Abstract
Aims: The aim of this study was to evaluate the feasibility, efficacy and safety of the bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction (BASILICA) technique during transcatheter aortic valve implantation (TAVI) in an initial cohort at a single European centre.
Methods and results: Between August 2018 and March 2020, BASILICA was attempted in 23 leaflets in 21 consecutive patients undergoing TAVI (age 78±6 years, 52% female). The index procedure was performed for 21 degenerated bioprosthetic leaflets (90%, 9.2±2.6 years after implantation) and two native leaflets (10%). BASILICA was performed for a single leaflet in 19 (90%) patients and for both leaflets in two (10%) patients. The median total procedure time was 82 (interquartile range [IQR] 70-131) minutes, and BASILICA time (sheath-in to laceration) was 45 (IQR 35-67) minutes. A cerebral embolic protection device was used in 20 (95%) patients. BASILICA was feasible in all but one patient (95%) and resulted in effective prevention of coronary obstruction in 19 patients (90%). One patient developed a non-flow-limiting ostial lesion after BASILICA and TAVI, and was treated by additional coronary stenting. No mortality or stroke was observed up to 30 days.
Conclusions: The feasibility, efficacy and safety of BASILICA in this early single-centre experience were consistent with the initial proof-of-concept reports. Further validation by ongoing multicentre registries remains warranted.
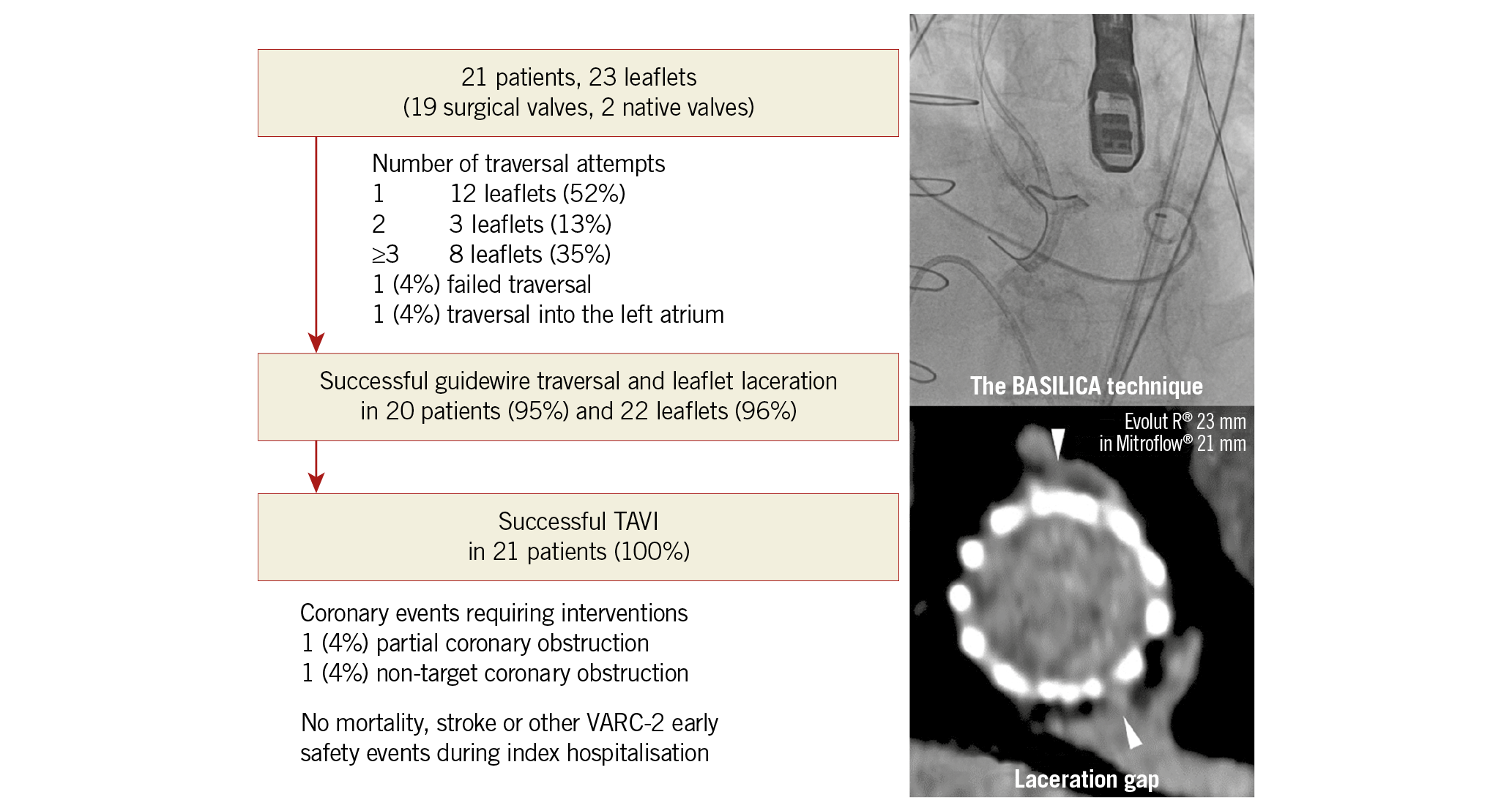
Visual summary. The Leipzig BASILICA experience.
