Abstract
Aims: Chronic total occlusions (CTO) are the final stage of atherosclerosis. Occluded coronary arteries have large plaque burden and negative remodelling. The aim of this study was to assess lumen and vessel changes of segments located distal to successfully recanalised CTO.
Methods and results: Ninety-one CTO treated with drug-eluting stents underwent quantitative coronary angiography (QCA) at baseline and at 12-18 months; 31 underwent serial intravascular ultrasound (IVUS) imaging. Angiographic changes were assessed with QCA as differences in minimal, mean and maximal lumen diameter (MinLD, MeanLD and MaxLD, respectively). Vessel changes were assessed with IVUS as changes in plaque and vessel volume. At follow-up, angiographic MinLD increased 23.9% (from 0.88±0.32 to 1.09±0.35 mm; p<0.01), MeanLD 16.4% (from 1.59±0.44 to 1.85±0.45 mm; p<0.01) and MaxLD 11.7% (from 2.39±0.67 to 2.67±0.70 mm; p<0.01). Lumen enlargement was greater in non-restenotic lesions, small lumen area at the end of the index procedure and low LDL-cholesterol levels during the study. By IVUS, lumen volume increased 26.9% (from 108.1±89.2 to 137.3±115.3 mm3; p<0.01), vessel volume increased 12.1% (from 207.1±170.2 to 232.2±196.0 mm3; p<0.01) and plaque volume tended to decrease 3.9% (from 98.9±88.7 to 94.9±89.3 mm3; p=0.07). Small lumen at baseline was related to greater lumen enlargement.
Conclusions: Segments distal to recanalised CTO showed a notable lumen and vessel enlargement with a trend toward mild plaque regression. Low LDL-cholesterol levels increase lumen enlargement.
Abbreviations
CTO: chronic total occlusion(s)
DES: drug-eluting stent
EEM: external elastic membrane
IVUS: intravascular ultrasound
LDL: low-density lipoprotein
MinLD: minimal lumen diameter
MeanLD: mean lumen diameter
MaxLD: maximal lumen diameter
PCI: percutaneous coronary intervention
PTCA: percutaneous transluminal coronary angioplasty
Introduction
Coronary chronic total occlusions (CTO) are defined as lesions with TIMI flow 0 for more than three months1,2. Coronary CTO are found in approximately 15-30% of patients with suspected coronary artery disease referred for coronary angiography. Several studies have demonstrated that successful recanalisation of coronary CTO leads to an improvement in angina status, normalisation of functional tests, improvement in left ventricular function, and avoidance of coronary artery bypass graft3. However, it remains unclear if successful recanalisation of coronary CTO is associated with lower mortality compared to medical treatment4.
Coronary CTO are considered the final stage of coronary atherosclerosis5. Chronically occluded coronary segments have shown an important negative remodelling of the external elastic membrane (EEM) with respect to reference non-diseased segments of the same coronary artery5,6. Moreover, intravascular ultrasound (IVUS) imaging of the coronary segments distal to the occlusion after successful recanalisation has shown an important atherosclerotic burden (>45%)7. As a result, epicardial coronary segments located distal to CTO are often diffusely diseased arteries. It is unclear whether angiographic lesions located at the distal segments of successfully recanalised CTO immediately after intervention are related to cardiac events at follow-up or whether these lesions require percutaneous coronary intervention (PCI) with stent implantation8.
The aim of this study was to investigate the lumen and plaque changes of the segments distal to successfully recanalised coronary CTO at 12-18 months follow-up. This study also aimed to assess the angiographic and IVUS predictors at the index procedure related to lumen enlargement at follow-up.
Methods
POPULATION
All patients with at least one coronary CTO who underwent percutaneous coronary intervention (PCI) were prospectively registered in our institution from December 2008 to December 2010. All enrolled patients were symptomatic for angina and/or had documented ischaemia/viability by non-invasive tests in myocardial regions supplied by the CTO. Patients with contraindications to dual antiplatelet therapy, advanced renal dysfunction (creatinine clearance ≤30 ml/min) or short-term life expectancy were excluded from the study. The inclusion and exclusion criteria are listed in the Online Appendix.
All patients successfully recanalised underwent clinical and one invasive follow-up between 12 and 18 months after the stent implantation. The last consecutive 31 patients were also imaged with IVUS at baseline and at follow-up. All patients gave their written informed consent to participate in the study. The study protocol was approved by the local ethics committee and complied with the Declaration of Helsinki. There was no funding source for this study.
