Abstract
Background: Contemporary chronic total occlusion (CTO) percutaneous coronary intervention (PCI) incorporates wire escalation and dissection/re-entry recanalisation strategies.
Aims: The purpose of the study was to investigate changes in collateral function after CTO PCI and to identify whether the mode of successful recanalisation influences collateral function regression.
Methods: Patients scheduled for elective CTO PCI with evidence of viability in the CTO territory by noninvasive imaging were included in this study. After successful CTO PCI, the aortic pressure (Pa) and distal coronary artery wedge pressure (Pw) during balloon occlusion were measured, both in a resting state and during infusion of intravenous adenosine, allowing the calculation of the pressure-derived collateral pressure index at rest and hyperaemia (CPIrest and the collateral fractional flow reserve [FFRcoll], respectively). Measurements were repeated 3 months later during angiographic follow-up.
Results: Eighty-one patients had physiological measurements at baseline and follow-up. In the final cohort the mean age was 64 years and 82% were male. The mean maximal stent diameter and total stent length were 3.2±0.5 mm and 68±31 mm, respectively. Successful strategies were antegrade wiring (64.2%), antegrade dissection re-entry (8.6%), and retrograde dissection re-entry (27.1%). Between the index procedure and follow-up, wedge pressure decreased from 34±11 mmHg to 21±8.5 mmHg (p<0.01), respectively. FFRcoll changed from 0.34±0.11 to 0.19±0.09 (p<0.01) at follow-up and CPIrest from 0.40±0.14 to 0.17±0.09 (p<0.01). Absolute maximum collateral flow decreased from 55±32 ml/min directly after PCI to 38±24 ml/min (p<0.01). There was no relation between the recanalisation technique and changes in FFRcoll.
Conclusions: There was a significant reduction in collateral flow over time, independent of the recanalisation technique.
Introduction
Percutaneous coronary intervention (PCI) for chronic total occlusions (CTO) has expanded remarkably during the last decades. Nowadays it is accepted to perform such procedures in symptomatic patients with viable myocardium. The hybrid algorithm has incorporated wire-escalation and dissection/re-entry recanalisation strategies (antegrade or retrograde) as planned steps of the procedure. Using these methods, success rates higher than 90% are common in experienced centres whilst complication rates are low1. Nevertheless, CTO PCI remains complex and target lesion failure (TLF) is still high compared to non-CTO PCI2. TLF post-CTO PCI is multifactorial and includes patient-, lesion- and procedure-related factors. A comprehensive assessment of pathophysiological changes in the coronary circulation after CTO PCI enables better understanding of the underlying mechanisms3. These pathophysiological changes can be classified as follows: 1) effects on the CTO vessel itself and its dependent myocardium, 2) effects on the donor vessel and 3) effects on the interaction between the two, i.e., the collateral circulation3. Older and recent studies have demonstrated that after successful CTO PCI, blood flow and microvascular function do not normalise immediately but improve significantly over time45. This is reflected by an increase in absolute blood flow (Q) and fractional flow reserve (FFR) of the CTO artery and a decrease in microvascular resistance (R) of the dependent myocardium6. These physiological changes are accompanied by a reduction in blood flow in the collateral vessels and further collateral regression over time789. In the donor artery, an increase in FFR with a decrease of flow and an increase in resistance has been observed; this has been attributed to decreased collateral function91011.
Following contemporary CTO PCI, the collateral circulation has been studied in small groups of patients, but the relationship between current CTO recanalisation techniques and changes in collateral function directly post-PCI and at follow-up have not been investigated. The aim of this study was to investigate changes in collateral flow after contemporary CTO PCI and to identify whether the mode of successful recanalisation influences changes in collateral function.
Methods
Study design and population
This prospective observational study was performed in patients undergoing elective CTO PCI in one of the participating hospitals (The Essex Cardiothoracic Centre, United Kingdom; Royal Sussex County Hospital, United Kingdom; Catharina Hospital Eindhoven, the Netherlands) between February 2019 and November 2020. All patients had evidence of viability in the CTO territory, confirmed by noninvasive imaging viability assessment (i.e., cardiac magnetic resonance [CMR] or myocardial perfusion imaging [MIBI]) or preserved left ventricular wall motion at rest. In all cases angiographically visible collateral vessels were present. Patients unable to receive antiplatelets, with known severe kidney disease, or who were pregnant were excluded. The study was approved by the local ethics committees and adhered to the principles of the Declaration of Helsinki. All subjects gave written informed consent prior to participating in the study.
Chronic total occlusion percutaneous coronary intervention
CTO PCI was performed according to international guidelines and local practice. All patients were on dual antiplatelet therapy prior to the procedure. Any attempted recanalisation was at the operator’s discretion. All contemporary crossing techniques were used: antegrade wire escalation, antegrade dissection and re-entry, retrograde wire escalation and retrograde dissection and re-entry. A procedure was considered successful when TIMI flow grade 3 was achieved with <30% angiographic residual stenosis in the CTO vessel. All patients received drug-eluting stents. Patients were discharged on dual antiplatelet therapy with a duration of at least 6 months.