Introduction
Iatrogenic coronary artery obstruction is a rare but potentially fatal complication of transcatheter aortic valve implantation (TAVI). Its incidence appears to be higher after valve-in-valve (ViV) procedures for degenerated surgical bioprostheses; it is highest after ViV for stentless valves and those with externally mounted leaflets1. Coronary obstruction is also a concern after ViV procedures for degenerated transcatheter valves, but its incidence and consequences in this setting remain poorly understood. Consequently, several imaging-based algorithms have been developed to predict the risk of coronary obstruction during TAVI and subsequently prevent its occurrence by either withholding TAVI or prophylactic coronary stenting2.
Recently, Khan et al described the therapeutic concept of bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction (BASILICA) during TAVI3, and reported its feasibility and safety in a small multicentre prospective trial4. This procedure aims at slicing the native or bioprosthetic aortic valve leaflet in front of the coronary artery at risk of obstruction using percutaneous electrosurgical techniques, resulting in leaflet splaying after TAVI and maintained coronary flow. In the multicentre BASILICA trial, which was performed exclusively in the USA by the pioneers of this technique, none of the 30 included patients experienced coronary obstruction and the technical success rate was 93%4.
The BASILICA procedure is still in its infancy and requires several complex interventional steps. In addition, the feasibility, safety and efficacy of this technique outside of its country of origin remain unreported. Therefore, we sought to describe the first consecutive series of patients treated with BASILICA at a single high-volume European centre.
Methods
STUDY POPULATION
All patients undergoing the BASILICA procedure at the Leipzig Heart Center of the University of Leipzig were prospectively included in a dedicated institutional database. Between August 2018 and March 2020 (total number of TAVI = 1,507), the technique was attempted in 23 high-risk leaflets in 21 patients (1.4%). The indication for BASILICA was based on an elevated risk of direct leaflet-induced coronary obstruction (sinus deficiency) and/or leaflet tips extending above the sinotubular junction (STJ) with the risk of sinus sequestration based on preprocedural three-dimensional (3D) computed tomography (CT), as previously described2. Bicuspid aortic valves, valve thrombosis and infective endocarditis were carefully excluded using echocardiography and reconstructed CT images at enrolment.
The first four cases were proctored by an external expert (D. Dvir). Thereafter, an institutional Heart Team including an interventional cardiologist (M. Abdel-Wahab) and a cardiac surgeon (D. Holzhey) performed all procedures independently.
The study protocol conformed to the ethical guidelines of the 1964 Declaration of Helsinki and its later amendments. All patients provided written informed consent.
PREPROCEDURAL CT
Pre-evaluation using reconstructed CT images was performed to elucidate: 1) the relationship between valve leaflets and coronary ostia, 2) considerations for procedural feasibility, and 3) commissural alignment and coronary eccentricity5 (Figure 1). All the analyses were simulated on a 3D-imaging workstation (syngo.via®, version VB30A; Siemens, Munich, Germany). The precise description and CT evaluation for BASILICA were described recently by Lederman et al2,5. Briefly, an evaluation of the relationship between the virtually deflected leaflets and the coronary ostia and/or STJ after TAVI is performed initially (Figure 1A). If leaflet tips extend above the coronary ostia or the STJ, the distance between a virtual transcatheter heart valve (THV) and the coronary ostium at risk (VTC) or STJ (VTSTJ) is measured (Figure 1A). A coronary height <10 mm, a VTC <4 mm and a VTSTJ <2 mm were considered high-risk features for coronary obstruction2,4. For procedural guidance during BASILICA, the operator front and side views of the target cusp were identified (Figure 1B). In addition, the presence of misaligned bioprosthetic commissures and leaflet/cusp calcification that might interfere with guidewire traversal and leaflet laceration were identified (Figure 1C, Figure 1D). These measurements were performed by two investigators independently, and the final decision regarding whether or not to perform the procedure was made by the local Heart Team.