PROCEDURAL CHARACTERISTICS
All cases were performed by anterograde approach, electively, post hoc, using dedicated equipment and by a single experienced operator. Nitroglycerine was administered after successful recanalisation of the coronary occlusion. Stent implantation was limited to the occluded segment and to angiographic stenoses proximal to the occluded segment. In case of flow-limiting angiographic stenoses located distally to the stent edge, these stenoses were treated using percutaneous transluminal coronary angioplasty (PTCA) at low pressure (2-4 atmospheres) in order to restore TIMI 3 flow. In cases without flow restoration after PTCA, stent implantation was performed at the distal segment. IVUS imaging of distal coronary segments was performed after all interventions at least 30 mm distal to the stent edge. At follow-up, IVUS imaging was performed within the imaged segment at baseline. All IVUS recordings were acquired using the 40 MHz Atlantis SR Imaging Catheter (Boston Scientific Corporation, Natick, MA, USA). Pharmacological treatment is reported in the Online Appendix.
ANGIOGRAPHIC AND IVUS ANALYSES
Two experienced analysts performed quantitative angiographic analysis (QCA) and IVUS measurements. The methodology used is explained in the Online Appendix. In summary, angiographic coronary segments located at least 30 mm distally to the distal stent edge were analysed every 5 mm. The following QCA parameters were measured for each segment: the minimal luminal diameter (MinLD), the mean luminal diameter (MeanLD) and the maximal lumen diameter (MaxLD). IVUS volumetric analysis was also performed in matched segments at baseline and at follow-up according to clear landmarks.
STATISTICAL ANALYSIS
The Kolmogorov-Smirnov test was used to evaluate the normality assumptions of continuous variables. Continuous variables were expressed as mean±1 standard deviation. Categorical variables were expressed as counts (%). Comparisons between post-intervention and follow-up values were estimated using the paired t-test analysis. In case of non-normal distribution, comparisons between post-intervention and follow-up values were estimated with the Wilcoxon test.
Predictors of angiographic MeanLD and IVUS-derived lumen volume enlargement were investigated using a generalised estimating equation method. The relative differences of MeanLD and lumen volume between baseline and follow-up were used as dependent variables for the univariate and multivariate analyses. Univariate analysis of angiographic predictors of lumen enlargement included all clinical and angiographic parameters. Univariate analysis of IVUS predictors of lumen enlargement at follow-up included all IVUS parameters. Angiographic and IVUS parameters with a p-value <0.2 in the univariate analysis were included in the multivariate model. A two-tailed p-value <0.05 was considered significant. Linear correlations between continuous quantitative data were estimated with the Pearson coefficient. All measures were obtained with SPSS 15.0 (SPSS Inc., Chicago, IL, USA).
Results
During the study period, 117 coronary CTO were successfully treated in 111 patients. A total of 26 coronary CTO lesions in 25 patients were excluded from this study. A flow chart with the patient selection is shown in Figure 1. Ninety-one coronary CTO lesions in 86 patients were included.
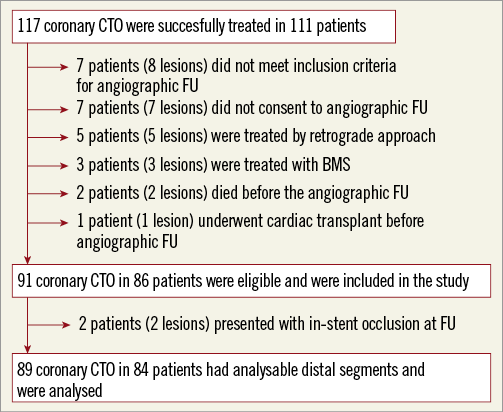
Figure 1. Flow chart of the study. BMS: bare metal stent; CTO: chronic total occlusions
CLINICAL AND ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
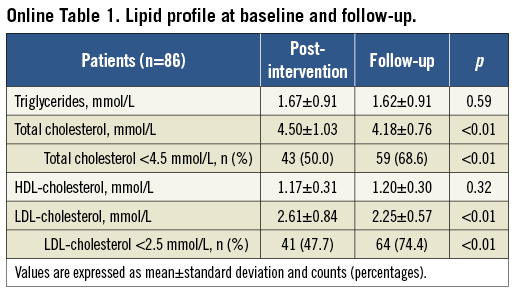
Table 1 shows the clinical characteristics of the patients included in the present study. Mean age was 62.7±10.9 years, 88.4% of the subjects were male and 39.5% were diabetic. The lipid profile of the patients is shown in the Online Appendix. On average, total cholesterol decreased 7.1% and LDL-cholesterol decreased 13.8%. Triglycerides and HDL-cholesterol remained unchanged.