Collateral fractional flow reserve and coronary wedge pressure assessment
Immediately after successful CTO PCI, coronary physiology indices were measured. A guidewire equipped with a pressure and temperature sensor (PressureWire X; Abbott) was introduced into the revascularised vessel and, after equalisation of pressures and administration of nitrates, advanced to the distal vessel. To adequately assess wedge pressure, the pressure wire was positioned in the distal coronary artery. Then, a balloon was advanced over the pressure wire and placed into the stent at the location of the previous occlusion. Next, the balloon was inflated at low pressures to occlude the vessel. The wedge pressure was assessed during rest and hyperaemia using intravenous (IV) adenosine. Immediately after acquisition of the wedge pressure, the balloon was deflated and anterograde blood flow was restored.
FFR as represented by hyperaemic Pd/Pa (distal coronary pressure/aortic pressure) reflects the influence of a coronary stenosis on the maximum achievable myocardial blood flow. Myocardial blood flow is the sum of coronary artery blood flow and collateral blood flow. Collateral flow is negligible in patients without significant stenosis, but collateral flow becomes important in stenotic arteries and CTO. The distribution of maximum blood flow in the underlying myocardium, the supplying coronary artery, and the collateral is described by FFRmyo=FFRcor+FFRcoll3. The 3 FFR components can be assessed separately by regular pressure measurements if measurement of the coronary wedge pressure during balloon occlusion is also performed12. In this way, the maximum achievable collateral blood flow in the dependent myocardium is expressed as a percentage (or fraction) of the total normal maximum myocardial blood flow.
FFRcoll was calculated as FFRcoll=(Pw−Pv)/(Pa−Pv) during maximum hyperaemia as described before (Pw=wedge pressure and Pv=central venous pressure)12. For Pv the default value of 5 mmHg was used13. FFRcoll has also been called pressure-derived collateral flow index at hyperaemia14. The epicardial component of FFR (i.e., FFRcor) can be calculated according to the equation FFRcor=(Pd−Pw)/(Pa−Pw)12. Resting collateral flow was estimated by (Pw−Pv)/(Pa−Pv) at rest and is described in the manuscript as resting pressure-derived collateral pressure index (CPIrest). The difference between (Pw−Pv)/(Pa−Pv) at rest and at hyperaemia has been suggested as a measure of coronary steal15.
Absolute flow and resistance measurements
Alongside FFRcoll and Pw, measurements of absolute blood flow were also performed using continuous thermodilution. This method has been previously described16. In short, a multifunctional monorail infusion catheter (RayFlow; Hexacath) is advanced over the dedicated pressure and temperature guidewire and placed in the proximal coronary artery. The catheter is connected to an infusion pump, and saline infusion at a prespecified flow rate (Qi) is started. The distal temperature (T) of the saline/blood mixture is recorded automatically by the guidewire sensor. The saline infusion itself creates a state of maximum hyperaemia within seconds17. When a steady hyperaemic state is achieved, the guidewire is pulled back to the tip of the catheter and the temperature of the infused saline (Ti) is measured. The absolute coronary flow during steady state maximum hyperaemia (Q in ml/min) is calculated by assessment of the changes in the distal coronary temperature (T) compared to the infusion temperature of the saline (Ti) by the equation Q=1.08 Ti/T×Qi. Instantaneous wireless recording and analysis of coronary pressure traces and temperature are performed, and automated calculations of Q and R are carried out using a dedicated software system (CoroFlow; Coroventis). Because FFR as well as absolute coronary blood flow are known, the maximum recruitable collateral flow can also be calculated in ml/min by the equation Qcoll=Q × FFRcoll/FFRcor (Supplementary Appendix 1).
Follow-up procedure
After 3 months, patients were scheduled for a follow-up catheterisation with measurements of physiologic parameters in the previously stented, recanalised CTO vessel. The Central Illustration shows an example of the complete measurements at the index procedure and at 3-month follow-up.