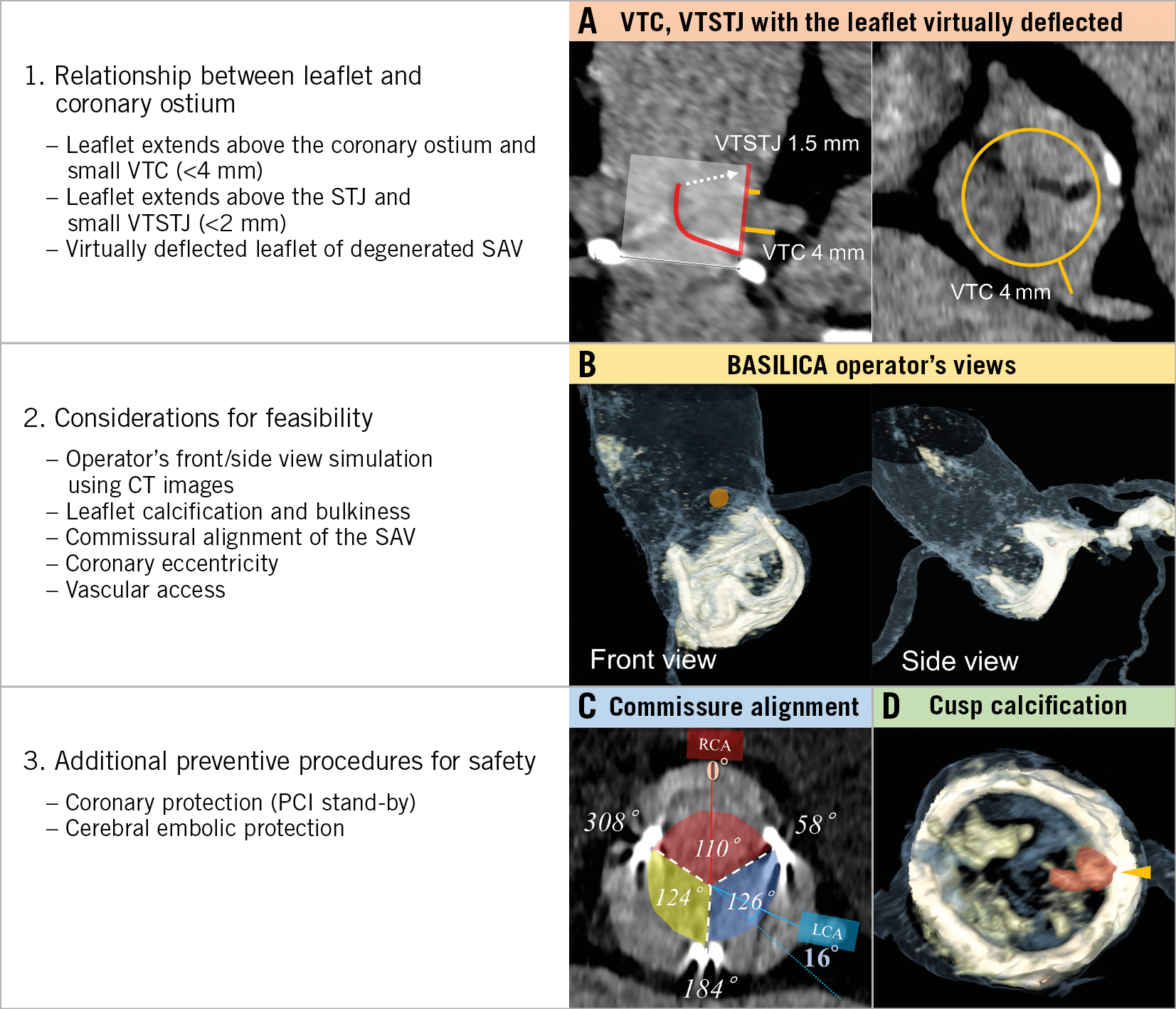
Figure 1. Risk assessment of TAVI-induced coronary obstruction and special considerations for a successful BASILICA procedure. CT: computed tomography; PCI: percutaneous coronary intervention; VTC: virtual transcatheter valve to coronary distance; SAV: surgical aortic valve; VTSTJ: virtual transcatheter valve to sinotubular junction distance
THE BASILICA PROCEDURE
Details of the BASILICA technique have been described elsewhere2,3,6. We performed the procedure under general anaesthesia using a bilateral femoral access (Figure 2A), and cerebral embolic protection with a SENTINEL™ dual filter system (Boston Scientific, Marlborough, MA, USA) was attempted in all cases. A special large-bore sheath that allows the insertion of multiple catheters without back-bleeding (DrySeal; W.L. Gore & Associates, Inc., Flagstaff, AZ, USA) was used in all procedures. The snare size was chosen according to the left ventricular outflow tract (LVOT) size, with a tendency for undersizing. Leaflet traversal and laceration were performed with an Astato XS 20/300 cm wire (Asahi Intecc, Aichi, Japan) insulated in a wire converter (PiggyBack®; Teleflex, Morrisville, NC, USA), and was guided by the predetermined fluoroscopic front and side views as well as transoesophageal echocardiography (TOE) (Figure 2B). The optimal traversal point was considered central on the nadir of the target leaflet. When the width of the native or bioprosthetic leaflet nadir was too narrow to manipulate the traversal system, the traversal point was modified to be higher than the nadir. Leaflet laceration was achieved by locally transmitted electricity generated by an electrosurgery system with guidewire tension by pulling on both guiding catheters (Figure 2C, Figure 2D). The THV was implanted immediately after leaflet laceration.
