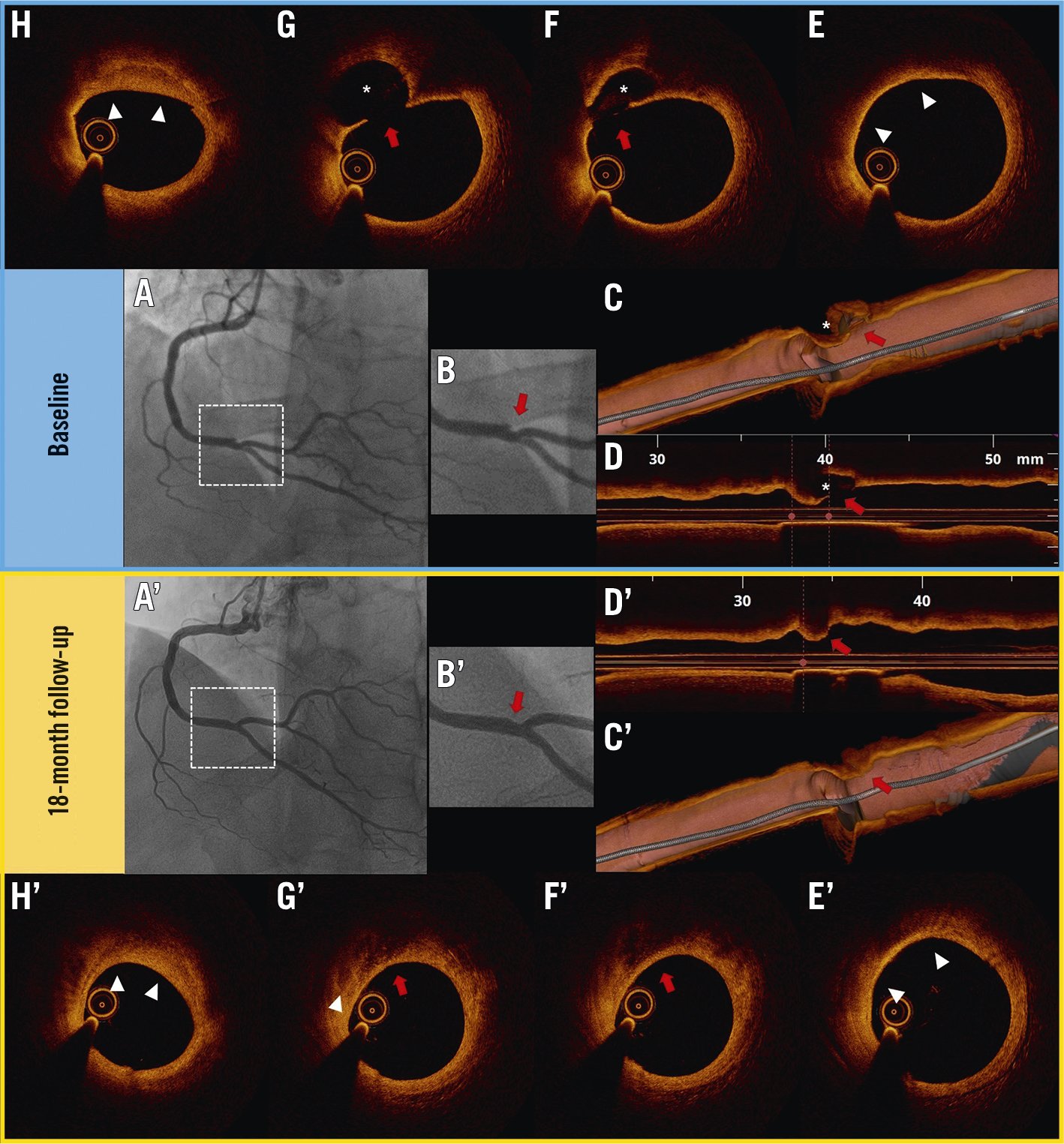
Figure 1. Plaque rupture healing detected by serial optical coherence tomography imaging. A-B) Right coronary artery (RCA) angiogram showing a focal, complex lesion at the crux (red arrow in magnification). C-D) 3D and 2D longitudinal OCT views showing a plaque rupture (red arrows) with a large empty cavity (asterisks). E) Thin-cap fibroatheroma (white arrowheads). F-G) Ruptured plaque, with a fibrous cap discontinuity (red arrows) and a cavity (asterisks). H) Layered pattern (white arrowheads). A’-B’) Follow-up RCA angiogram showing a resolution of the ulceration and a smooth vessel profile (red arrow in magnification). C’-D’) Follow-up 3D and 2D longitudinal OCT views showing a smooth vessel profile at the site of the previous plaque rupture (red arrows). E’) Thick-cap fibroatheroma. F’-G’) Complete healing of the ruptured plaque (red arrows) and initial calcification formation (white arrowhead). H’) Layered pattern (white arrowheads).
