The goal of investigations to risk-stratify individual coronary plaques over the past few decades has been to identify the so-called “vulnerable plaque”, i.e., a high-risk plaque on a trajectory towards plaque destabilisation and precipitation of a new clinical event, so that pre-emptive interventions could be utilised to interrupt that trajectory and avert the adverse event. Initial efforts focused on anatomic characterisation of the plaque, but prognostication based on plaque anatomy features has consistently been inadequate to influence clinical decision making1,2,3,4. Most plaques, including ostensibly high-risk plaques based on plaque anatomy characteristics alone, remain quiescent and do not destabilise and cause a new event. Investigations have consequently focused on complementary haemodynamic/biomechanical forces that may influence plaque natural history, leading to incremental changes in plaque size, shape, or constituents, that may culminate in destabilisation. Local shear stress (synonyms wall shear stress [WSS] or endothelial shear stress [ESS]) along the tortuous course of a coronary artery, at bifurcations, and upstream and downstream from partially obstructing plaque, has been most extensively investigated, but other important biomechanical metrics that may influence plaque behaviour have recently been studied, including plaque structural stress5 and axial plaque stress6 (Figure 1). There are preliminary clinical reports that a combination of plaque anatomic characteristics and associated haemodynamic/biomechanical forces may indeed provide clinically relevant, synergistic prognostication both for plaque progression2,7 and, perhaps even more importantly, for plaque destabilisation and clinical events8,9,10.
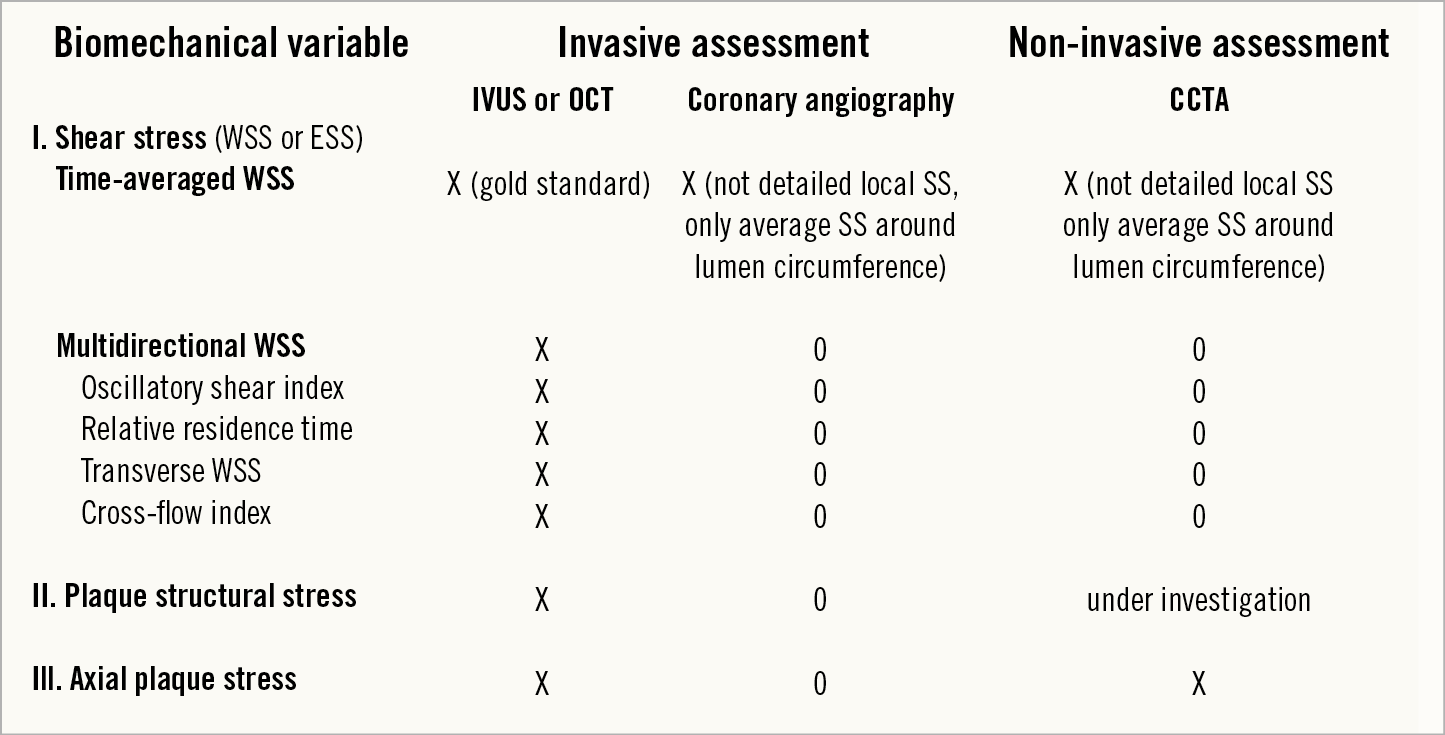
Figure 1. Current biomechanical assessment of intracoronary haemodynamics and plaque behaviour.