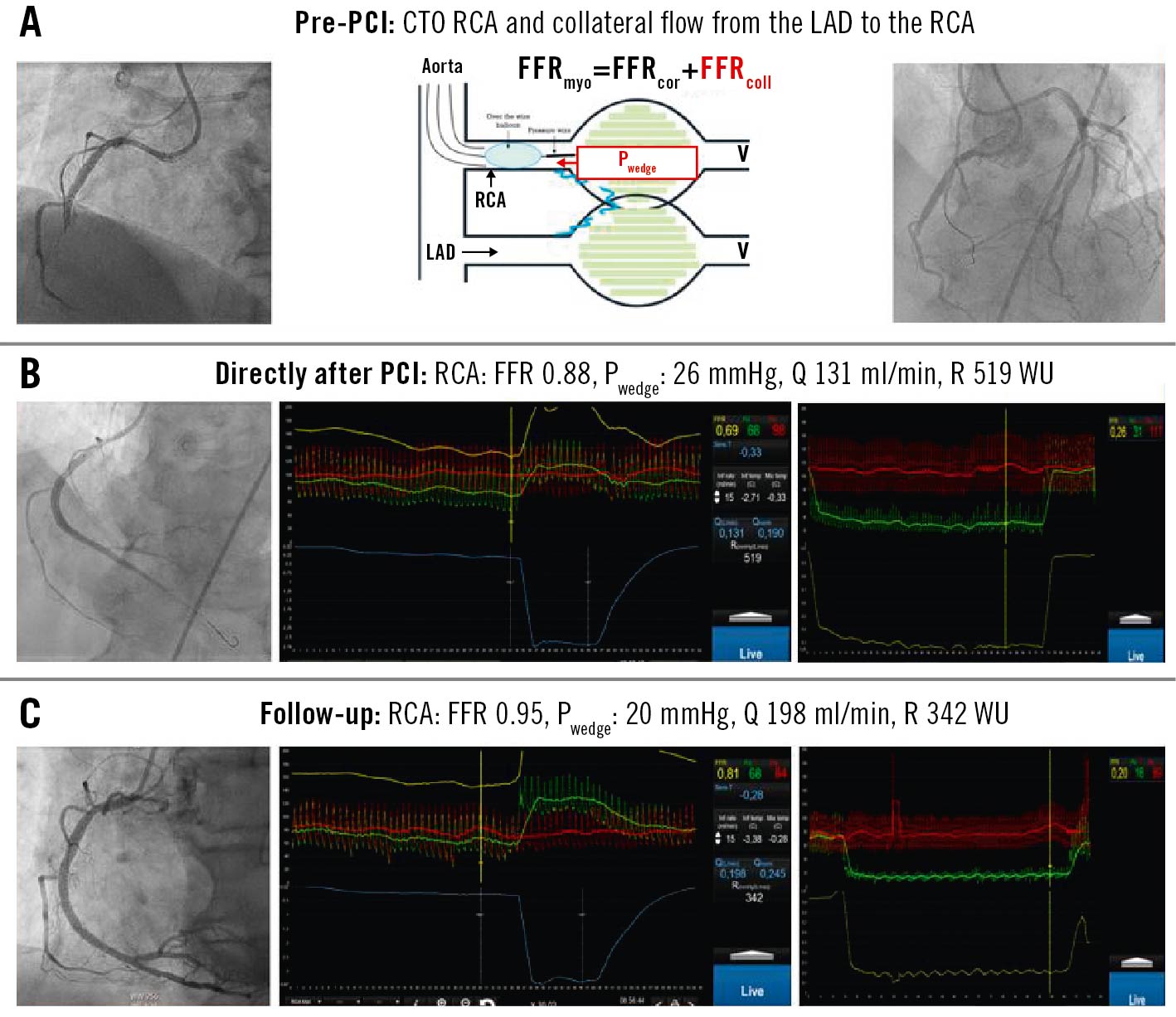
Central Illustration. Example of the complete measurements at the index procedure and at 3-month follow-up. A) In panel A (left) the angiographic image from the chronic occluded RCA is shown. The right panel shows collaterals from the LAD to the RCA. An overview of this situation is drawn in the middle image. B) Panel B shows the angiogram (left panel) and physiologic measurements directly after PCI of the RCA (middle panel). FFR equals 0.88 and the absolute flow is 131 ml/min with a microvascular resistance of 519 WU. In the right panel the wedge pressure is shown, indicating a wedge pressure of 26 mmHg and an FFRcoll of 0.23. In the right panel the donor vessels from the LAD are visualised. C) Panel C shows the angiogram at follow-up after 3 months. In the left panel the positive remodelling of the RCA can be observed. The middle panel shows an FFR of 0.95, absolute flow of 198 ml/min and microvascular resistance of 342 WU. In the right panel the wedge pressure is shown, indicating a decreased wedge pressure of 20 mmHg and FFRcoll of 0.15. CTO: chronic total occlusion; FFRcoll: fractional flow reserve collateral; FFRcor: fractional flow reserve coronary artery; FFRmyo: fractional flow reserve myocardium; LAD: left anterior descending; PCI: percutaneous coronary intervention; Pwedge: wedge pressure; Q: absolute blood flow; R: microvascular resistance; RCA: right coronary artery; WU: Wood units
Statistical analysis
Categorical variables are presented as absolute numbers and percentages. Continuous variables are presented as mean±standard deviation or median and interquartile range as appropriate. Data were checked for normality of distribution using the Kolmogorov–Smirnov test. Comparisons of the relative change in coronary wedge pressure, or FFRcoll at baseline versus follow-up, were made using a paired t-test in case of normal distribution and Wilcoxon Rank test in case of non-normal distribution. Multivariate regression analysis was performed to determine predictors for changes in wedge pressure, FFRcoll and Qcoll. A 2-tailed level of significance of 0.05 was used. All preceding analyses were performed using SPSS Statistics 25.0 (IBM).
