Introduction
The risk of coronary obstruction after transcatheter aortic valve implantation (TAVI) is high in cases where a deflected failing aortic valve leaflet is positioned in close proximity to a coronary ostium1,2. Bioprosthetic or native Aortic Scallop Intentional Laceration to prevent Iatrogenic Coronary Artery obstruction (BASILICA) is a novel technique in which splitting of such an aortic valve leaflet can reduce that risk3. Although multidetector computed tomography (MDCT) and aortic root angiography are the primary imaging modalities to evaluate the anatomic relationship between the aortic valve and the coronary ostia to determine that risk, no systematic classification exists to determine if coronary obstruction risk is elevated and whether preventive techniques, such as BASILICA, could be of benefit. The Valve-in-Valve International Data (VIVID) registry investigators convened in Paris, France, in May 2019 in response to a need for standardisation. We propose here a simplified classification that may guide operators on the risk of coronary obstruction during TAVI and the possible need for BASILICA. Each coronary artery ostium would need to be evaluated, and subsequently classified, separately.
Methods and results
VIVID CLASSIFICATION
The key consideration in this classification is the estimation of the most upper and lateral location of the deflected failed valve leaflet position after TAVI (Figure 1). In many cases, we can predict the location of this top deflection by defining the plane with the top of the commissures in native valves or the top of the posts of the failed stented bioprosthetic valve, assuming that the deflected leaflet would not rise significantly above that plane. In some failed bioprosthetic valves these leaflets can extend towards the top of the posts (e.g., Mitroflow; Sorin Group USA Inc., Arvada, CO, USA), while in others it would be relatively low (e.g., Epic™; Abbott Vascular, Santa Clara, CA, USA). Although data from the VIVID registry reveal that a virtual transcatheter heart valve to coronary ostium (VTC) distance of <4 mm is associated with high risk of coronary obstruction with high sensitivity and specificity (85% and 89%, respectively), the actual threshold that will put coronary flow at risk also depends on the bulkiness of the deflected leaflet, the magnitude of coronary flow (dominancy, supply by bypass vessels, etc.) and the actual lateral leaflet deflection, all of which can occasionally be difficult to predict1. There are other conditions in which exaggerated focus on VTC/virtual transcatheter heart valve to sinotubular junction (VTSTJ) may lead to overestimation of the risk of obstruction.