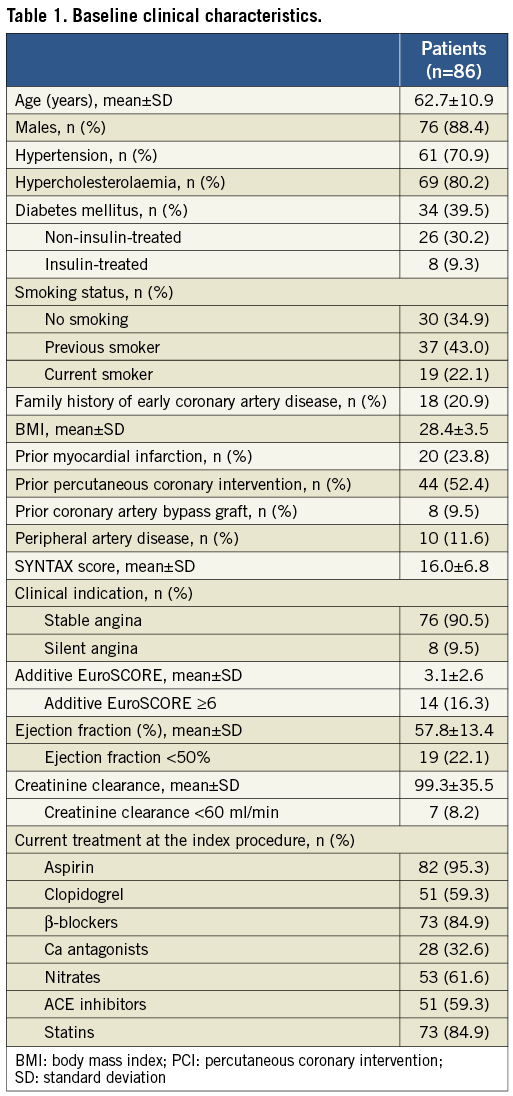
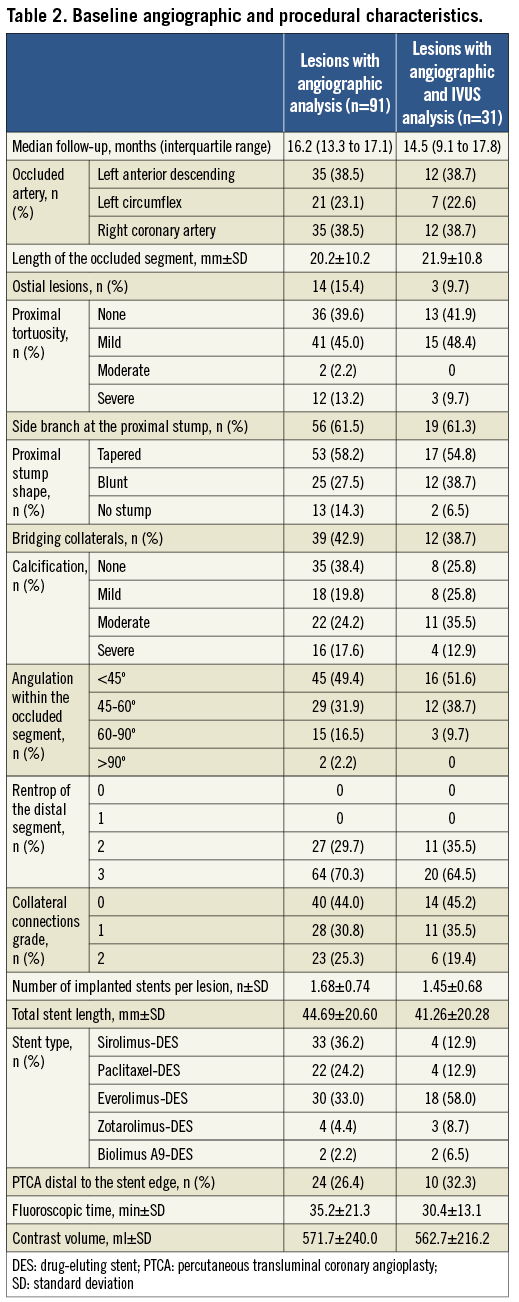
Table 2 shows the baseline angiographic and procedural characteristics. Angiographic follow-up was performed at 16.2 months (median). Total length of the implanted stents per lesion was 44.69±20.60 mm. PTCA of flow-limiting distal lesions was performed in 24 lesions (26.4%). One patient (1.1%) did not return to TIMI 3 flow after PTCA and was successfully treated with a DES.
QUANTITATIVE CORONARY ANGIOGRAPHY ANALYSIS
Nine patients with nine lesions (9.9%) presented with angiographic in-segment restenosis at follow-up; two patients presented with stable angina and were re-catheterised at four and nine months after PCI, respectively. Two patients presented with complete reocclusion of the treated lesion at follow-up and were excluded from the distal segment analysis. One patient (1.1%), treated with PTCA at low dilatation pressure at the index procedure because of a distal flow-limiting angiographic lesion, presented with an asymptomatic restenosis of the treated segment and was treated with DES implantation at follow-up.
