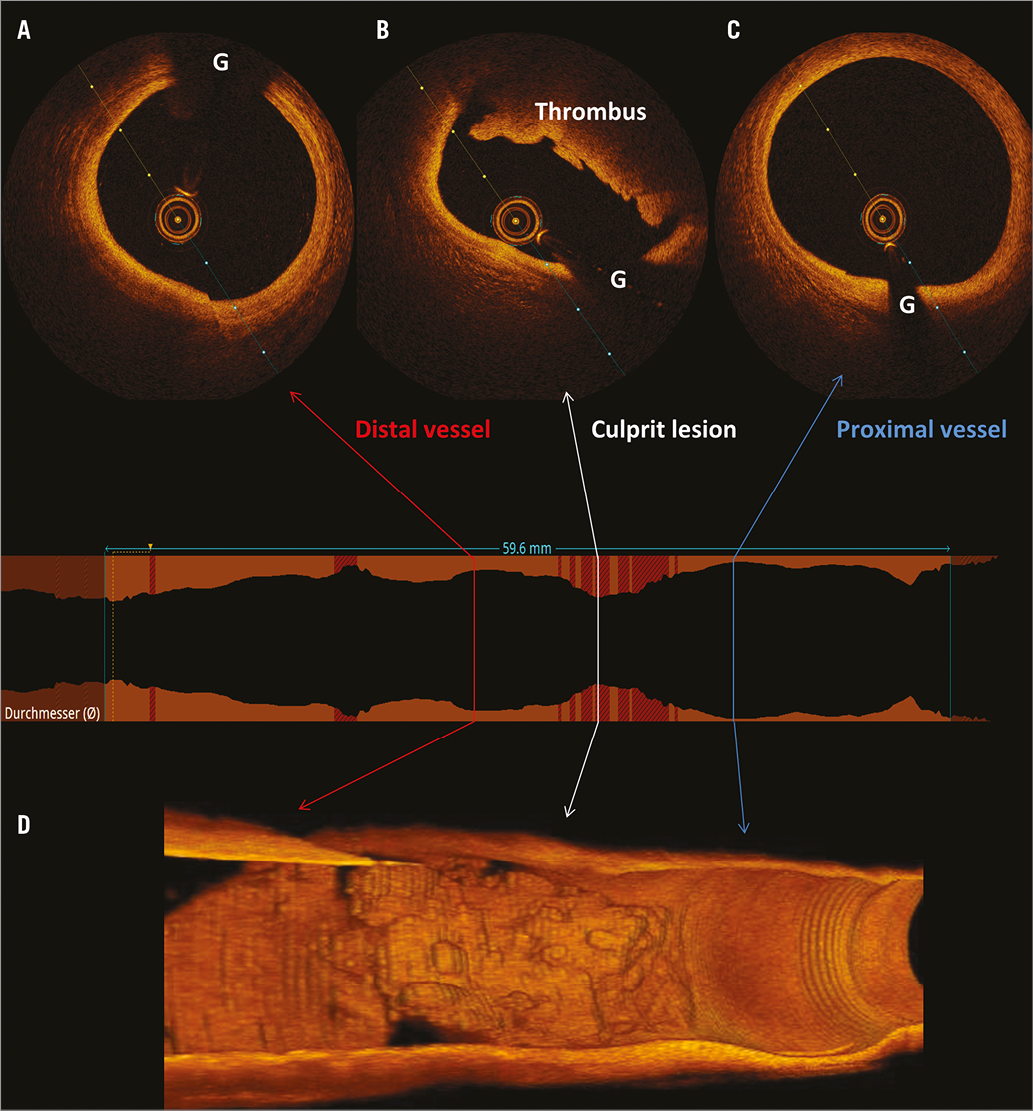
A 35-year-old male endurance athlete presented with a history of stuttering chest pain, which began four days earlier after a final training session for a cycling marathon. Symptoms recurred two days later during and after the marathon event, prompting presentation to our department. He was a non-smoker with no known cardiac risk factors. An electrocardiogram showed anterior ST-elevation (Appendix Figure 1). Coronary angiography showed moderate-to-severe mid left anterior descending (LAD) artery stenosis with distal vessel occlusion (Appendix Figure 2, Moving image 1), impenetrable to guidewire passage. Optical coherence tomography (OCT) imaging (Panel A-Panel C, G=guidewire artefact) – including 3D reconstruction (Panel D, Moving image 2) – of the mid LAD lesion showed focal intimal thickening with overlying thrombus and no detectable fibrous cap rupture (Panel B). There was no evidence of coronary dissection, and normal vessel wall architecture was preserved proximal (Panel C) and distal (Panel A) to the lesion. As the underlying plaque was not well visualised due to residual thrombus, this was considered probable OCT erosion. The lesion was treated with an everolimus-eluting stent. The subsequent clinical course was uneventful and the patient was discharged to cardiac rehabilitation and advised to avoid high-performance sport.