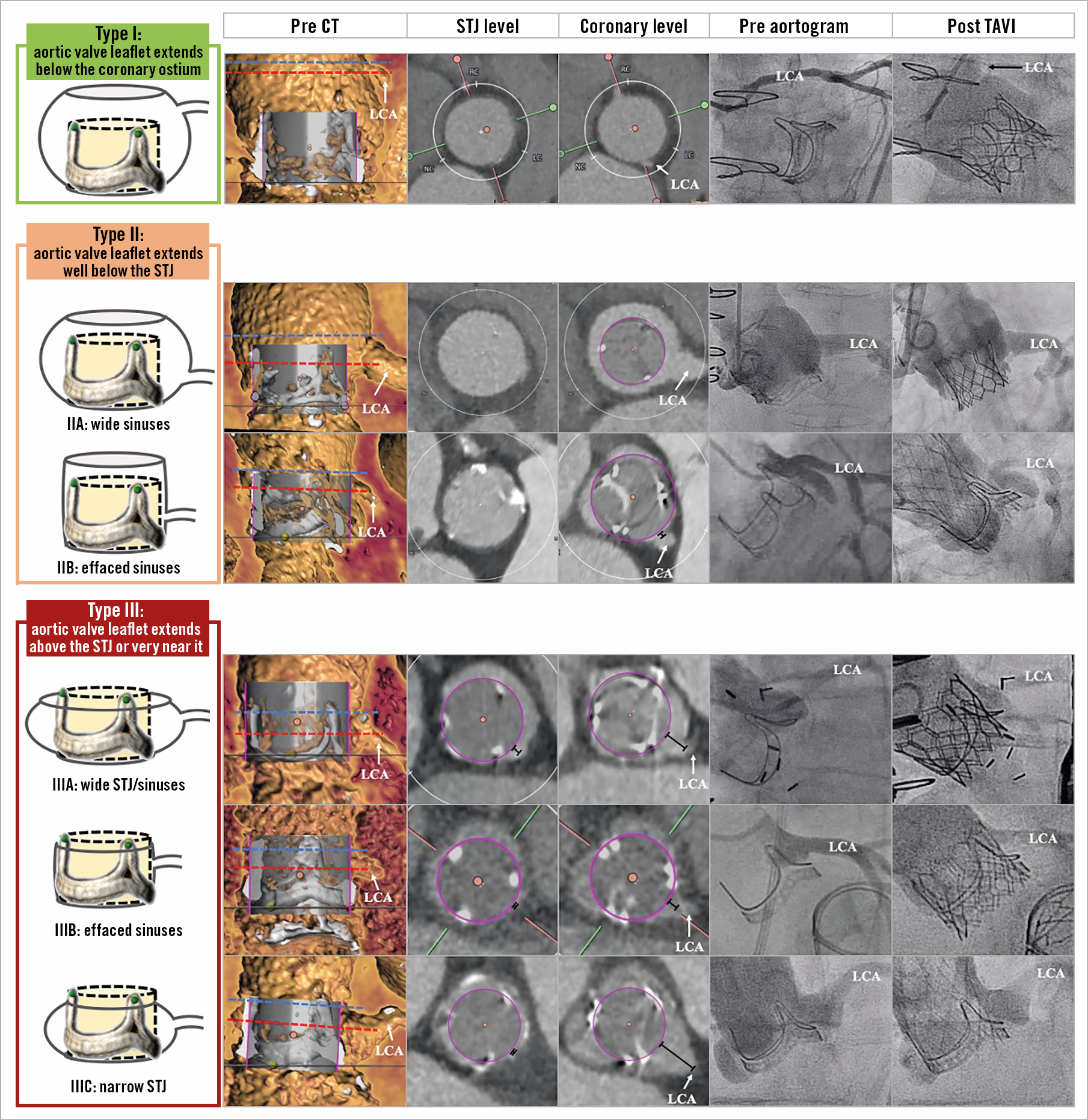
Figure 1. VIVID classification. Anatomic classification of the aortic root and valve leaflet position to determine the possible need for BASILICA during transcatheter aortic valve implantation (TAVI). Each coronary artery ostium would need to be classified separately.
Discussion
Figure 1 illustrates different types of aortic root anatomy. Type I anatomy consists of a failed valve leaflet that extends fully below the coronary ostia plane and therefore the risk of coronary obstruction is close to none; no BASILICA is necessary and conventional TAVI can be performed safely. In Type II anatomy, the failed valve leaflet may extend above part of the coronary ostium, but not near the STJ.
In Type II, if the sinus has large capacity it may accommodate the deflected failed valve leaflet without reducing blood flow to the coronary artery and the risk of obstruction would be low (Type IIA). On the other hand, if the sinuses are effaced (VTC2 distance is <4 mm) (Type IIB), then BASILICA should be considered. In rare scenarios, in which the failed valve leaflet deflects minimally below the level of the STJ, the diagonal and vertical distances between the highest and most lateral leaflet deflection towards the STJ should be measured as well and, in cases of a short distance (<2.5-3.5 mm), BASILICA should be considered.
Type III anatomy represents the most complex anatomy, in which the failed valve leaflet can extend either above the STJ plane, or below the STJ plane but very near it (<2 mm). Many cases of surgical valves with Type III anatomy would be at risk of coronary obstruction. If the VTC is <4 mm (Type IIIB), then BASILICA is recommended. If the VTC is ≥4 mm, then there is a need to examine whether obstruction can occur in the inflow to the sinus (the STJ level). If the VTSTJ distance is sufficient to allow diastolic flow to the coronaries (Type IIIA), then conventional TAVI can be performed with low risk of obstruction. There is currently no scientifically derived threshold that defines what should be considered too narrow a VTSTJ. That cut-off will probably depend on the size of the post-TAVI STJ residual non-obstructed crescent area and magnitude of the coronary blood supply. If the VTSTJ distance is short (Type IIIC), then BASILICA should be considered. A VTSTJ <2.5 mm is widely considered to be high risk in Type III anatomy, while a VTSTJ between 2.5 and 3.5 mm is considered a borderline condition.