Table 3 shows the quantitative angiographic results of the 5 mm proximal segment, the in-stent segment, and the 5 mm segment distal to the stent edge. A mean of 55.62±19.62 mm of the distal coronary segments were analysed per lesion. The lumen diameter of the coronary segments distal to the in-segment edge increased from baseline to follow-up (23.9% MinLD, 16.4% MeanLD and 11.7% MaxLD; p<0.001). Figure 2 shows the matched segments between baseline and follow-up of all lumen diameters.
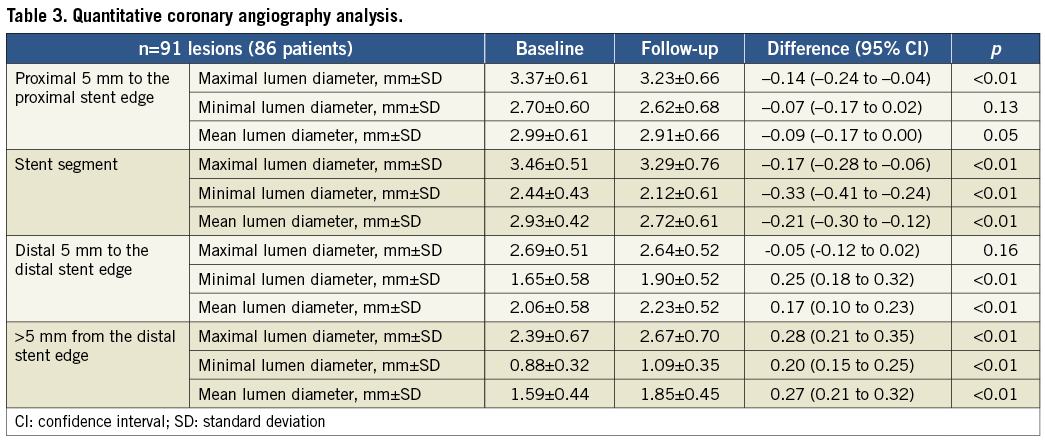
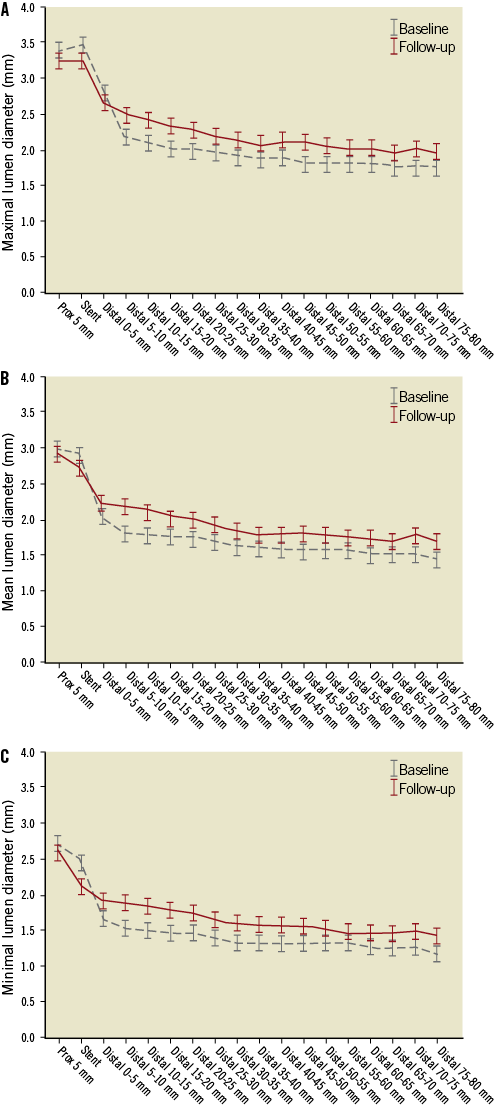
Figure 2. Angiographic A) maximal, B) mean and C) minimal lumen diameter changes between baseline and follow-up.
Univariate predictors of greater lumen enlargement were: female gender, creatinine clearance, mean LDL-cholesterol during the study period, mean HDL-cholesterol during the study period, absolute difference in LDL-cholesterol between baseline and follow-up, mean lumen diameter at baseline, PTCA of the distal segment at baseline and absence of restenosis at follow-up. Independent predictor factors of greater lumen enlargement were: absence of angiographic in-segment restenosis, low levels of LDL during the study period and small mean lumen area at baseline. Figure 3 shows the relationship between the percentage of mean lumen diameter changes and the mean LDL-cholesterol during the study period and the mean lumen diameter at baseline in patients without angiographic restenosis at follow-up.