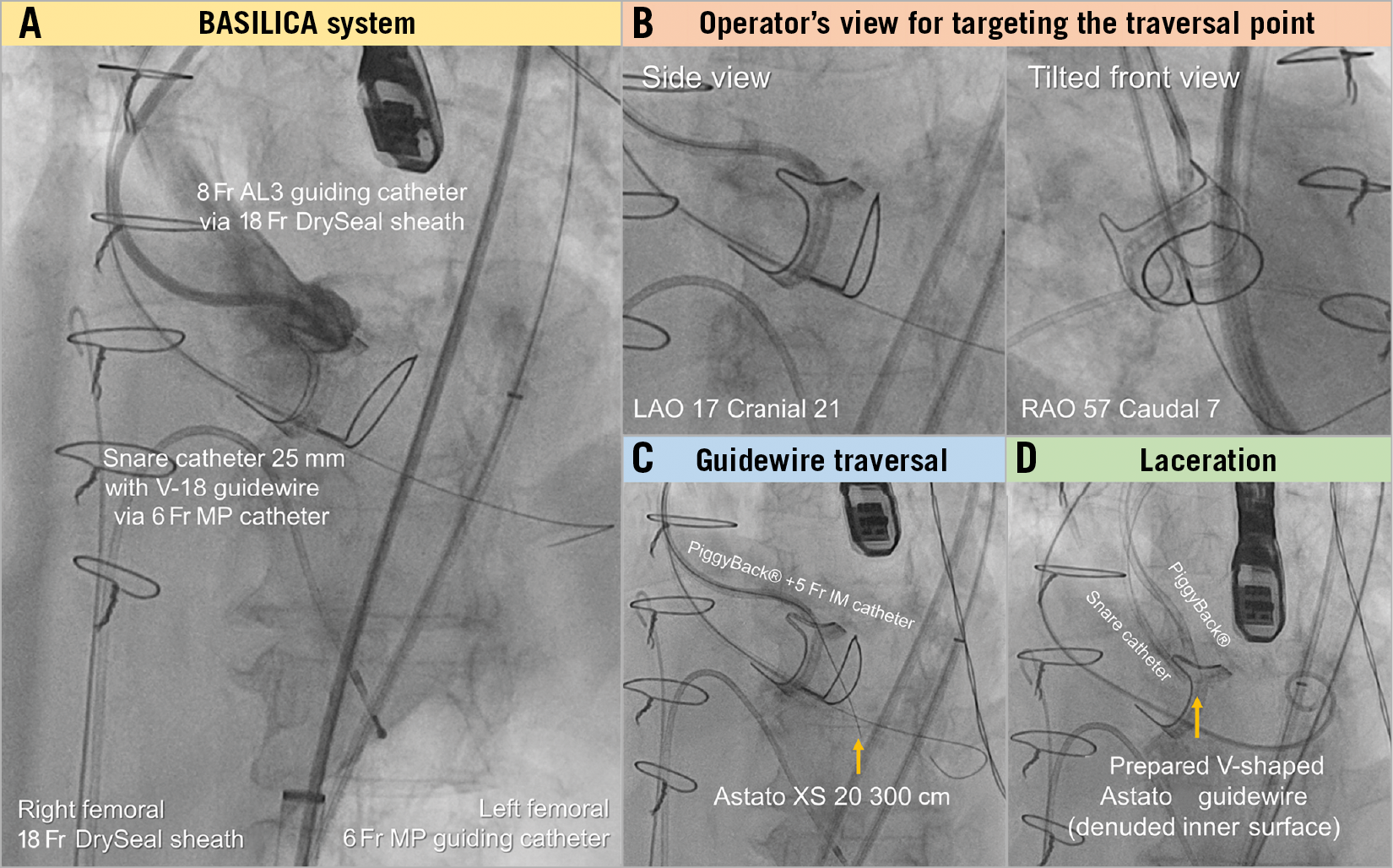
Figure 2. Steps of the BASILICA procedure. AL: Amplatz left; LAO: left anterior oblique; MP: multipurpose; RAO: right anterior oblique
Post-procedural management was in accordance with a standardised institutional protocol for patients undergoing TAVI. Bioprosthetic valve function was evaluated using transthoracic echocardiography before discharge. Patients were discharged on single antiplatelet therapy or oral anticoagulation if indicated. In addition, post-procedural CT evaluation was planned within 30 days from the index TAVI.
