In chronic coronary syndromes, revascularisation of coronary atherosclerotic lesions has two aims: symptomatic improvement on one hand and avoiding future acute coronary events on the other1. For a long time, “ischaemia” has been assumed to constitute the differentiating factor: stenoses associated with stress-induced ischaemia would benefit from revascularisation both regarding symptoms, such as angina, and also regarding prognosis, with a reduction of future acute coronary events and subsequent mortality. All the same, it is widely realised that acute coronary syndromes (ACS) can also result from the rupture of lesions that are not significantly stenotic and, hence, not associated with ischaemia. In fact, since “mild” coronary atherosclerotic lesions are substantially more prevalent in the general population than “high-grade” coronary stenoses, the majority of ACS are caused by the rupture of coronary plaques which, on angiography, display luminal stenoses of less than 50%2.
The “hunt” for vulnerable coronary atherosclerotic plaque – a coronary atherosclerotic lesion that is likely to rupture with subsequent thrombosis and clinical manifestation as an acute coronary syndrome – is intensive, has been going on for many years, and has so far not led to the identification of a single clear parameter (or combination of parameters) that would be highly predictive of future events. In fact, two major approaches have been followed, on one hand the identification of lesions that cause ischaemia, and on the other, the identification of certain types of plaque anatomy and composition that would increase the likelihood of plaque rupture.
A landmark study in this field was the PROSPECT study, published in 20113. The investigators, led by G. Stone, performed coronary angiography and three-vessel intravascular ultrasound (IVUS) in 697 ACS patients. In particular, they investigated the characteristics of non-culprit lesions that could cause a second ACS in subsequent years. The PROSPECT study indeed confirmed that the average degree of luminal stenosis of non-culprit coronary lesions resulting in a second ACS during the subsequent 3-year period was only 32%. However, IVUS also allowed the identification of a plaque burden (cross-sectional vessel area with plaque as a fraction of the entire cross-sectional vessel area at the site of maximum luminal stenosis) ≥70%, a minimal luminal area ≤4.0 mm², and lesion classification as “thin-cap fibroatheroma” on radiofrequency IVUS as independent predictors of future ACS. The most predictive single parameter was plaque burden ≥70%, with an adjusted hazard ratio (HR) of 5.3 (95% confidence interval [CI]: 2.51-10.11). In subsequent analyses of the PROSPECT study, proximal location, large vessel size, and lack of calcium were also identified as predictors of future ACS4, and a similar trial, PROSPECT II, confirmed large plaque burden, along with high lipid content, as strong predictors of subsequent events5. This strongly suggests that plaque morphology is at least as important as, if not more important than, luminal obstruction for identifying plaques at particularly high risk for future events.
A similar approach has been taken for many studies performed by coronary computed tomography (CT) angiography (CTA). CTA allows operators to visualise atherosclerotic plaque, both stenotic and non-stenotic, and its non-invasive nature opens a window to the study of large cohorts. By following such cohorts and determining the incidence of acute coronary syndromes, lesion characteristics and their association with future events can be studied. Several anatomic and compositional plaque characteristics have been identified which increase the risk for downstream ACS. They prominently include the two closely related factors “positive remodelling” and “plaque burden”, but also low CT attenuation (suggesting a more lipid-rich composition of the plaque or a larger necrotic core), and lack of severe calcification67891011 – all of which serve as confirmation, in stable patients, of the parameters that the PROSPECT study had highlighted in patients with ACS. Other morphologic parameters have also been identified as predictive of future coronary events. They include the so-called “napkin-ring sign”12, which is poorly defined but likely a marker of large plaques with a sizeable low-density necrotic core, and even CT attenuation of the fatty epicardial tissue that surrounds the respective coronary lesion131415.
There are two important caveats around the study of coronary atherosclerotic plaque and morphologic plaque characteristics and their potential use of markers for future cardiovascular events. First, coronary plaque is a frequent finding. The recent SCAPIS trial showed that 42% of a Swedish population cohort, comprising 25,182 men and women aged 50 to 65 years, had detectable atherosclerotic plaque on coronary CTA16. And while lesions with “vulnerable” characteristics have a higher risk of future coronary events than lesions without “vulnerable” characteristics, this does not mean that all plaque that appears “vulnerable” will invariably lead to a future ACS; on the contrary, in an analysis of the SCOT-HEART Trial, the event risk for individuals with “vulnerable” plaque detected on CT was 3 times higher than for patients without, yet 96% of patients with “vulnerable” plaque detected did not have an event in the subsequent three years17. Hence, most morphologically “vulnerable” lesions will not lead to an acute coronary syndrome when followed for several years. Second, even while morphologic plaque features have prognostic relevance, the degree of stenosis remains a prominent prognostic marker, independent of plaque composition. In fact, Lee et al identified the “pressure drop” across the lesions, determined by simulated fractional flow reserve (FFR), as more prognostic for future coronary events than any morphologic plaque criteria18.