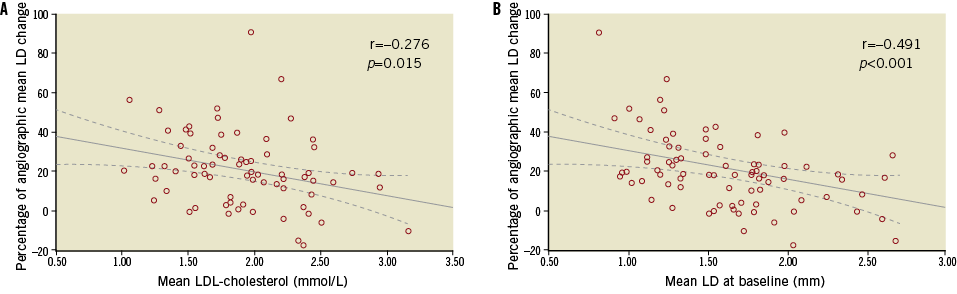
Figure 3. Angiographic changes in lumen area according to A) LDL-cholesterol and B) lumen diameter at baseline. Relationship between percentage of angiographic mean lumen diameter changes and LDL-cholesterol and angiographic mean lumen diameter at baseline excluding patients with in-segment angiographic restenosis.
QUANTITATIVE CORONARY ULTRASOUND ANALYSIS
A total of 44 matched segments in 31 consecutive lesions in 31 patients were imaged with IVUS at baseline and follow-up. The median (interquartile range) length of each analysed segment was 22.0 mm (15.0 to 31.2 mm). Table 4 shows the quantitative coronary ultrasound analysis of the segment distal to the stent edge. From baseline to follow-up, lumen volume increased 27% (from 108.11 to 137.32 mm3; p<0.01), vessel volume increased 12.1% (from 207.08 to 232.19 mm3; p<0.01) and plaque volume tended to decrease 3.9% (from 98.85 to 94.93 mm3; p=0.07). A total of 25 segments (56.8%) had calcification and one segment (2.3%) had intramural haematoma.
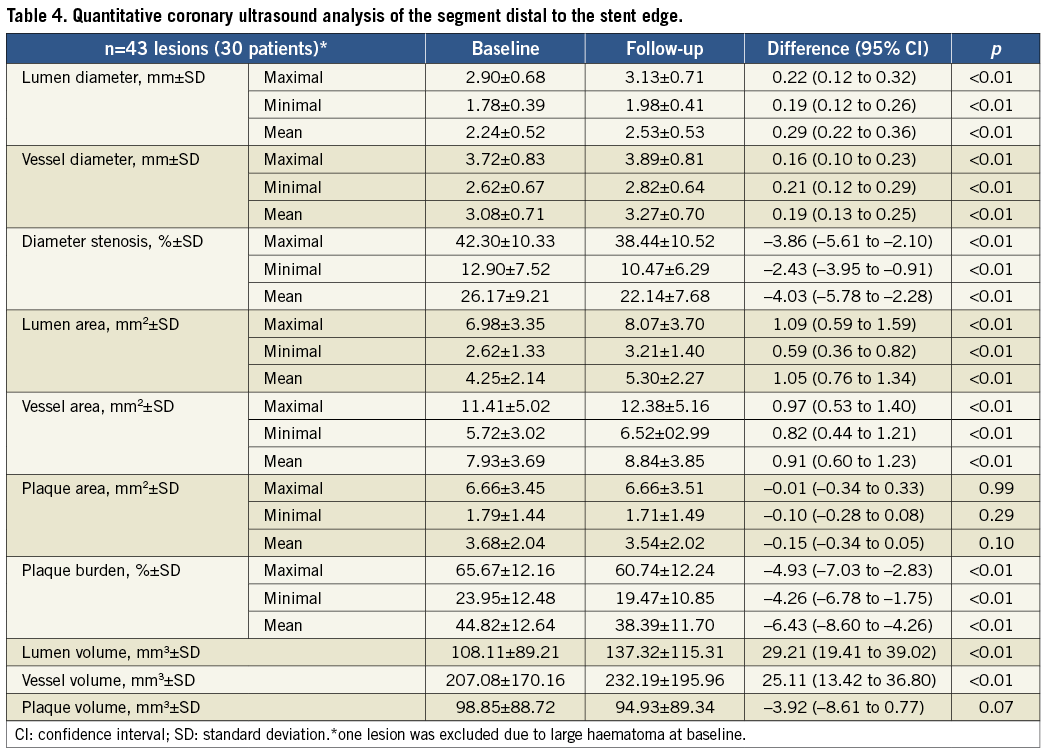
Univariate predictors of IVUS-derived lumen enlargement were: mean plaque burden at baseline, severe calcification and mean lumen area at baseline. The only independent predictor factor related to greater percentage of lumen volume enlargement was the mean lumen area at baseline.
