A 59-year-old man presented to the emergency department with sustained chest pain. Emergency coronary angiography (CAG) revealed an occluded right coronary artery (RCA) (Figure 1A). After aspiration, a coronary stent was implanted. Histopathological examination showed that the thrombus contained cholesterol crystals and foam cells (Figure 1B and Figure 1C). He was discharged 11 days later without any complications.
A 320-slice multidetector computed tomography (CT) had been accidentally performed five days prior to plaque rupture. He had been suffering from stable angina with ST depression in leads II, III, and aVF, and without elevation of cardiac enzymes. He preferred non-invasive coronary CT to CAG at first. CT images demonstrated moderate luminal narrowing in the RCA (Figure 1D, Figure 1E and Figure 1F) and the lesion had a large calcification, which associated with stable plaque (Figure 1G). Notably, we observed a specific type of cross-sectional image, the so-called signet ring-like appearance (Figure 1H).
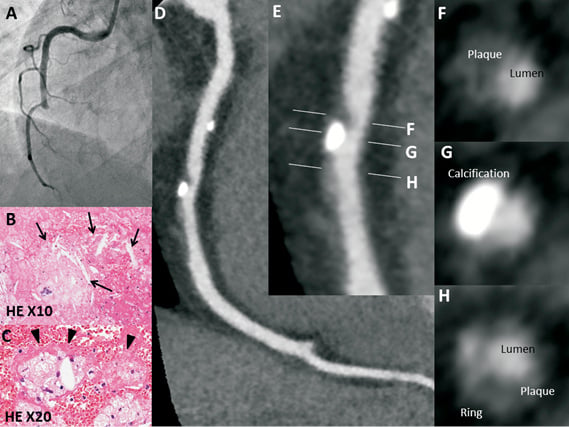
Figure 1. Angiography showed complete occlusion of the middle RCA (A). The thrombus contained cholesterol crystals (arrows, B) and foam cells (arrowheads, C). The images showed the multiplanar reconstruction image of the RCA (D and E). The lumen was moderately narrowed by a moderate CT density plaque (60 HU in the cross-sectional view, F) and the plaque contained a focal large calcification (G). The signet ring-like appearance, defined as a semicircular thin enhancement, was observed along the outer contour of the vessel wall (H).
This appearance has been defined as a semicircular thin enhancement (CT density >130 HU) along the outer contour of the vessel wall in cross-sectional views1. This appearance might indicate deep calcification within lipid-rich plaque containing a necrotic core or intraplaque vasa vasorum, which is one of the specific features of vulnerable plaque.
Conflict of interest statement
The authors have no conflicts of interest to declare.