A 64-year-old man, a prior smoker, with a history of paroxysmal atrial fibrillation was referred to our hospital due to dyspnoea, progressively worsening angina and a positive stress electrocardiogram (ECG) test. The coronary angiography (CAG) showed intermediate stenosis of the mid-left anterior descending (LAD) artery, which was deferred based on a normal fractional flow reserve (FFR), and a focal, complex lesion of the distal right coronary artery (RCA) (Moving image 1, Figure 1A, Figure 1B, red arrow). Optical coherence tomography (OCT) imaging (ILUMIEN OPTIS; Abbott) was performed to better characterise the RCA lesion (Moving image 2), disclosing a ruptured thin-cap fibroatheroma (TCFA) with a large “empty” cavity (Figure 1C-Figure 1G, red arrows) and overlying “layered” tissue (Figure 1H, white arrowheads). Based on these OCT findings, which were suggestive of initial plaque healing, and on a large residual lumen dimension (i.e., minimum lumen area [MLA] at the rupture site: 7.7 mm2), this lesion was not treated by percutaneous coronary intervention. The patient was discharged on aspirin, edoxaban, metoprolol, ramipril, rosuvastatin and ezetimibe, and he remained clinically stable for more than 1 year. Due to angina recurrence, a new CAG was performed 18 months after the first admission, revealing a progression of the mid-LAD stenosis; this was treated with a 2.5/28 mm everolimus-eluting stent. A right coronary angiogram showed an improvement of the distal RCA lesion appearance, with smooth contours (Moving image 3, Figure 1A’, Figure 1B’). OCT imaging was repeated, demonstrating a complete healing of the large rupture cavity with all the hallmarks of the reparative process (Moving image 4, Figure 1C’-Figure 1H’): 1) re-established fibrous cap integrity and smooth vessel lumen profile; 2) thickening of the fibrous cap and reduction of lipid burden (i.e., transformation of TCFA into thick-cap fibroatheroma [ThCFA]); 3) replacement of the “empty” cavity with new signal-poor, low-backscattering, low-attenuating and heterogeneous tissue with poorly defined borders; 4) initial calcification of the plaque; 5) heterogeneous signal-rich layers with distinct optical signal intensity (a layered, “onion-like” pattern); and 6) mild relative lumen narrowing (MLA at the rupture site: 6.9 mm2). Based on these findings, the lesion was left untreated. At 6-month clinical follow-up, the patient was asymptomatic and no adverse events occurred.
Atherosclerotic plaque healing is a dynamic process which develops after plaque rupture or erosion, consisting of 3 main overlapping phases: 1) thrombus lysis, which prevents lasting occlusive thrombus formation in patients with an efficient endogenous fibrinolytic system; 2) healing tissue formation, caused by the proliferative response of local plaque smooth muscle cells and homing of blood progenitors; and finally, 3) plaque re-endothelialisation, which restores the vessel wall integrity1. This process, when effective, may protect the patient from the occurrence of acute coronary syndrome1. On the other hand, multiple cycles of disruption/thrombosis and healing may lead to stepwise, silent lumen loss with the potential risk of higher revascularisation rates2. Although it is well known from previous studies using different imaging modalities that some plaque ruptures can heal over time345, to the best of our knowledge, this is the first demonstration of complete healing of a large, ruptured plaque using serial OCT imaging, which incorporates all the major typical OCT findings of the healing process.
Conflict of interest statement
R. Vergallo, C. Aurigemma and E. Romagnoli received speaker fees from Abbott Vascular, and Terumo. F. Burzotta and C. Trani received speaker fees from Abbott Vascular, Abiomed, Medtronic, and Terumo. F. Crea received speaker fees from Amgen, AstraZeneca, Servier, BMS, and other from GlyCardial Diagnostics. The other author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline coronary angiogram showing a focal, complex lesion at the distal segment of the right coronary artery (RCA).
Moving image 2. Baseline optical coherence tomography (OCT) imaging showing a ruptured thin-cap fibroatheroma at the distal segment of the RCA.
Moving image 3. Follow-up RCA angiogram showing an improvement of the lesion at the distal segment with smooth contours after 18 months.
Moving image 4. Follow-up OCT imaging of the distal RCA showing a complete healing of the large rupture cavity after 18 months.