Results
Baseline characteristics and procedural results
A total of 119 patients having elective CTO PCI were recruited, and 106 had a successful procedure (procedural success rate 89%). Of these, 92 underwent the research protocol at the end of the PCI, and 14 patients were excluded due to the following reasons: time constraints (n=8), unfavourable anatomy for pressure wire passage distal to the stented segment (n=4) and balloon angioplasty without stent placement (n=2). A final cohort of 81 patients had physiological measurements at baseline and follow-up. The mean subjects’ age was 64 years, and 82% were male (Table 1). The mean follow-up was 84±35 days. The mean Japanese-CTO (J-CTO) score was 2, and the EURO-CASTLE score was ≥3 in 22% of patients (Table 2). The final successful strategies were antegrade wiring (64.2%), antegrade dissection re-entry (8.6%), and retrograde (27.1%). The mean maximal stent diameter and total stent length were 3.2±0.5 mm and 68±31 mm, respectively. Three patients experienced atrioventricular (AV) block during the research procedure (absolute flow measurement) with quick recovery.
Table 1. Baseline characteristics.
| Baseline characteristics | N (%) or mean±SD | |
|---|---|---|
| Age (years) | 64±9.3 | |
| Sex, male | 66 (81.5) | |
| BMI (kg/m2) | 29.1±4.5 | |
| CCS class | CCS I | 18 (22.2) |
| CCS II | 37 (45.7) | |
| CCS III | 23 (28.4) | |
| CCS IV | 3 (3.7) | |
| NHYA Class (I/II/III) | NYHA I | 35 (43.2) |
| NYHA II | 27 (33.3) | |
| NYHA III | 19 (23.5) | |
| Viability test | LVgram | 3 (3.7) |
| Echo | 26 (32) | |
| MRI | 44 (54.3) | |
| MIBI | 8 (9.9) | |
| LVEF (%) | 54±10 | |
| Risk factors | ||
| Diabetes | 16 (19.8) | |
| Hypertension | 57 (70.4) | |
| Cholesterol | 71 (87.7) | |
| Current smoker | 12 (14.8) | |
| Ex-smoker | 35 (43.2) | |
| Previous myocardial infarction | 41 (50.6) | |
| Previous PCI | 33 (40.7) | |
| Previous CABG | 12 (14.8) | |
| Chronic kidney disease | 3 (3.7) | |
| Previous TIA or CVA | 4 (4.9) | |
| Medication | ||
| Aspirin | 70 (86.4) | |
| Antiplatelets | 70 (86.4) | |
| Beta-blocking agents | 59 (72.8) | |
| RAAS-inhibitor | 47 (58) | |
| Statin | 60 (74.1) | |
| Nitrates | 34 (42) | |
| BMI: body mass index; CABG: coronary artery bypass graft; CCS: Canadian Cardiovascular Society; CVA: cerebrovascular accident; LVEF: left ventricular ejection fraction; LVgram: left ventriculogram; MIBI: myocardial perfusion imaging; MRI: magnetic resonance imaging; NHYA: New York Heart Association; PCI: percutaneous coronary intervention; RAAS: renin angiotensin aldosteron system; SD: standard deviation; TIA: transient ischaemic attack | ||
Table 2. Procedural characteristics.
| Baseline angiographic data | Number (%) or mean±SD |
|
|---|---|---|
| Dominance | Right | 76 (93.8) |
| Left | 4 (4.9) | |
| Codominance | 1 (1.2) | |
| CTO vessel (RCA/LAD/LCx) | RCA | 53 (65.4) |
| LAD | 20 (24.7) | |
| LCx | 8 (9.9) | |
| Donor vessel | RCA | 20 (24.7) |
| LAD | 50 (61.7) | |
| LCx | 8 (9.9) | |
| LM/SVG | 1 (1.2) /2 (2.4) | |
| Rentrop grade | I | 3 (37) |
| II | 25 (30.9) | |
| III | 52 (64.2) | |
| Collateral connection grade | I | 48 (59.3) |
| II | 20 (24.7) | |
| III | 13 (16) | |
| J-CTO score | 2±1.3 | |
| CASTLE score | 1.6±1.3 | |
| CTO PCI procedure | ||
| 1st Access site | Left radial artery | 1 (1.2) |
| Left femoral artery | 0 (0) | |
| Right radial artery | 14 (17.3) | |
| Right femoral artery | 66 (81.5) | |
| 2nd Access site | Left radial artery | 5 (6.1) |
| Left femoral artery | 5 (6.1) | |
| Right radial artery | 53 (65.4) | |
| Right femoral artery | 18 (22.2) | |
| Wiring time (min) | 52.5±45.1 | |
| Final strategy | AWE | 52 (64.2) |
| RWE | 2 (2.4) | |
| ADR | 7 (8.6) | |
| RDR | 20 (24.7) | |
| Number of stents | 2±0.9 | |
| Number of stents | I | 24 (29.6) |
| II | 32 (39.5) | |
| III | 20 (24.7) | |
| VI | 5 (6.1) | |
| Total stent length (mm) | 68.4±30.3 | |
| Maximal stent diameter (mm) | 3.2±0.5 | |
| ADR: antegrade dissection re-entry; AWE: antegrade wire escalation; CTO: chronic total occlusion; J-CTO; Japanese chronic total occlusion; LAD: left descending anterior; LCx: left circumflex; LM: left main; PCI: percutaneous coronary intervention; RCA: right coronary artery; RDR: retrograde dissection re-entry; RWE: retrograde wire escalation; SD: standard deviation; SVG: saphenous vein graft | ||
Collateral fractional flow reserve and coronary wedge pressure measurement
Between CTO PCI and follow-up, coronary wedge pressure decreased from 34.4±11 mmHg to 21±8.5 mmHg (p<0.01) and FFRcoll changed from 0.34±0.11 to 0.19±0.09 (p<0.01) (Figure 1, Table 3) at follow-up. The resting value of (Pw−Pv)/(Pa−Pv)/CPIrest decreased from 0.40±0.14 to 0.17±0.09 (p<0.01).
