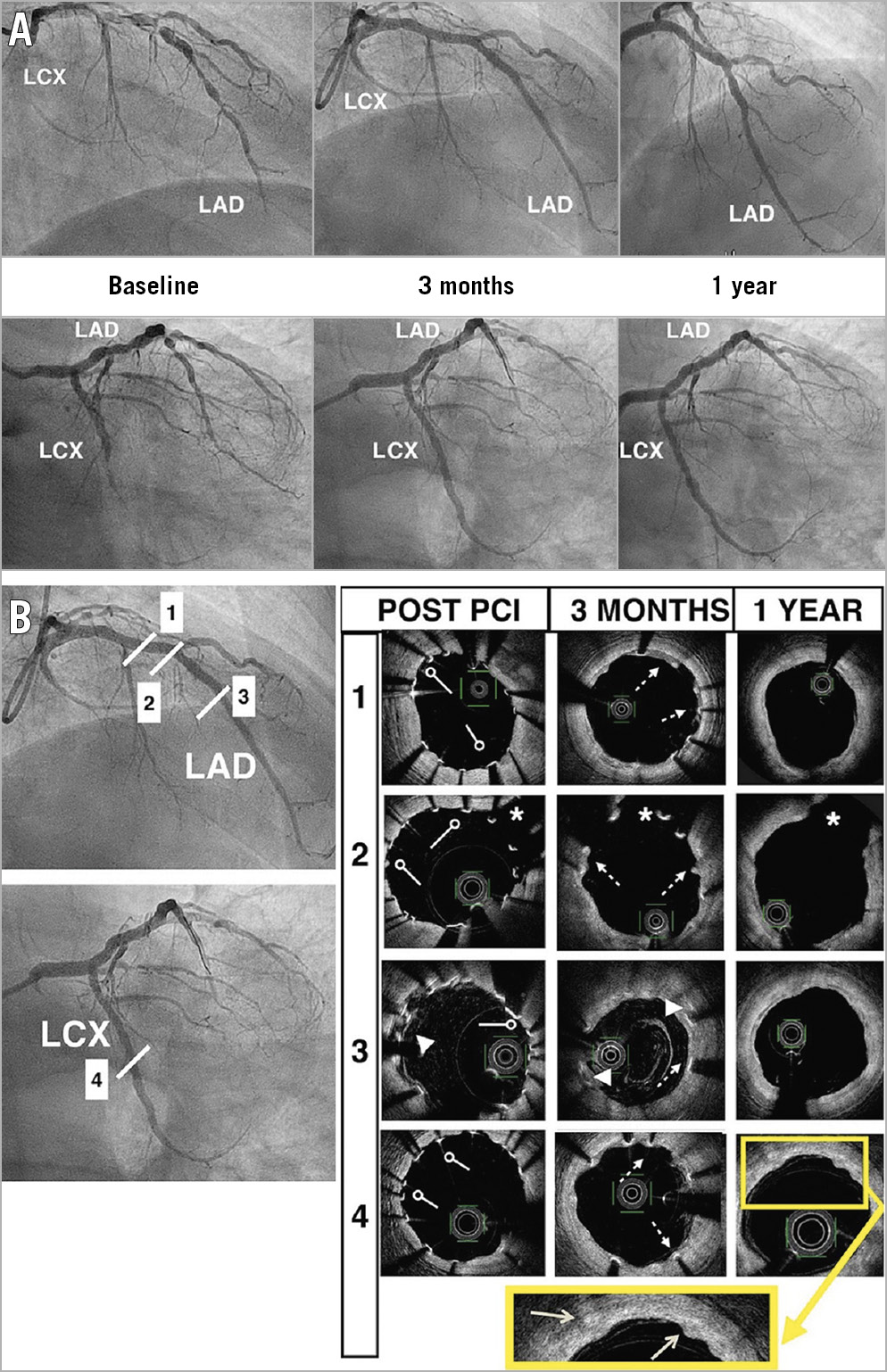
Figure 1. Angiographic and OCT images over time. A) Coronary angiography showing coronary artery disease in the LAD and LCX at baseline and at three months with good result of implanted scaffolds, and at one-year follow-up, with no evidence of restenosis. B) Optical coherence tomography (OCT) post PCI, at three-month and one-year follow-up. Cross-sections are divided into proximal LAD (1), LAD bifurcated with diagonal (2), mid LAD overlapping scaffold (3) and LCX (4). At baseline circle arrowheads indicate correct apposition of the struts. At three months, dotted line arrows indicate partial covering of the majority of the struts and arrowheads indicate two layers of struts in overlapping cross-sections. At one year, solid arrows (magnified image) indicate the last remnants of the magnesium backbone degradation process without evidence of Magmaris scaffold struts. Asterisk (*): diagonal lumen. LAD: left anterior descending; LCX: left circumflex
The bioresorbable sirolimus-eluting magnesium scaffold (Magmaris; Biotronik AG, Bülach, Switzerland) has a metallic magnesium skeleton with a thickness/width of 150 µm/150 µm1. The absorption time is fast: 95% will be absorbed in the first twelve months2.
A report on successful bifurcation lesion treatment with the Magmaris has been published previously3; however, there is little literature on complex percutaneous coronary intervention (PCI), such as coronary dissections, with this device4, and no previous reports in chronic total occlusion (CTO).
We present the case of a 65-year-old male with an allergy to nickel, coronary disease of two vessels with multiple tandem lesions in the left anterior descending (LAD) artery, and CTO in the left circumflex (LCX) artery. The patient was discussed by the Heart Team, who concluded that the diffuse vessel disease was not suitable for grafting. Coronary angiography (at baseline, three months post PCI and at one-year follow-up) is shown in Figure 1A.
We treated the LAD with sequential and overlapping Magmaris scaffolds, implanting from the distal LAD to the bifurcation with the diagonal, which was treated with a two-scaffold technique – the first implanted in the diagonal branch and the second one in the mid LAD. Total occlusion of the LCX was also treated with the Magmaris.
The final result was confirmed by optical coherence tomography (OCT), post PCI, at three months and at one-year follow-up (Figure 1B). Post-PCI OCT showed 2.1% malapposed struts within Magmaris scaffolds. At three months, we reviewed strut coverage with 82% endothelialisation. Post-PCI OCT indicated correct apposition of the struts (circle arrowheads). Three-month OCT showed partial covering of the majority of the struts (dotted line arrows). Twelve-month OCT showed the remnants of the magnesium backbone degradation process (solid arrows) without evidence of Magmaris scaffold struts. Use of the Magmaris scaffold is becoming a real and safe choice in this kind of patient.
Conflict of interest statement
The authors have no conflicts of interest to declare.