accuracy of combined IVUS parameters, namely MLA and %PB, in functional significance prediction of coronary artery stenosis; and 2) define the factors which affect the relation between FFR value and IVUS parameters.
Methods
STUDY POPULATION
This international multicentre registry was performed at 11 centres (four in Korea, two in Japan, one in China, one in Singapore, two in the USA and one in Europe), all with ample experience in IVUS and FFR. This registry included previously published5,6,13,14 and unpublished data. All patients had de novo lesions with visual intermediate stenosis (30% to 70%) in non-left main major epicardial coronary arteries. IVUS and FFR measurements were simultaneously obtained in the lesion of interest. Lesions were excluded if any of the following conditions were present: left main disease, prior coronary artery bypass graft surgery, additional stenosis (>30% by visual estimation) in the same vessel, left ventricular ejection fraction <35%, primary myocardial or valvular disease, and culprit vessel in the setting of acute myocardial infarction. The study protocol was approved by each institutional review board and all patients provided written informed consent.
Data analysis
The target vessel was engaged using a 5 Fr-7 Fr guiding catheter. QCA data were analysed by an independent technician blinded to the result. After acquiring optimal projections, QCA analysis including reference vessel diameter, minimal lumen diameter, lesion length and percent diameter stenosis was performed at each participating centre by computer-assisted analysis. IVUS imaging was obtained in a standard fashion using an automated motorised pullback system (0.5 mm/s) with either of two commercially available imaging catheters (Boston Scientific/SCIMED, Minneapolis, MN, USA, or Volcano Corp., Rancho Cordova, CA, USA). MLA was measured by a skilled specialist at each centre and obtained at the site of the smallest lumen, and %PB was calculated as: (100× [vessel area at MLA site-MLA]/vessel area at MLA site)15.
FFR was measured using a 0.014 inch pressure guidewire (St. Jude Medical, St. Paul, MN, USA, or Volcano Corp.). Maximum hyperaemia was induced according to the standard protocol of each individual centre. Hyperaemia was induced with adenosine in 92.1% and papaverine in 7.9% of cases using: intravenous continuous infusion of adenosine (140-220 μg/kg/min) via central or antecubital vein; intracoronary continuous infusion of adenosine (240 μg/min); intracoronary bolus injection of adenosine (12-80 μg into the left coronary artery, 8-40 μg into the right coronary artery); or intracoronary bolus injection of papaverine (20 μg)16. The lesion was considered functionally significant when FFR was ≤0.817,18. In addition to IVUS and FFR analysis, detailed data on baseline demographic and clinical characteristics were submitted to the data management core laboratory at Seoul National University Cardiovascular Centre.
Statistical analysis
Data are presented as means±standard deviations for continuous variables and frequencies for categorical variables. Student’s t and chi-square tests were used to compare continuous and categorical variables, respectively. Correlations between IVUS parameters and FFR were assessed by Pearson correlation analysis.
Receiver operating characteristic (ROC) curve analysis was used to determine the best cut-off values (BCV) of the IVUS parameters predicting the functional significance of a lesion. Diagnostic accuracy including sensitivity, specificity, and positive and negative predictive values was calculated using best new cut-off values as well as the historical cut-off values of ≤4.0 mm2 and %PB >70%. Independent predictors for functional significance were identified by multivariate logistic regression analysis. All statistical analyses were performed using SPSS, Version 19.0.0 (IBM Corp., Armonk, NY, USA), and a p-value of <0.05 was considered statistically significant.
Results
BASELINE CHARACTERISTICS
Eight hundred and eighty-six patients (945 lesions) were enrolled in this pooled analysis from 11 centres, each with a different enrolment period ranging overall from 2004 to 2010. Among them, 64 patients (64 lesions) were excluded (incomplete clinical information, <18 years old, left ventricular ejection fraction <35%, or incomplete angiographic data). Data from 822 patients were finally included in this study. Data on a total of 881 lesions with 881 MLA and 701 %PB values were available.