Figure 4 shows the relationship between percentage of IVUS-derived lumen, plaque and vessel volume changes and mean LDL-cholesterol levels during the study period. Figure 5 shows the angiographic and IVUS imaging of the patient with greatest lumen enlargement.
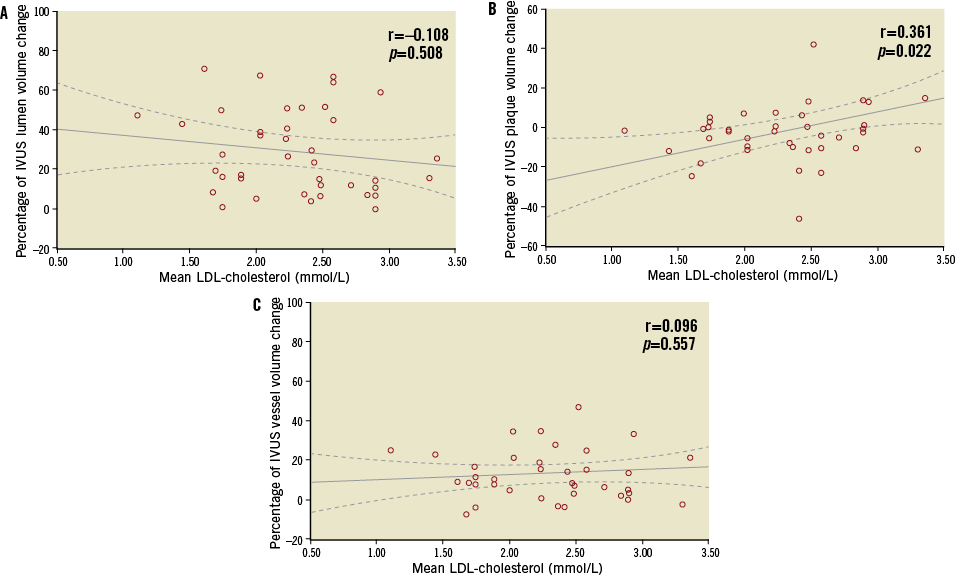
Figure 4. IVUS changes in A) lumen, B) plaque and C) vessel volume according to LDL-cholesterol. Relationship between percentage of IVUS-derived lumen, plaque and vessel volume changes and mean of LDL-cholesterol levels during the study period.
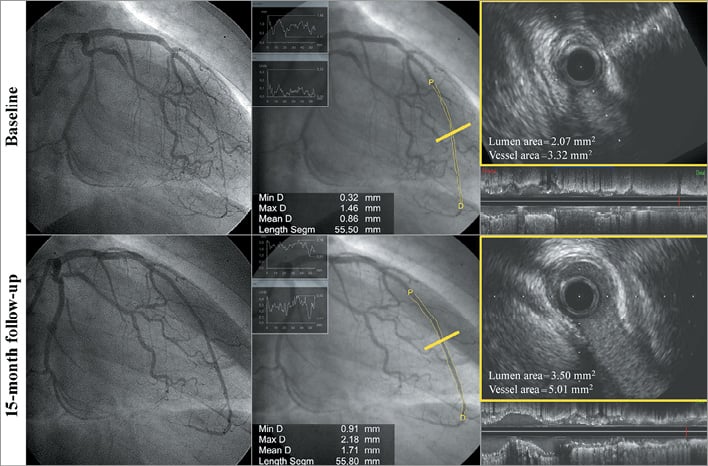
Figure 5. Angiographic and IVUS imaging of patient with greatest lumen enlargement. Images recorded at baseline and 15-month follow-up after nitroglycerine.
Discussion
The main findings of this study are: 1) there is a notable increase in lumen size in the segments distal to successfully recanalised coronary CTO between baseline and follow-up; 2) late lumen enlargement is mainly caused by enlargement of the EEM and by a trend towards plaque reduction, although plaque reduction was not statistically significant.
To the best of our knowledge, this is the first study to have performed IVUS volumetric analysis of matched coronary segments distal to successfully recanalised CTO. This is noteworthy since it is considered the best methodology to assess lumen, plaque and EEM changes of native coronary arteries9. The late lumen enlargement of coronary segments distal to successfully recanalised CTO found in this study can be explained by two different mechanisms: first, enlargement of the EEM, and second, plaque regression between baseline and follow-up.