At baseline, the absolute difference between rest and hyperaemic (Pw−Pv)/(Pa−Pv) measurements was 0.06±0.08 (0.40±0.14 vs 0.34±0.11; p<0.01). Sixty-three (78%) patients showed an absolute lower hyperaemic (i.e., FFRcoll) value (Figure 2). The higher value of the resting measurement indicates the presence of coronary steal at that moment. This argues indirectly for incomplete recovery of the microvasculature immediately post-PCI. At 3-month follow-up, such a difference between resting and hyperaemic measurements was not observed (0.17±0.09 vs 0.19±0.09; p=nonsignificant).
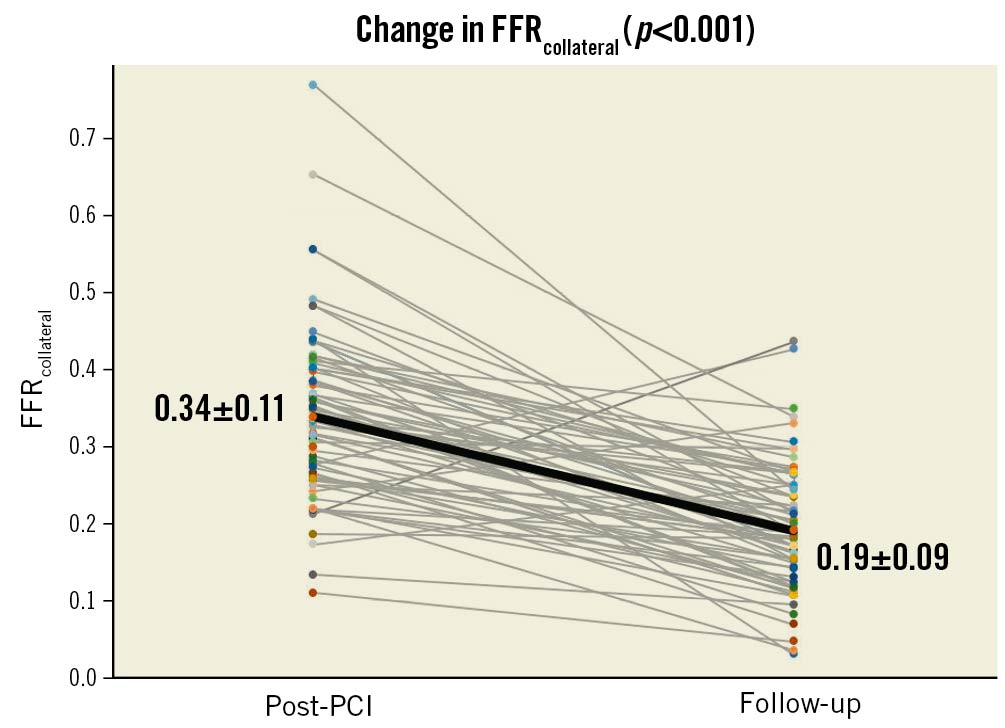
Figure 1. Change in collateral FFR between index procedure and 3-month follow-up. FFRcollateral indicates the percentage of normal maximum myocardial perfusion which is possible by collaterals. FFR: fractional flow reserve; PCI: percutaneous coronary intervention
Table 3. Physiologic measurements.