PRIMARY OUTCOMES
The primary outcome measures of this analysis were the feasibility, efficacy and safety of the BASILICA technique in this early single-centre experience. Feasibility was evaluated through the technical success of BASILICA, defined as successful leaflet traversal and laceration without injury to the surrounding structures and successful retrieval of the BASILICA system. Efficacy was defined through procedural success, defined as technical success, successful THV implantation, absence of coronary obstruction or intervention related to the target aortic valve leaflet, and no procedural mortality. Early safety was defined according to the updated Valve Academic Research Consortium-2 (VARC-2) criteria7.
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation or as median and interquartile range as appropriate. Categorical variables are expressed as counts and percentages. The correlation of preprocedural VTC and VTSTJ with the actual post-procedural CT measurements was analysed using Spearman’s rank correlation coefficient. To test the intra- and inter-observer agreements of CT measurements, VTC, VTSTJ and the actual observed distances were repeatedly measured by the same observer at least six weeks apart, and separately measured by another observer blinded to the initial measurements. Using these three data sets, the intraclass correlation coefficient was calculated for the absolute agreement. A two-tailed p-value of 0.05 was considered statistically significant. All statistical analyses were performed using SPSS, Version 21 (IBM Corp., Armonk, NY, USA).
Results
BASELINE CLINICAL AND ECHOCARDIOGRAPHIC CHARACTERISTICS
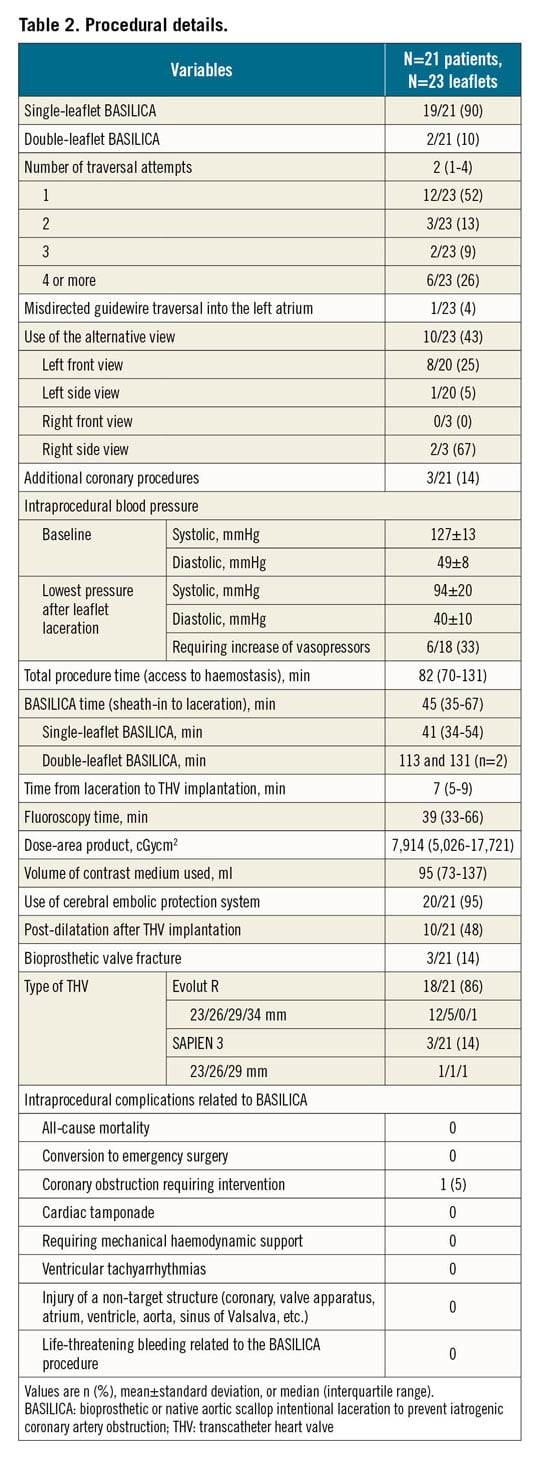
BASILICA was attempted in 23 leaflets in 21 consecutive patients (mean age 78±6 years, 52% female) between August 2018 and March 2020 (Supplementary Table 1). The index procedure was performed for 21 degenerated bioprosthetic leaflets (91%, 9.2±2.6 years after implantation) and two native leaflets (9%). Bioprosthetic valves were externally mounted stented valves in 12 patients (52%), internally mounted stented valves in 4 patients (17%), stentless bioprostheses in 2 patients (9%) and a self-expanding transcatheter valve in 1 patient (4%) (Table 1). The mode of aortic valve disease at the index TAVI with BASILICA was severe stenosis in 10 patients (48%), severe regurgitation in 7 (33%) and mixed aetiology in 4 (19%). The effective orifice area was 0.7±0.2 cm2, the peak gradient was 57±18 mmHg and the mean gradient was 34±11 mmHg.
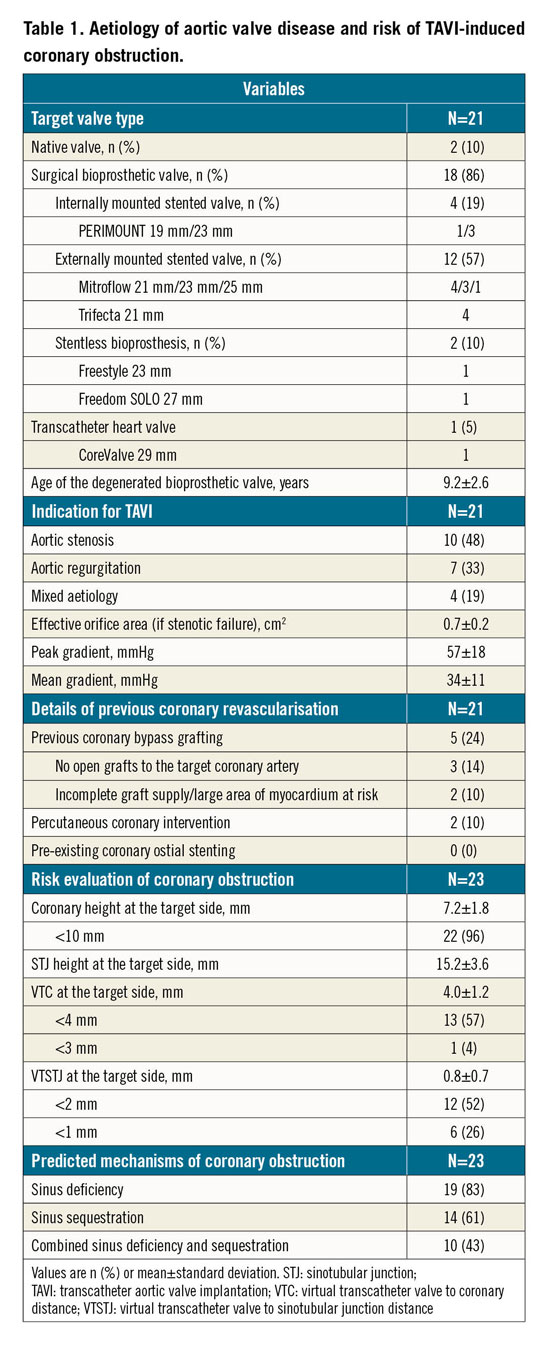
PREPROCEDURAL CT
In the pre-evaluation CT, all patients had at least one of the high-risk features of TAVI-related coronary obstruction, i.e., coronary height <10 mm (96%), VTC <4 mm (57%), and VTSTJ <2 mm (52%). One patient with a degenerated supra-annular self-expanding THV had a high risk of STJ obstruction by the deflected valve, and the feasibility of future coronary intervention for a previously stented ostial left anterior descending coronary artery was a concern after redo TAVI (Figure 3A-Figure 3C).
