A 75-year-old man presented with stable effort angina and normal cardiac biomarkers 10 years after the implantation of two bare metal stents in the proximal right coronary artery. Coronary angiography revealed a moderate lesion on the left anterior descending coronary artery, diffuse distal disease and good results of the two stents. However, a minor, intraluminal filling defect was detected in the segment between the two stents (Appendix Figure 1, Moving image 1). Optical coherence tomography (OCT), with the novel “co-registration” technique, confirmed excellent results in the two stents, nicely covered by a mild layer of homogeneous neointima. However, OCT demonstrated a bright, finger-like structure, deeply protruding into the lumen causing major posterior shadowing (*) (Figure 1, Moving image 2) at the site showing the filling defect on co-registration imaging. Large superficial calcified plates (+) were also detected. Considering the stable clinical presentation, this image was considered diagnostic of a calcified nodule with a large residual lumen and was left untreated.
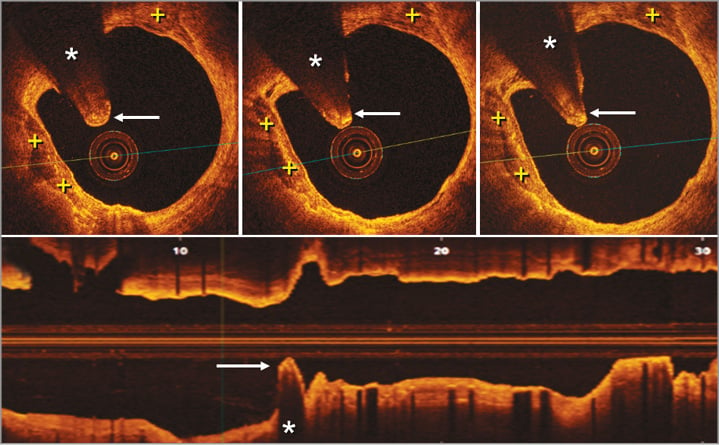
Figure 1. Optical coherence tomography. Top: a bright protruding “finger-like” structure (arrows) with dorsal shadowing (*) is clearly depicted. Additional superficial calcified plates (+) are visualised on the vessel wall. Bottom, longitudinal display: notice that the guidewire had been removed to avoid any artefacts.
Angiographic filling defects typically correspond to intracoronary thrombi. However, classic intravascular ultrasound studies have demonstrated that some angiographic filling defects may actually be caused by heavily calcified coronary plaques. Alternatively, bright tissue protruding into the lumen and casting a major dorsal shadow constitutes the hallmark of a “red” thrombus on OCT. Very recently, however, it has been demonstrated that images of bright protruding intracoronary tissue inducing an intense posterior shadow may indeed correspond to uncomplicated calcified nodules not associated with overlying thrombosis. The presence of a distinct superficial border line on top of the protrusion image, just slightly separate from the lumen, and the existence of extensive calcification of the adjacent vessel wall are additional clues to suggest the presence of a calcified nodule. Our findings illustrate that a stable calcified nodule may mimic an intracoronary thrombus on both coronary angiography and OCT, thus explaining this “double paradox” on coronary imaging. A high degree of clinical suspicion remains crucial for the correct diagnosis of this elusive clinical entity.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
The legends of the Moving images can be found in the Appendix.
Moving image 1. Coronary angiography of the right coronary artery in the left anterior oblique projection showing a faint small intraluminal filling defect located in the proximal segment of the vessel between the two previously implanted bare metal stents.
Moving image 2. Optical coherence tomography images of the proximal right coronary artery. The distal stent is nicely covered by a thin ring of homogeneous bright tissue. The segment between the two stents is heavily calcified but with a large lumen. A bright finger-like protruding mass inducing dorsal shadowing is clearly depicted. The proximal stent also shows a good lumen, although some struts are not fully covered and others show malapposition. The exit of a large right ventricular branch and the location of the proximal aspect of the stent with respect to the coronary ostium are also readily recognised.
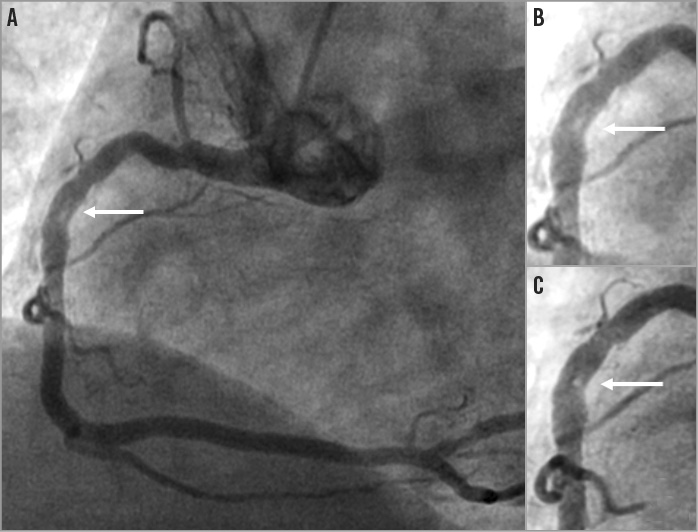
Appendix Figure 1. A) Angiographic filling defect (arrow) in the proximal right coronary artery. B) & C) Magnified images.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Coronary angiography of the right coronary artery in the left anterior oblique projection showing a faint small intraluminal filling defect located in the proximal segment of the vessel between the two previously implanted bare metal stents.
Moving image 2. Optical coherence tomography images of the proximal right coronary artery. The distal stent is nicely covered by a thin ring of homogeneous bright tissue. The segment between the two stents is heavily calcified but with a large lumen. A bright finger-like protruding mass inducing dorsal shadowing is clearly depicted. The proximal stent also shows a good lumen, although some struts are not fully covered and others show malapposition. The exit of a large right ventricular branch and the location of the proximal aspect of the stent with respect to the coronary ostium are also readily recognised.