| Physiologic measurement | Immediately after index procedure | Follow-up | p-value |
|---|---|---|---|
| Pdrest during wedge | 41.1±13.5 | 20.1±9.7 | <0.01 |
| Parest during wedge | 95.5±14.1 | 92±13.6 | 0.28 |
| Pd/Parest during wedge | 0.44±0.13 | 0.21±0.09 | <0.01 |
| Pdhyperaemia during wedge | 34.4±11.3 | 21.5±8.5 | <0.01 |
| Pahyperaemia during wedge | 90.4±15 | 92.9±14.8 | <0.01 |
| Pd/Pahyperaemia during wedge | 0.38±0.11 | 0.23±0.09 | <0.01 |
| FFRcoll during occlusion | 0.34±0.11 | 0.19±0.09 | <0.01 |
| (Pw−Pv)/(Pa−Pv) at rest | 0.40±0.14 | 0.17±0.09 | <0.01 |
| FFRmyo | 0.86±0.11 | 0.88±0.08 | 0.06 |
| FFRcor | 0.76±0.17 | 0.84±0.1 | <0.01 |
| FFRcoll | 0.08±0.11 | 0.05±0.02 | <0.01 |
| Qmax | 210±87 | 255±99 | <0.01 |
| Qcor | 155±82 | 215±82 | <0.01 |
| Qcoll during occlusion (ml/min) | 55±32 | 38±24 | <0.01 |
| Qcoll (ml/min) | 14±10 | 7±5 | <0.01 |
| Values represent mean±SD. FFRcoll: fractional flow reserve collateral; FFRcor: fractional flow reserve coronary artery; FFRmyo: fractional flow reserve myocardium; Pa: aortic pressure; Pd: diastolic pressure; Pv: central venous pressure; Pw: wedge pressure. Qcoll during occlusion is the maximal recruitable blood flow over the collateral directly after PCI with an inflated balloon in the just-placed stent. Qcoll is the actual blood flow over the collateral directly after PCI in the open vessel. | |||
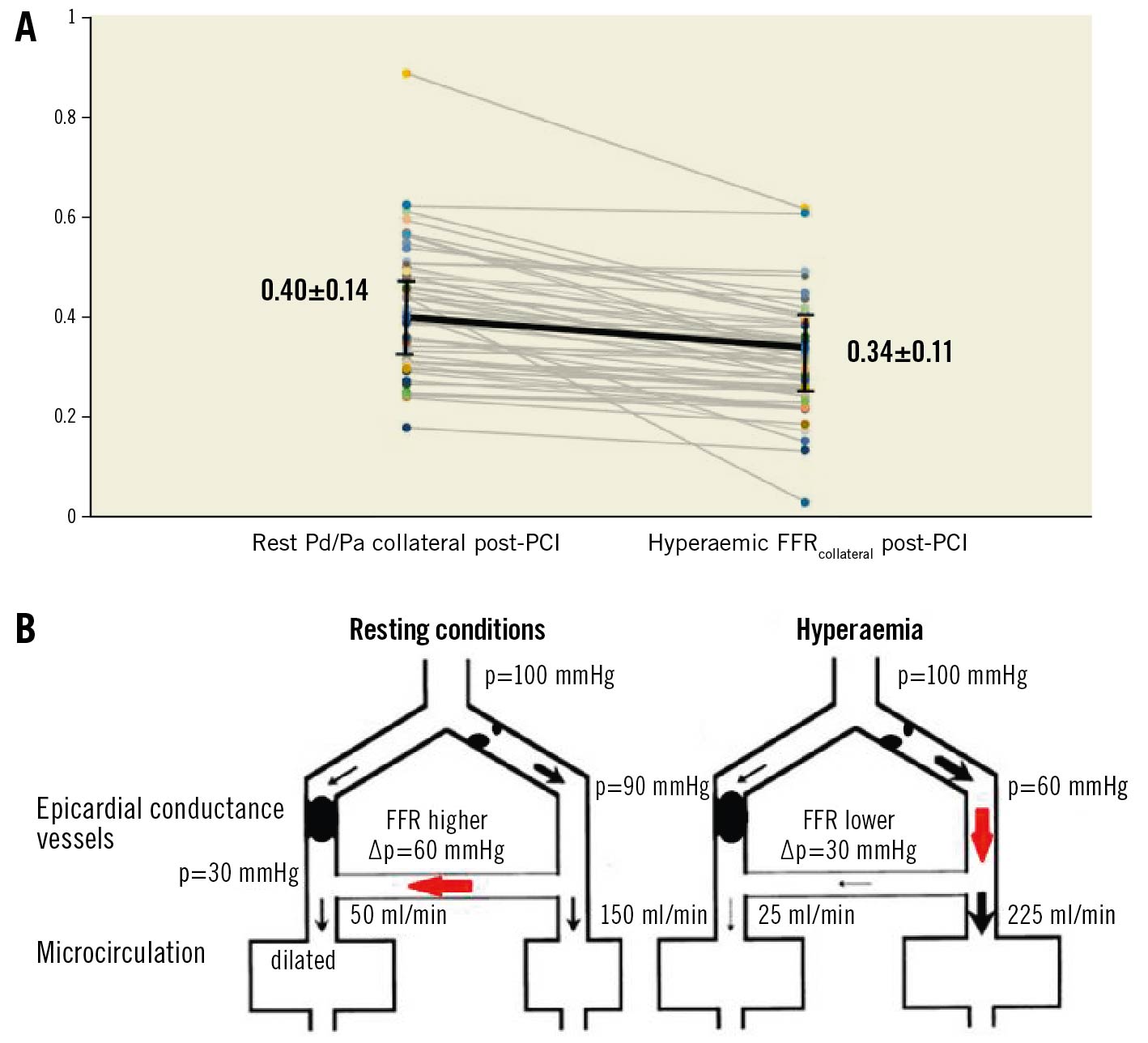
Figure 2. Coronary steal. A) Panel A demonstrates the difference between (Pw−Pv)/(Pa−Pv) at rest (directly after CTO PCI) and hyperaemic FFRcollateral. This difference is significant and indicates the presence of coronary steal. B) Panel B is a schematic explanation of how steal occurs. Under resting conditions the microcirculation from the myocardium distal to the CTO is already fully dilated. Blood supply is provided by the donor arteries. When hyperaemia is induced the microcirculation of the donor area dilates and flow to this territory increases. With a further decrease of blood flow to the (already) ischaemic CTO myocardium. CTO: chronic total occlusion; FFR: fractional flow reserve; PCI: percutaneous coronary intervention; Pd/Pa: distal coronary pressure/aortic pressure
Change in absolute collateral blood flow
Absolute collateral blood flow can be calculated using maximum coronary blood flow and the FFRcor and FFRcoll values during balloon occlusion (Supplementary Appendix 1). The maximum recruitable Qcoll decreased from 55±32 ml/min directly after PCI to 38±24 ml/min (p<0.01) at 3-month follow-up (Table 3). The actual Qcoll values in the open CTO artery decreased from 14±10 ml/min directly after PCI to 7±5.2 ml/min (p<0.01) at 3-month follow-up. Whereas total myocardial blood flow in the CTO territory had increased from 210±87 ml/min directly after PCI to 255±99 ml/min at follow-up (p<0.01).
Multivariate analysis for predictors of collateral function changes
Multivariate regression (unstandardised beta [95% confidence interval]) identified no independent predictors determining changes in FFRcoll. The J-CTO score, baseline angiographic collateral grades, total stent length, maximum stent diameter and recanalisation technique did not influence such changes.
Discussion
This study is the largest contemporary study to perform a complete physiological analysis of collateral function directly after modern CTO PCI and at follow-up.