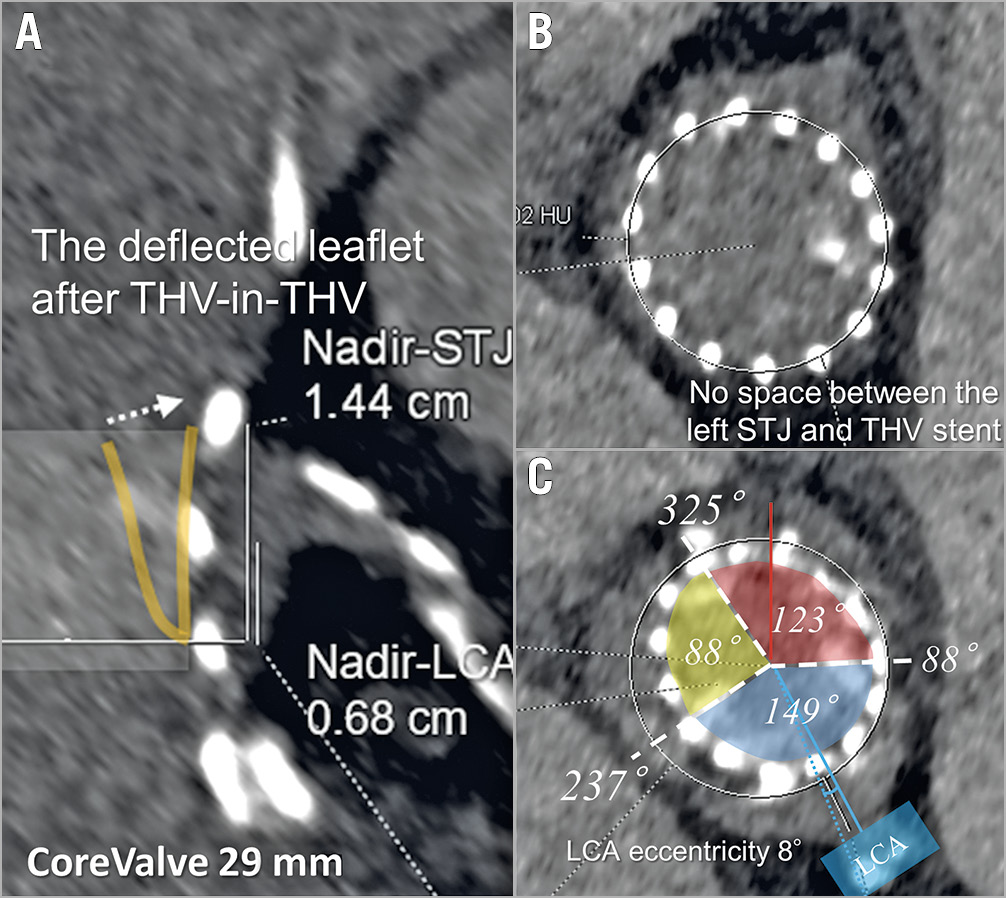
Figure 3. Assessment of future coronary re-access after valve-in-valve for a degenerated supra-annular self-expanding transcatheter heart valve. Expected leaflet deflection towards the sinotubular junction (A & B) and commissural orientation (C) are demonstrated on preprocedural computed tomography. LCA: left coronary artery; STJ: sinotubular junction; THV: transcatheter heart valve
The intraclass correlation coefficient of VTC and VTSTJ measurements on preprocedural CT was 0.91 and 0.77 for the intra-observer comparison, and 0.85 and 0.79 for the inter-observer comparison, respectively (p<0.0001 for all comparisons).
PROCEDURAL DETAILS
BASILICA was performed for a single leaflet in 19 patients (90%) and for two leaflets in two patients (10%) (Table 2). All procedures were performed under general anaesthesia and guided by fluoroscopy and TOE. The median total procedure time (from vascular puncture to haemostasis) was 82 (interquartile range [IQR] 70-131) minutes, and the median BASILICA procedure time (sheath-in to leaflet laceration) was 45 (IQR 35-67) minutes. A cerebral embolic protection device was used in 20 patients (95%), and macroscopic embolic debris was captured in all of them. Alternative fluoroscopic views were used in 10 leaflets (43%), mostly for the front view of the left coronary cusp (8 of 20 leaflets, 25%) and for the side view of the right coronary cusp (2 of 3 leaflets, 67%).