Enlargement of the EEM has been previously reported by Park et al in 58 patients imaged with IVUS at index procedure and at six months10. In this study, the EEM of the distal coronary segments increased 12.5% from baseline to follow-up10. This result is similar to the 11.5% increase observed in the present study. Enlargement of the EEM together with plaque progression has been observed at the early stages of coronary atherosclerosis and is defined as positive remodelling5. However, this study showed a trend towards plaque reduction and therefore the phenomenon of EEM enlargement cannot be described as positive remodelling. The most probable explanation of the EEM enlargement observed between baseline and follow-up is the restoration of the vasomotor tone of the coronary segments distal to successfully recanalised CTO. Distal epicardial segments have shown an important impairment of the vasomotion function to endothelium-independent stimuli (nitroglycerine) immediately after successful recanalisation11,12. At follow-up, endothelium-independent response (to nitroglycerine) is restored in most patients, showing a remarkable luminal gain compared to the index procedure11.
The second cause of lumen enlargement of coronary segments located distal to successfully recanalised CTO is plaque regression. Plaque volume and plaque area tended to decrease by 3.9% and 4.0% between baseline and 12-18 months follow-up, although this difference was not statistically significant. Park et al also observed a trend towards plaque area reduction of 1.8% at six-month follow-up10. The most probable cause of plaque reduction is the intensive statin therapy. Different serial IVUS-imaging studies before and after intensive statin treatment have shown a remarkable plaque volume reduction (of 8-11%) in non-occluded coronary arteries9,13. In those studies, plaque volume reduction was also associated with a mild lumen volume increase (of 1-2%) and with a notable EEM shrinkage (of 7-8%) from baseline to follow-up9,13. Moreover, previous studies have demonstrated that plaque volume progression/regression was linearly correlated with the mean LDL-cholesterol levels during the study period9. The present study, using intensive statin therapy, has also shown a trend towards larger lumen volume increase and plaque volume reduction in patients with low levels of LDL-cholesterol during the study period (Figure 4). However, in this study, EEM enlargement was not correlated with the LDL-cholesterol levels during the study period (Figure 4). The negative impact of LDL-cholesterol levels with EEM changes can be explained by the fact that 84% of the IVUS segments presented with EEM enlargement.
Angiographic lesions located distal to successfully recanalised CTO are frequently observed8. So far, it is uncertain if these angiographic lesions are related to clinical events at follow-up, and it is still uncertain if these lesions need to be treated with a stent. According to the results of this study, in case of non-flow-limiting lesions located distal to successfully recanalised CTO, a conservative approach with intensive statin therapy should be considered. In case of flow-limiting lesions, PTCA with low dilatation pressure is useful to restore TIMI 3 flow during the index procedure, and it is associated with good clinical and angiographic results at one-year follow-up. However, further investigations are required in order to assess the best clinical management of lesions located distal to successfully recanalised coronary CTO.
Limitations
This study was observational in nature. It is uncertain if the lumen and vessel changes of the coronary fields distal to successfully recanalised CTO at 12-18 months can be observed in the very early phase after coronary intervention. Moreover, an endothelial function test of the distal segment after successful recanalisation of the coronary CTO was not performed. It is uncertain if endothelium-mediated vasomotion could have played a role in the lumen enlargement observed in the present study.
Conclusion
Segments distal to successfully recanalised coronary CTO showed an important lumen and vessel enlargement at 12-18 months follow-up. Late lumen enlargement can be caused by the absence of vasomotor response to non-endothelium-mediated stimuli immediately after recanalisation. Moreover, mild plaque regression under intensive statin treatment and an important decrease of LDL-cholesterol levels can also contribute to late lumen enlargement. Therefore, in cases of non-flow-limiting lesions located distal to successfully recanalised CTO, medical treatment with intensive statin therapy should be considered.
| Impact on daily practice Angiographic lesions located distal to coronary CTO are often observed immediately after CTO recanalisation and usually require to be treated with long stent lengths. However, a conservative approach with PTCA at low pressure in order to restore TIMI 3 flow can be used with good clinical and angiographic results at follow-up. Intensive statin treatment can also play a role in the lumen enlargement of these segments. |
Funding
This study was performed as an investigator initiative and has not received any funding. The first author of the manuscript was awarded a grant by the IDIBELL (Institut d’Investigacio Biomedica de Bellvitge).
Conflict of interest statement
J.L. Ferreiro declares honoraria for lectures from AstraZeneca, Daiichi Sankyo Inc. and Eli Lilly Co. The other authors have no conflicts of interest to declare.
Appendix. Study methodology.