Limitations
The current classification is limited by lack of clinical validation. We are currently retrospectively and prospectively evaluating cases that needed BASILICA to validate this model and hope that the data will provide more specific understanding of cases at risk of coronary obstruction and BASILICA-favourable anatomy.
Conclusion
Based on the above classification, we outline a treatment algorithm for identifying which root anatomy may benefit from BASILICA (Figure 2). Based on the proposed algorithm, in Type I anatomy there is no need to measure the VTC/VTSTJ and in Type II there is no need to measure the VTSTJ, since in these anatomies even short distances would not result in obstruction by conventional mechanism. We believe that our classification would provide an unified terminology of aortic roots that would be beneficial for patient evaluation and could help to guide whether the BASILICA technique should be performed concomitantly during TAVI.
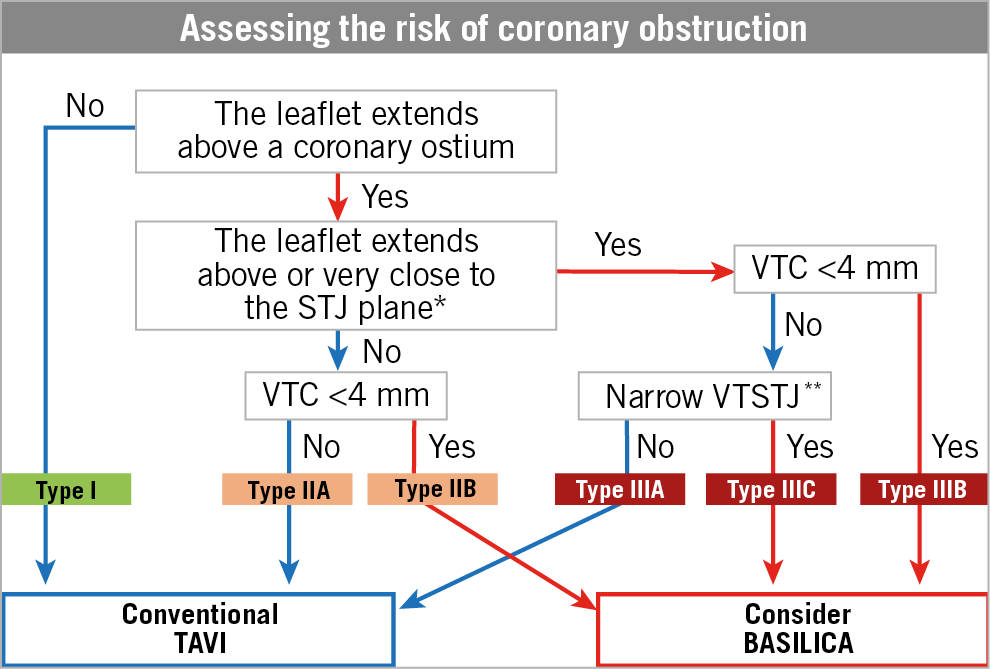
Figure 2. Proposed algorithm to determine aortic root anatomy and indication for BASILICA. *Either above, at, or up to 2 mm below the plane of the STJ. **The threshold to define a narrow VTSTJ is unknown and is currently considered to be <2.5-3.5 mm (<2.5 mm is a high-risk condition and 2.5-3.5 mm is a borderline condition).
|
Impact on daily practice This report describes a novel anatomical classification of aortic root types according to the risk of coronary obstruction during TAVI. This classification scheme would help to unify terminology and guide operators on how to evaluate the risk of coronary obstruction and the need to utilise prevention techniques, such as BASILICA. |
Conflict of interest statement
G. Tang is a physician proctor for Medtronic and a consultant for Medtronic, Abbott Structural Heart and W. L. Gore & Associates. D. Dvir is a consultant to Edwards Lifesciences, Medtronic, Gore, Jena, and Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.