The shear stress metric most utilised to assess plaque behaviour and outcomes has been either shear stress as a time snapshot computed through a steady-state simulation of flow at a phase of the cardiac cycle, or the time-averaged WSS (TAWSS) computed through phasic simulation of flow and averaging over a cardiac cycle. The calculated value of TAWSS using phasic flow is in close quantitative agreement with the ESS results obtained assuming steady flow11. While average flow within a coronary artery is heterogeneous and complex, the disturbed flow patterns throughout the cardiac cycle are even more complex and multidirectional. The multidirectional WSS metrics include oscillatory shear index (OSI) and cross-flow index (CFI), which measure the change in direction of WSS over a cardiac cycle, transverse wall shear stress (transWSS) which is the WSS component perpendicular to both the surface and TAWSS vector, and relative residence time (RRT) which is a parameter formed by combining TAWSS and OSI.
In this issue of EuroIntervention, Kok et al provide results evaluating both TAWSS and multidirectional WSS metrics in the left anterior descending coronary artery in 20 patients with stable coronary artery disease (CAD) investigated at baseline and after six months of follow-up, using virtual histology intravascular ultrasound (VH-IVUS) to assess plaque composition12.
They observed that plaque progression was most influenced by exposure to baseline low TAWSS and co-localisation of low multidirectional WSS. Multidirectional WSS metrics were primarily involved in altering plaque composition rather than plaque size, suggesting that plaque vulnerability was increased. High TAWSS showed change in characteristics of plaque vulnerability, with modest incremental impact of multidirectional WSS.
The study contributes valuable new insights concerning the impact of multidirectional WSS on coronary plaque and will certainly motivate other investigators to pursue these more complex intracoronary flow patterns. The study is limited, as the investigators acknowledge, by investigating a small number of stable CAD patients with brief follow-up, and all patients were treated with high-dose atorvastatin. As the investigators also acknowledge, the characterisation of plaque “vulnerability” based on VH-IVUS tissue features may be incomplete. It will be important to confirm that the changes in ostensible “plaque vulnerability” have clinical significance based on actual destabilisation leading to new clinical events rather than tissue characterisation alone.
It would also be useful to compare the value of the different multidirectional WSS metrics, since they share many similar features related to the disturbed local flow patterns and determine whether there is incremental benefit of using one or a combination of these metrics compared to using TAWSS or its steady-state analogue, ESS, alone. How independent are these variables, or are they primarily describing similar phenomena related to similar flow patterns? What is the degree of correlation among the multidirectional WSS metrics? Another critical aspect for future research is the effect of different magnitudes of “high” WSS on plaque behaviour. “Increased” WSS has often been found to be atheroprotective, but the WSS values investigated in these studies have often not been as elevated as the very high values observed clinically at the throat of a tight luminal obstruction. The consequences of these “superhigh” WSS values may be qualitatively very different and more detrimental than physiologic “high” WSS.
The field of risk stratification of individual coronary plaques is evolving rapidly as new and more refined metrics of factors impacting on vascular biology/plaque behaviour are identified and methodologies are developed to measure these metrics and compare their prognostic significance. Much of the focus in the past has been on evaluating changes of plaque outcome characteristics such as plaque size, burden, shape, and constituents, but it is particularly important going forward to focus on the actual process of plaque destabilisation and clinical events. Most previous prognostic studies of plaque natural history investigating the effect of baseline haemodynamic/biomechanical plaque characteristics have been inefficient for studying WSS since those natural history studies were designed for other purposes and, consequently, the imaging data sets were often inadequate for WSS computations. It will be invaluable in the future to focus our haemodynamic/biomechanical investigations on predicting plaque destabilisation and new clinical events, since only those “hard” prognostic outcomes will provide the crucial justification necessary to consider pre-emptive intervention for the true “vulnerable” plaque.
Conflict of interest statement
The authors have no conflicts of interest to declare.