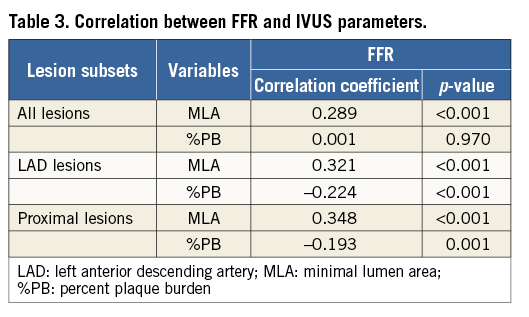
Patient baseline characteristics are presented in Table 1. Mean FFR value was 0.81±0.11. FFR was ≤0.80 in 353 lesions (40.1%). Mean MLA was 3.1±1.3 mm2. MLA was ≤4.0 mm2 in 689 lesions (78.2%). Mean %PB was 72.1±11.6%. The correlation between MLA and %PB was –0.594 (p<0.001). Functionally significant lesions were longer, more frequently located in the left anterior descending artery, and had smaller reference vessel diameter and minimal lumen diameter, higher percent diameter stenosis, and smaller MLA (Table 2). In analysis of the relationship between IVUS parameters and FFR, MLA showed a statistically significant but very weak correlation (r=0.289, p<0.001), and there was no correlation between %PB and FFR (r=0.001, p=0.970) (Figure 1). For LAD lesions, the correlation between MLA and FFR value was 0.321 (p<0.001) and that between %PB and FFR value was –0.224 (p<0.001). Similarly, in proximal lesions, the correlation with FFR was 0.348 for MLA (p<0.001) and -0.193 for %PB (p=0.001) (Table 3).
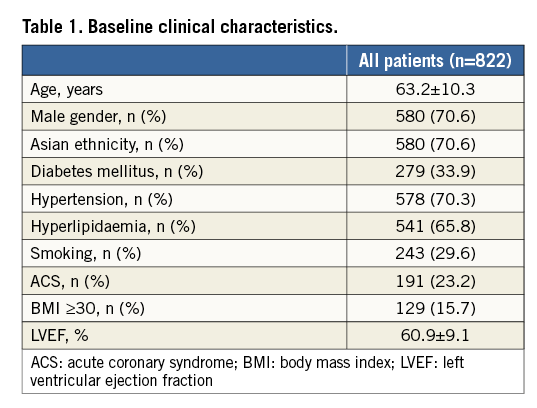
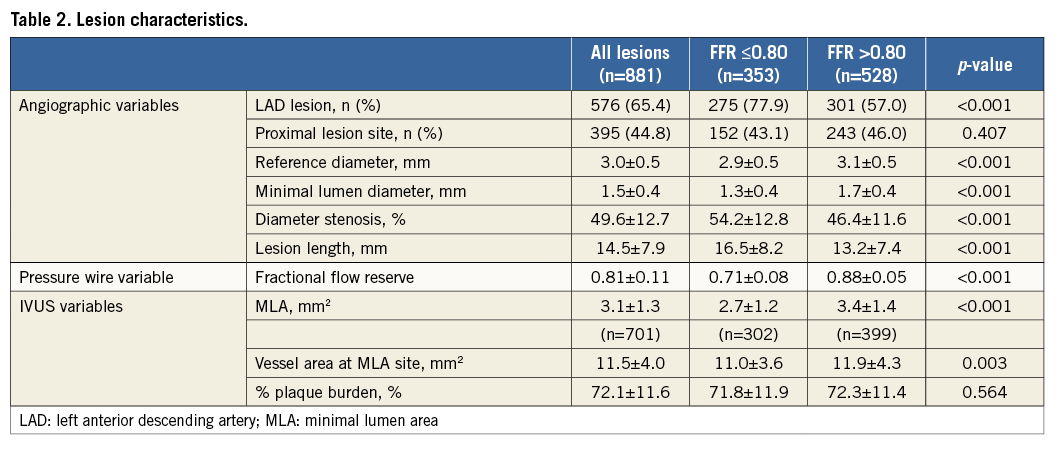
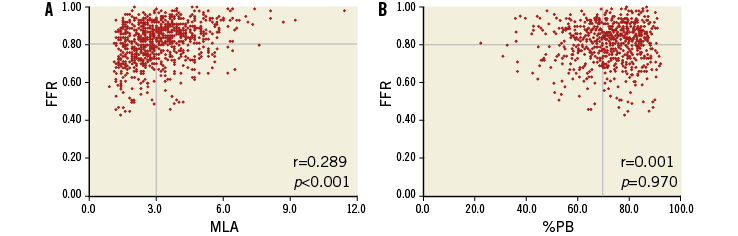
Figure 1. Relationship between FFR and IVUS MLA/%PB. There was a positive correlation between IVUS MLA and FFR (r=0.289, p<0.0001) and no correlation between IVUS %PB and FFR (r=0.001, p=0.970).