Although plaque rupture is responsible for most cases of ST-elevation myocardial infarction1, plaque erosion is an important – but underdiagnosed – substrate for coronary thrombosis, accounting for one third of cases in autopsy and OCT series1,2. In contrast to lipid-rich thin-cap fibroatheromas (TCFA) typically underlying plaque rupture, plaque erosion is characterised histologically by endothelial erosion of intact fibroatheroma, rich in smooth muscle cells, and often lacking lipid core. The degree of luminal stenosis is typically less than that seen with ruptured plaques due to repeated rupture-healing phases seen with TCFA plaques. Thrombus overlying exposed collagen in eroded plaques more frequently forms slowly as “white” thrombus (symptoms often developing over days), is less often occlusive, and more frequently embolises, causing occlusion of the distal vessel, all features observed in this present case. Plaque rupture, on the other hand, causes expulsion of highly thrombogenic necrotic core, typically precipitating rapid formation of “red” thrombus, which often completely occludes the vessel.
Plaque erosion occurs more commonly in females, smokers, and in younger patients with fewer cardiovascular risk factors, less coronary artery calcification and single-vessel disease3. Its triggers are poorly understood. In our patient, sympathetic stimulation with extreme physical exertion may have induced local spasm in a coronary segment with pathological intimal thickening, which may have caused erosion of the overlying endothelium.
Eroded plaque is best identified in vivo by OCT: its high spatial resolution allows fibrous cap visualisation, though resolution is insufficient to identify individual endothelial cells, hence the term “OCT erosion” should be preferred. The differences in substrates for coronary thrombosis may have implications for management: while stenting of ruptured plaques is usual care, optimal treatment of eroded plaques requires further investigation4.
Conflict of interest statement
R. Colleran reports having received funding from the Irish Board for Training in Cardiovascular Medicine sponsored by MSD. M. Joner reports having received speaker fees from Biotronik, Boston Scientific, AstraZeneca, Coramaze, and OrbusNeich, as well as grants from Biotronik and the European Society of Cardiology. R.A. Byrne reports receiving lecture fees from B. Braun Melsungen AG, Biotronik and Boston Scientific and grants to the institution from Boston Scientific and HeartFlow. The other author has no conflicts of interest to declare.
Supplementary data
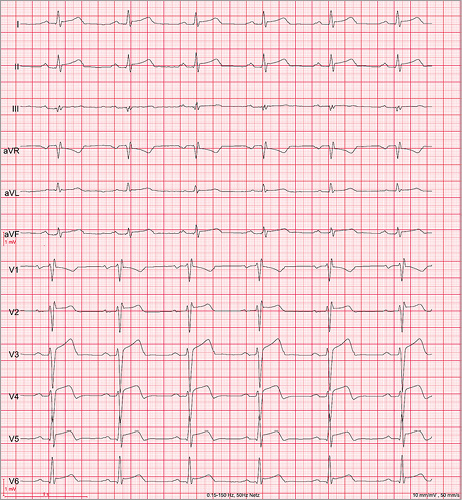
Appendix Figure 1. 12-lead electrocardiogram showing ST-segment elevation in the anterior leads.
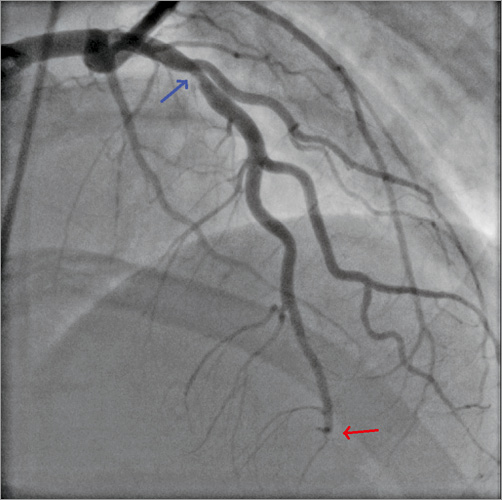
Appendix Figure 2. Coronary angiography showing moderate-to-severe mid LAD stenosis (blue arrow) with distal vessel occlusion (red arrow).
Moving image 1. Coronary angiography showing moderate-to-severe mid LAD stenosis with distal vessel occlusion.
Moving image 2. 3D reconstruction of the mid LAD lesion with overlying thrombus, no visible fibrous cap rupture and normal architecture of the adjacent vessel wall.
Supplementary data
To read the full content of this article, please download the PDF.
Coronary angiography showing moderate-tosevere mid LAD stenosis with distal vessel occlusion.
3D reconstruction of the mid LAD lesion with overlying thrombus, no visible fibrous cap rupture and normal architecture of the adjacent vessel wall.