The main findings of this study are:
- Wedge pressure and maximum recruitable collateral flow were significantly decreased at 3-month follow-up compared to immediately after the index procedure.
- Consequently, maximum absolute collateral blood flow was significantly decreased at 3-month follow-up.
- Methods of CTO recanalisation were not predictive of collateral function at 3-month follow-up.
- FFRcoll was significantly lower than CPIrest directly after PCI. This difference disappeared at follow-up, indicating the presence of coronary steal immediately after CTO PCI.
FFR and FFRcoll have been previously studied by Karamasis et al in patients undergoing contemporary CTO PCI. That study mainly focused on FFR changes after PCI and at follow-up but also analysed the 2 contributing components of FFR (FFRcor and FFRcoll). It showed a significant increase in FFR at follow-up with a decrease in collateral blood flow reflected by lower FFRcoll (0.29 after PCI compared to 0.18 at follow-up)6. The study included only patients with a right coronary artery (RCA) CTO and had a considerably small cohort size (n=26). The current study, which recruited all coronary arteries, showed a clear decrease in collateral flow at 3-month follow-up (34% of maximum achievable myocardial blood flow after PCI compared to 19% at follow-up). Twenty years ago, the seminal work by Werner et al18 showed similar results with collateral function regressing during long-term follow-up.
Five out of 81 patients in the current study showed an increase in FFRcoll at follow-up. Three of these patients had large epicardial collaterals that had not regressed. One patient had significant stenosis distal to the stented segment and in another one the distal stent landing zone involved the posterior descending artery/posterior left ventricular artery (PDA/PLV) bifurcation; a single-stent strategy was applied during the index procedure leaving the other branch with a significant ostial stenosis obvious at the follow-up angiogram. These patients underwent further optimisation. The above clinical and angiographic characteristics might explain the persistently high FFRcoll in those patients.
A novel feature of the present study is that not only FFR and its constituent components (FFRcoll and FFRcor) were measured, but also absolute coronary blood flow by continuous thermodilution. Therefore, collateral blood flow could be expressed as an absolute value in ml/min. Previous studies on collateral donor physiology have used average peak blood velocity, measured with intracoronary Doppler, and proximal vessel diameter to calculate absolute blood flow11. Although such a measurement is a quantitative estimate, it is less reliable and subject to several limitations, e.g., the exact position of the measurement. It has been shown previously that absolute coronary blood flow further increases during the 3 months after CTO PCI, accompanied by a decrease in resistance in the coronary microcirculation5. Those observations have now been extended to include a decrease in absolute collateral flow. The fact that it takes some time for the post-CTO PCI distal coronary artery and myocardium to recover explains why recruitable collateral flow also remains rather high for an interval.