HISTORICAL IVUS CUT-OFF VALUES TO PREDICT FUNCTIONAL SIGNIFICANCE
Three hundred and two (43.8%) out of 689 lesions with MLA ≤4.0 mm2 and 185 lesions (42.2%) out of 438 lesions with %PB >70% had functionally significant stenosis. Three hundred and fifty-four lesions (50.5%) satisfied the combined cut-off values of MLA ≤4.0 mm2 and %PB >70% (Figure 2). Diagnostic performance of historical cut-off values of IVUS is shown in Figure 3.
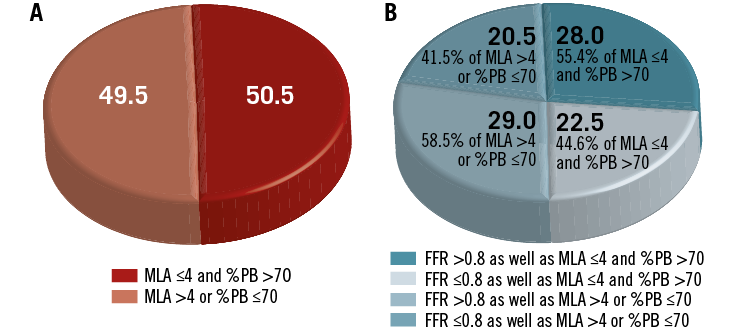
Figure 2. Historical IVUS cut-off. Distribution of study population according to: A) historical IVUS cut-off, and B) combination of IVUS and FFR cut-off. Among lesions with MLA ≤4.0 mm2 and %PB >70%, only 44.6% had FFR ≤0.80.
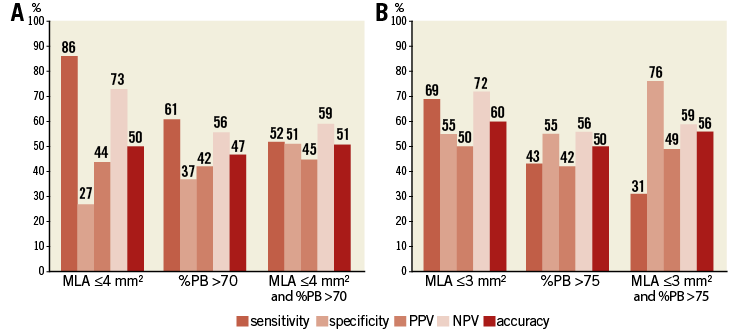
Figure 3. Diagnostic accuracy of IVUS criteria. Diagnostic accuracy according to historical (A) and new (B) IVUS criteria. Adaptation of new IVUS criteria improved specificity but decreased sensitivity. Consequently, accuracy did not vary much from that of historical IVUS criteria.
The area under the curve (AUC) of MLA ≤4.0 mm2 to define functional significance was 0.561 (95% confidence interval [CI]: 0.528-0.594) and that of %PB >70% was 0.511 (95% CI: 0.473-0.548). The AUC of combined IVUS criteria was 0.516 (95% CI: 0.478-0.554). When the ROC curves were compared, there were no significant differences between MLA ≤4.0 mm2, %PB >70% and both (p=0.285 between MLA and %PB; p=0.217 between MLA and both; and p=0.716 between %PB and both).
RENEWED IVUS BEST CUT-OFF VALUES TO PREDICT FUNCTIONAL SIGNIFICANCE
BCV of IVUS MLA to predict the presence of functional significance (FFR ≤0.8) in this pooled analysis was 3.0 mm2 (AUC 0.646, 95% CI: 0.609-0.684) and that of %PB was 75% (AUC 0.523, 95% CI: 0.479-0.567) (Figure 4).
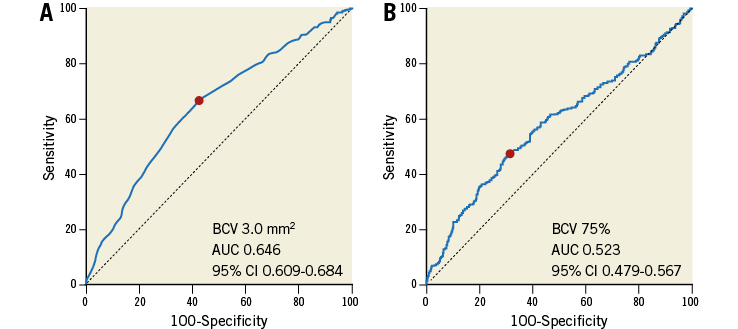
Figure 4. Receiver-operating characteristic curves for new IVUS criteria to predict FFR ≤0.80.