INCLUSION AND EXCLUSION CRITERIA
Patients with moderate renal dysfunction (creatinine clearance <45 ml/min), contrast-induced nephropathy during the index procedure or high radiation dose did not undergo invasive follow-up and were therefore excluded from the study. Retrograde cases were performed as bail-out treatment after unsuccessful recanalisation by anterograde approach (usually by subintimal wiring of the distal segment) and required high fluoroscopic time. For these reasons, retrograde cases were also excluded from the study.
PROCEDURAL CHARACTERISTICS
After successful recanalisation of a coronary CTO, all patients were treated with dual antiplatelet therapy with aspirin and clopidogrel for a minimum of one year. Patients not receiving statins at the time of the index procedure were treated with atorvastatin (40 mg/day) after successful recanalisation. Lipid profile was screened before the coronary intervention and several times post procedure in order to achieve the recommended cholesterol levels as outlined by the current guidelines for secondary prevention1. Total cholesterol and LDL-cholesterol levels had target values of <4.5 mmol/L and <2.5 mmol/L, respectively14.
ANGIOGRAPHIC ANALYSIS
After successful recanalisation of a coronary CTO treated with drug-eluting stent (DES) implantation, at least 200 mcg of intracoronary nitroglycerine was administered. The operator was requested to record at least two angiographic views with minimal foreshortening of the implanted stent and limited overlap with other vessels. These angiographic views were repeated at follow-up after infusion of at least 2 mg of intracoronary nitroglycerine.
Angiographic analysis was performed by two experienced analysts using the coronary angiography analysis software (CAAS) version 5.9 (Pie Medical BV, Maastricht, The Netherlands). After adequate calibration, the “in-stent” region (defined by the segment between the two stent edges) and the “in-segment region” (defined by the segment between the 5 mm proximal and 5 mm distal to the stent edges) were analysed. Coronary segments located at least 30 mm distally to the distal stent edge were analysed every 5 mm. Both operators were requested to match all analysed segments between baseline and follow-up using clear anatomical landmarks. Quantitative coronary angiography (QCA) analysis was performed at end diastole.
Rentrop and collateral connection (CC) classification were assessed qualitatively by two analysts15,16.
IVUS ANALYSIS
IVUS analysis was performed by two experienced analysts using the quantitative coronary ultrasound (QCU) analysis software (QCU CMS 6.1; Medis, Leiden, The Netherlands)17. In order to assess exactly the same segment between the index and follow-up images, clear anatomical landmarks such as the distal stent edge and side branches were used during the IVUS analysis. Coronary arteries distal to CTO were divided into matched segments at baseline and at follow-up according to clear landmarks. Side-branch segments of >1/3 of the lumen perimeter were excluded from the analysis. Intramural haematomas were defined as accumulations of homogeneous crescent-shaped hyperechogenic structures within the medial space7. Segments with intramural haematoma were identified and were excluded from the analysis. Presence of calcification was assessed qualitatively when a coronary segment >2 mm presented with a hyperechogenic image with acoustic shadow behind18.
After an appropriate calibration of the analysis software, lumen cross-sectional area was quantified by planimetry of the leading edge of the blood-intima acoustic interface. The outer vessel border (external elastic membrane) was detected as the interface between media and adventitia and defined as vessel area. Plaque area was calculated as the difference between vessel area and lumen area18. Volumetric reconstructions of each lumen, vessel and plaque area were performed automatically by the analysis software taking into account the frame rate and the pullback speed19.
Discussion
This study found that predictors of greater lumen enlargement at follow-up were: absence of restenosis, small lumen size at the end of the index procedure and mean levels of LDL-cholesterol during the study period. Park et al found that independent predictors of lumen enlargement were: occlusion duration, a poor collateral flow, and statin use20. It is noteworthy that none of the studies has been able to find any IVUS-derived predictor of lumen enlargement at follow-up.
It is widely accepted that segments distal to stenotic lesions are associated with larger endothelial dysfunction and with lower vasodilator response to nitroglycerine than non-stenotic lesions21. Therefore, the relationship between small baseline lumen size and greater lumen enlargement at follow-up can be explained by the lower vasodilator response to nitroglycerine of the vessels with small lumen diameter/volume at baseline. Vessels with low response to nitroglycerine at baseline experience larger changes in lumen size once the vasomotion function is restored at follow-up. Low levels of LDL-cholesterol during the study period are related to greater lumen enlargement at follow-up because of a more pronounced plaque reduction than those observed in patients with high levels of mean LDL-cholesterol during the study. It is noteworthy that segments distal to coronary CTO presented with a significant plaque burden (mean plaque burden of 45% in the present study) and 56.8% of segments had coronary calcification. Moreover, statin therapy has been associated with anti-inflammatory effects that prevent reperfusion injury after acute total occlusion recanalisation and decrease the periprocedural acute myocardial infarction even in patients with normal levels of LDL-cholesterol22.