Another interesting finding was that hyperaemic FFRcoll was significantly lower than the CPIrest in most of the patients (Figure 2A), indicating a degree of coronary steal of about 15% of recruitable blood flow immediately after CTO PCI. At follow-up this difference was absent. Coronary steal is a phenomenon that appears when vasodilatory reserve is limited (Figure 2B). This is certainly the case in chronic total occlusions15. The whole mechanism of steal is based on the redistribution of blood flow under hyperaemia from the donor vessel to the collateral circulation. Coronary steal occurs when the microcirculation distal to a stenosis in the donor vessel dilates with a subsequent pressure drop in the distal donor artery. Thereby, perfusion pressure across the already maximally dilated collateral bed decreases as does collateral blood flow. This is reflected by a higher value of (Pw−Pv)/(Pa−Pv) at rest compared to hyperaemia. Patients often present with angina pectoris when a stenosis in the donor vessel becomes severe enough to create steal to a level where symptoms occur with minimal physical exercise. Of note, we did not measure (Pw−Pv)/(Pa−Pv) before CTO PCI, which is feasible by exchanging the CTO guidewire when in the true lumen for a pressure wire through a microcatheter. These measurements could have revealed much more pronounced steal before the PCI. The number of patients with steal in our study is higher than the 33% reported by Werner et al1518 15 years ago. Here, collateral flow was assessed using a Doppler wire, which has its own intrinsic technical limitations, in particular for assessing collateral flow19.
Finally, we investigated independent predictors of collateral function changes over time. We were mainly interested in exploring whether specific crossing methods would affect physiological outcomes, considering that dissection/re-entry techniques create a degree of vessel injury. Comparing angiographic, imaging, functional and clinical outcomes of different contemporary recanalisation strategies has been the subject of important recent publications, since the focus of current CTO literature has moved from procedural success to optimisation of long-term outcomes2021. The dissection planes created by dissection/re-entry techniques can compromise branches and the distal myocardial bed. Furthermore, they can be accompanied by extensive subintimal haematoma that could lead to stent underexpansion, malapposition and suboptimal vessel healing at follow-up. Finally, they are associated with longer-stented segments. All of the above could theoretically affect the functional outcome of PCI and impact collateral regression since the distal myocardial bed will continue partly to depend on collateral supply. However, similarly to other studies, we did not find any relation between the different recanalisation techniques used and physiological outcome immediately after the index procedure or at follow-up. Changes in collateral function were not different in relation to any of the techniques used.
Limitations
This study has several limitations. First, it must be highlighted that FFRcoll was measured at the end of CTO PCI and not at baseline. Collateral flow after the opening of a CTO can decrease rapidly in some patients, and at the instant when we actually measured collateral flow, its value could have been underestimated. Pv was not measured directly, and a default value of 5 mmHg was used for physiological index calculations. Nevertheless, this is an established methodology within coronary collaterals literature. Even more importantly, the default value selection was based on our previous work, where Pv was measured directly with a 5 Fr pigtail catheter placed at the level of the right atrium13. Recanalisation techniques were classified based on intended strategy, equipment used, clinical experience, and angiographic evaluation. Thus, potential intraplaque or subintimal pathways in dissection/re-entry and wire escalation techniques, respectively, cannot be excluded. Finally, following the recently published CTO-ARC (Academic Research Consortium)22 consensus recommendations on procedural success, we included 2 cases in the analysis with TIMI (Thrombolysis in Myocardial Infarction) flow 2 at the end of the index procedure. In the first case, there was a diffusely diseased vessel of small calibre distal to a long-stented segment, and in the second one, there was competitive flow at the distal vessel by a patent venous graft (this patient had a previous coronary artery bypass graft). Both cases had TIMI 3 flow at follow-up, and in the second case the FFRcoll remained high as the venous graft was still patent at the time of follow-up angiography.
Conclusions
There was significant reduction in resting and hyperaemic collateral flow between the index procedure and 3-month follow-up, independent of the recanalisation technique.
Impact on daily practice
The present study showed that there was significant reduction in collateral flow over time following successful CTO PCI. This change was not influenced by different CTO PCI recanalisation approaches, signifying that intra- and extraplaque crossing strategies have a similar impact on collateral regression.
Funding
The study was supported by Abbott Vascular.
Conflict of interest statement
T. R. Keeble reports research grants from Boston Scientific, Volcano, Terumo, and Abbott Vascular. N.H.J. Pijls reports institutional grants from Abbott, and Hexacath; is a consultant for Abbott, and GE Healthcare; holds minor equities in Philips, ASML, and HeartFlow. J. Davies has received a research grant from Medtronic. G.V. Karamasis reports honoraria and a research grant from Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.