Two hundred and forty-three lesions (50.4%) among 482 lesions with MLA ≤3.0 mm2, and 129 lesions (41.9%) among 308 lesions with %PB >75% showed functional significance; 187 lesions (26.7%) fulfilled the combined MLA ≤3.0 mm2 and %PB >75% (Figure 5). Diagnostic performance of new BCVs for individual and combined IVUS parameters is shown in Figure 3.
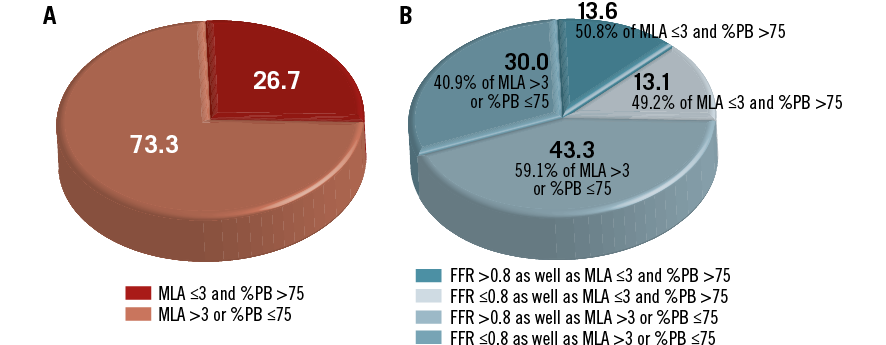
Figure 5. New IVUS cut-off. Distribution of study population according to: A) new IVUS cut-off, and B) combination of new IVUS and FFR cut-off. Among lesions with MLA ≤3.0 mm2 and %PB >75%, only 49.2% had FFR ≤0.80.
In ROC curve comparisons, new MLA BCV ≤3.0 mm2 (AUC 0.618, 95% CI: 0.585-0.650) had higher predictive power than new %PB BCV >75% (AUC 0.511, 95% CI: 0.473-0.548) or combined criteria (AUC 0.533, 95% CI: 0.496-0.571). However, %PB cut-off was not superior to combined criteria (p=0.0045 between MLA and %PB; p=0.0045 between MLA and both; and p=0.196 between %PB and both).
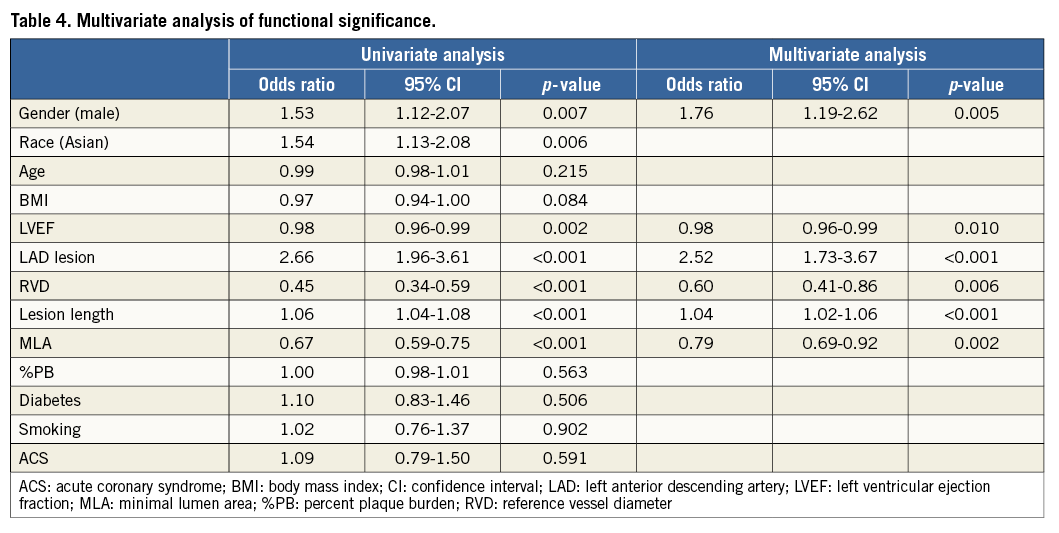
DETERMINANTS OF FUNCTIONAL SIGNIFICANCE
Univariate analysis of predictors of functional significance is shown in Table 4. Male gender, Asian race, left anterior descending artery (LAD) lesion and lesion length showed positive correlation with functional significance, while left ventricular ejection fraction (LVEF), reference vessel diameter (RVD) and MLA had negative correlation. Multivariate analysis showed the independent predictors of functional significance were male gender (odds ratio [OR] 1.76, 95% CI: 1.19-2.62), LVEF (OR 0.98, 95% CI: 0.96-0.99), LAD lesion (OR 2.52, 95% CI: 1.73-3.67), RVD (OR 0.60, 95% CI: 0.41-0.86), lesion length (OR 1.04, 95% CI: 1.02-1.06) and MLA (OR 0.79, 95% CI: 0.69-0.92).