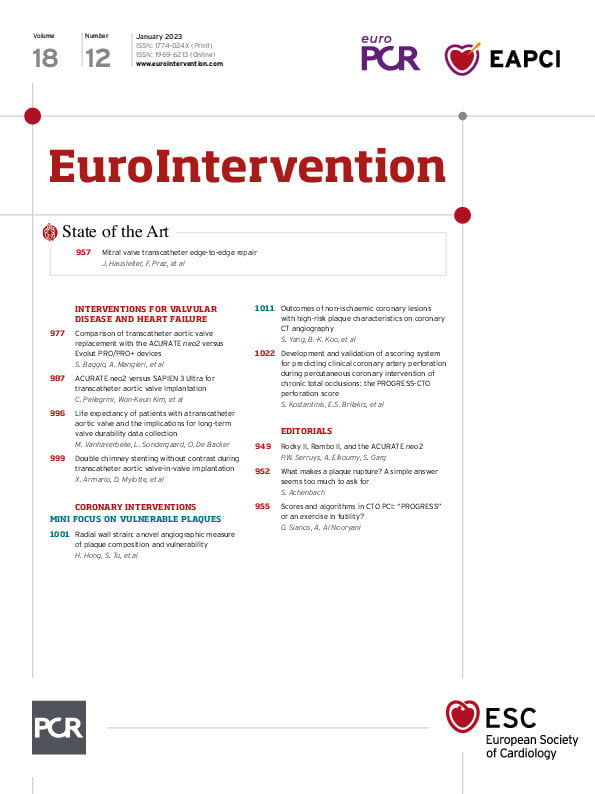
In this issue of EuroIntervention, Yang et al publish the results of an impressive trial based on a group of 458 patients who underwent invasive angiography with FFR measurements in 697 vessels following coronary CTA19. Revascularisation, guided by FFR, was performed in 25.8% of the 697 coronary arteries. During follow-up, vessel-specific ischaemic events (cardiac death, myocardial infarction, or revascularisation) occurred in 36 patients (8%). This offered the opportunity to study plaque characteristics and their associated event risk in lesions which, based on FFR, did not undergo revascularisation. The authors report that only lesions which were positive both for “quantitative” (geometric) features of plaque vulnerability (i.e., plaque burden ≥70% or MLA <3.3 mm²) and for “qualitative” (compositional) features of vulnerability (i.e., low CT attenuation or positive remodelling) had a significantly increased event risk as compared to lesions without any such features (HR 8.4, 95% CI: 2.9-24.4). Percutaneous coronary intervention (PCI) was associated with a reduced risk of events in patients with both positive “quantitative” and “qualitative” plaque features, even if FFR was between 0.81 to 0.90, but not if FFR was>0.90.
The authors deserve congratulations for their meticulous, state-of-the-art analysis of their thoroughly characterised cohort. Limitations of the trial clearly include the small number of events, the retrospective and observational nature with possible confounders, and the fact that the division between “quantitative” and “qualitative” plaque characteristics is somewhat arbitrary. We should also not forget that these were obviously selected patients who went on to angiography after CT, which makes the cohort a higher-risk cohort than an arbitrary population sample. The results can, therefore, not be applied to a “screening” situation. Yet, some conclusions can be drawn: for example, there is a clear association of vulnerable plaque characteristics with FFR (43% of lesions treated by PCI, but only 12% of lesions not treated by FFR, had high-risk plaque features). Also, the risk that goes along with single markers of “plaque vulnerability” is not very high – only in combination did they achieve significance in this cohort of several hundred patients. And one of the authors’ analyses seems to suggest that lesions with a combination of vulnerable characteristics potentially benefit from PCI even if FFR is between 0.81 and 0.90 (but not if FFR is above 0.90). Once again, we need to alert ourselves to the fact that all of these conclusions are based on a relatively small number of events and to some degree are subject to the play of chance. However, in the context of all previous studies, they add to a picture that is becoming increasingly obvious: there is, unfortunately no easy answer to what makes a plaque prone to cause acute coronary events. Some features of plaque morphology and compositional characteristics may make a plaque vulnerable, but so does the presence of severe luminal stenosis and a large pressure gradient across the lesion. While most lesions will remain stable, forces inside the plaque, as well as forces acting from the outside, e.g., through large differences in regional wall shear stress2021, may “tip the scale” and lead to plaque rupture and subsequent vessel thrombosis. There is no single decisive parameter that determines stability or instability, and, hence, the fate of a coronary atherosclerotic plaque. As is so often the case, a simple answer is too much to ask for.
Conflict of interest statement
The author has no conflicts of interest to declare.