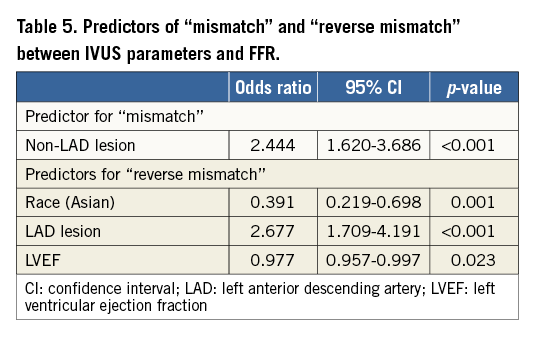
FACTORS TO PREDICT FUNCTIONAL AND ANATOMICAL MISMATCH
In terms of diagnostic accuracy of new BCV, incidence of false positive (mismatch) lesion, i.e., MLA ≤3.0 mm2 and %PB >75% and FFR >0.80, was 17.0%, in association with non-LAD lesion (OR 2.444, 95% CI: 1.620-3.686, p<0.001). For false negative lesion (reverse mismatch), i.e., MLA >3.0 mm2 or %PB ≤75% and FFR ≤0.80, the incidence was 24.4% in association with race (OR 0.391, 95% CI: 0.219-0.698, p=0.001 in the case of Asians), LAD lesion (OR 2.677, 95% CI: 1.709-4.191, p<0.001) and LVEF (OR 0.977, 95% CI: 0.957-0.997, p=0.023) (Table 5).
Discussion
The major findings of this large international multicentre pooled analysis were: 1) addition of %PB to MLA did not improve diagnostic performance of IVUS criteria to predict the functional significance of coronary lesions; 2) anatomical and functional mismatch occurred frequently; and 3) the predictors of mismatch were race, LAD lesion and LVEF.
IVUS CUT-OFF VALUES TO DEFINE FUNCTIONAL SIGNIFICANCE
Based on the study by Abizaid et al19, MLA ≤4.0 mm2 has been accepted as the standard cut-off to determine functional significance. However, several recent studies have proposed different ischaemic thresholds of MLA between 2.0 mm2 and 3.1 mm2 according to vessel size or lesion location5,7,13,20. The current large international multicentre study showed that ischaemia-predictable MLA is smaller than the historical value, and varies according to anatomical factors and the amount of myocardium supplied by the target segment.
In contrast to MLA, %PB reflects difference in vessel size (or amount of myocardium) and has been utilised to improve the accuracy of functional significance prediction21. However, the benefit of %PB to define the functional significance of coronary stenosis has been inconsistent in previous studies. Waksman et al found that %PB was not an independent predictor for identifying FFR <0.8 (OR 1.03, 95% CI: 0.99-1.06, p=0.110)22. Likewise, when Yang et al evaluated the relationship between various IVUS parameters and FFR, %PB was not an independent predictor23. In our study, the accuracy of %PB >70% alone to predict functional significance was similar to that of MLA ≤4.0 mm2. Moreover, there was inferiority in newly determined %PB BCV of >75% compared with new MLA BCV of ≤3.0 mm2. Although the diagnostic accuracy of %PB to predict functional significance could be lower than that of other anatomical parameters, %PB as a prognostic factor should not be undervalued as validated in a recent study24.
Because the accuracy of individual IVUS values was challenged, that of their combination was evaluated. Briguori et al (43 patients, 53 lesions) found that the combined use of MLA ≤4.0 mm2 and %PB >70% greatly improved specificity compared to the MLA criterion alone21. However, these criteria are no longer valid because MLA cut-off value varies according to lesion conditions. Although Chen SL et al suggested different cut-off values of MLA and %PB to predict functional significance according to clinical presentation, vessel size and lesion location, the combination of MLA and %PB increased the diagnostic value only for LAD lesion12. Similar results were obtained in our study. Although the correlation between FFR and IVUS variables was poor, its value improved after lesion was subdivided into only LAD lesion or proximal lesion. The correlation between MLA and FFR value was 0.321 (p<0.001), and that between %PB and FFR value was –0.224 (p<0.001) when only LAD lesion was selected. Similarly, the correlation in proximal lesion was 0.348 in MLA (p<0.001) and –0.193 in %PB (p=0.001). Therefore, the accuracy of anatomical lesion assessment to predict functional significance can be affected by the affected myocardium.
The combination of IVUS criteria in the present study also failed to increase diagnostic accuracy in predicting functional significance, for which there might be several explanations. First, as discussed above, %PB might have a lower diagnostic value than MLA. Second, although %PB increased, positive remodelling of a vessel can compensate for luminal loss during early atherosclerosis, thereby affecting the correlation between MLA and %PB with FFR. Third, contingent upon its definition, %PB can be affected by change in vessel area evoked by spasm or stretch during IVUS examination. Fourth, the use of combined criteria improved specificity but decreased sensitivity because of a higher possibility of false negatives. Consequently, there was almost no change in diagnostic accuracy.
FACTORS ASSOCIATED WITH FFR VALUE
The current study suggested that gender affects functional severity. Compared with females, males generally have higher body mass index and larger coronary arteries which might account for the gender difference seen. A similar explanation can be used for the observed effect of race. Because lower LVEF is associated with higher left ventricular end-diastolic pressure (LVEDP), and in turn LVEDP is positively associated with FFR, LVEF has a negative correlation with functional significance24. LAD also influenced functional significance. This could be explained by the larger extent of myocardium supplied by LAD compared to non-LAD arteries9. Larger reference vessel diameter is also related to a greater extent of affected myocardium, and therefore functional severity varies with vessel diameter22. Not surprisingly, lesion length and MLA affect lesion severity. Iguchi et al (165 patients, 199 lesions) suggested that lesion length >16 mm was the BCV to predict functional significance for intermediate lesions (AUC: 0.940)25.
The variety of factors which affect coronary physiology renders it more difficult to pinpoint anatomical parameters to predict physiology. Even with the most widely used historical parameters, a single anatomical value could not appropriately reflect specific physiologic conditions (different resting flow, myocardial bed size, and achievable hyperaemic flow capacity, among others) in individual patients. Each imaging modality is limited by its own resolution on a geometric measurement, which in turn limits the usefulness of such measurement.
Limitations
First, this is a pooled analysis which has the possibility of selection bias. Second, various hyperaemic methods were used with different hyperaemic agents, routes of administration and dosages. However, the efficacy of all hyperaemic methods has previously been validated in several studies. Third, IVUS and QCA analysis was performed at each centre without common core lab analysis; however, data were obtained from skilled and validated analysts. Fourth, although the FFR cut-off value to define functional significance is a continuum spanning from 0.75 to 0.80, we decided to use the upper limit as was done in the FAME study. Therefore, the IVUS cut-off value would change if FFR <0.75 was defined as standard. Fifth, FFR analysis was performed based on cross-sectional information without pullback evaluation. Although serial stenosis was excluded in this study, mild plaque beyond the lesion of interest might affect FFR value.
Conclusion
Because of the various factors that affect FFR, IVUS parameters such as MLA and %PB, either alone or in combination and at different thresholds, have limited ability to predict functional significance in intermediate coronary artery stenosis. This limitation of IVUS should always be taken into account in clinical decision making. Therefore, it is no longer reasonable to use IVUS alone to inform decisions on stent implantation. When evaluating the relationship between functional and anatomical parameters, more careful consideration is warranted to avoid frequent mismatch between FFR and IVUS.
| Impact on daily practice Although IVUS can provide various anatomical information on coronary artery disease, inherent limitations to define the functional significance of coronary artery stenosis need to be taken into account in clinical decision making. Our study showed that the addition of percent plaque burden to minimal lumen area did not improve diagnostic performance of IVUS to predict the functional significance of coronary stenosis. False positive results (IVUS+, FFR–) were more common in non-LAD lesions and false negative results (IVUS–, FFR+) were more common in LAD lesions, Westerners and low left ventricular ejection fraction. |
Funding
This study was supported by a 2012 grant from the Scholar Research Grant of Keimyung University and a 2013 research grant from Myung-In Pharmaceutical Company.
Conflict of interest statement
The authors have no conflicts of interest to declare.