The median number of attempted guidewire traversals was 2 (IQR 1-4, range 1-9) until successful leaflet traversal (one attempt in 52%, two attempts in 13%, three attempts in 9%, and four or more attempts in 26%) (Table 2). There was one failed guidewire traversal, which was thought to be related to a combination of severe leaflet calcification (Figure 4) and severe peripheral tortuosity in the early phase of experience. In this case, coronary ostial stenting using the chimney technique was performed to mitigate the risk of coronary obstruction and there were no coronary or cerebrovascular events after TAVI. Another patient experienced a misdirected guidewire traversal into the left atrium, which was identified by both fluoroscopy and TOE. Successful traversal was achieved after changing the direction of the traversal system without relevant injury.
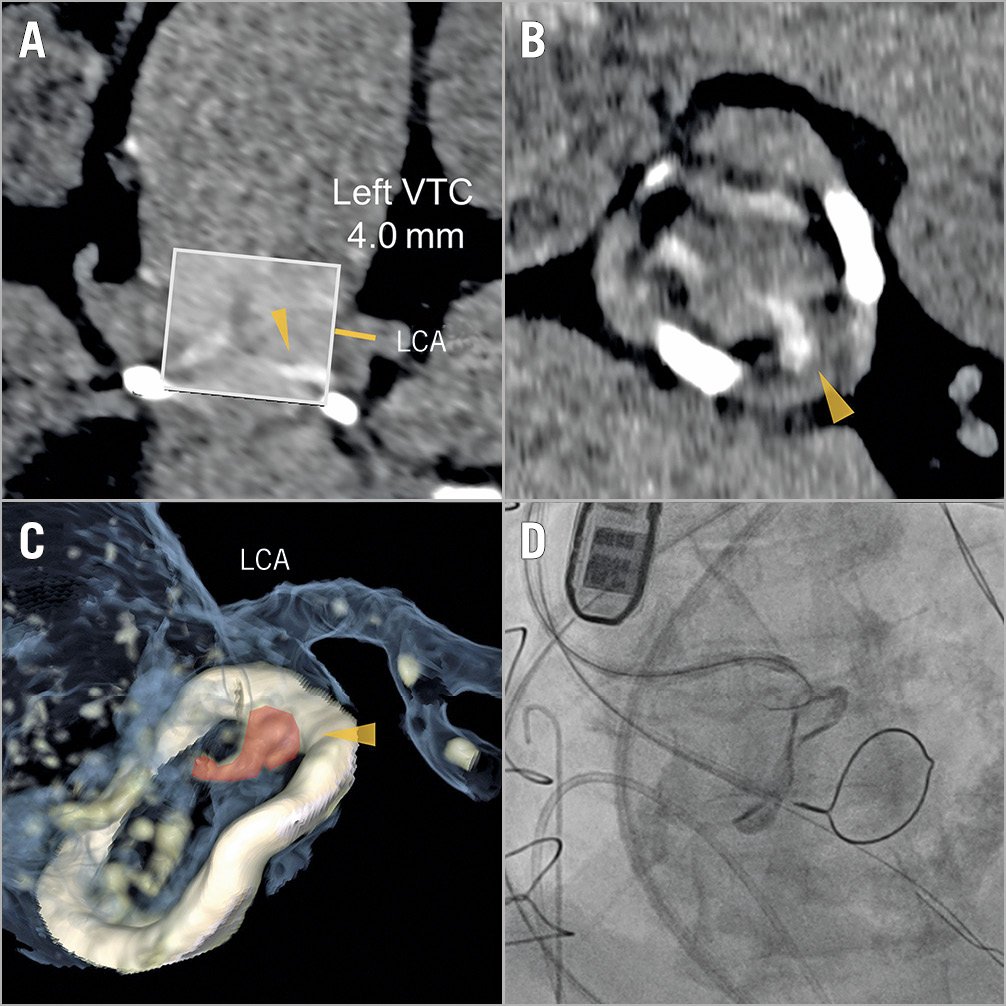
Figure 4. Failed guidewire traversal. Severe calcification of the target leaflet (A-C) eventually resulting in failed guidewire traversal (D).
Externalisation of the guidewire using snaring was achieved within five minutes in most patients (81%), and leaflet laceration was successfully performed in all patients with successful guidewire traversal (n=22). All THVs were successfully implanted immediately after leaflet laceration. No cardiac arrest or ventricular arrhythmias occurred, and none of the patients required mechanical circulatory support. On the other hand, six patients required vasopressor support between leaflet laceration and THV implantation (Table 2). These included the first four proctored patients. Thereafter, a low dose of norepinephrine was used prior to leaflet laceration in patients with a systolic blood pressure below 120 mmHg.
FEASIBILITY AND EFFICACY
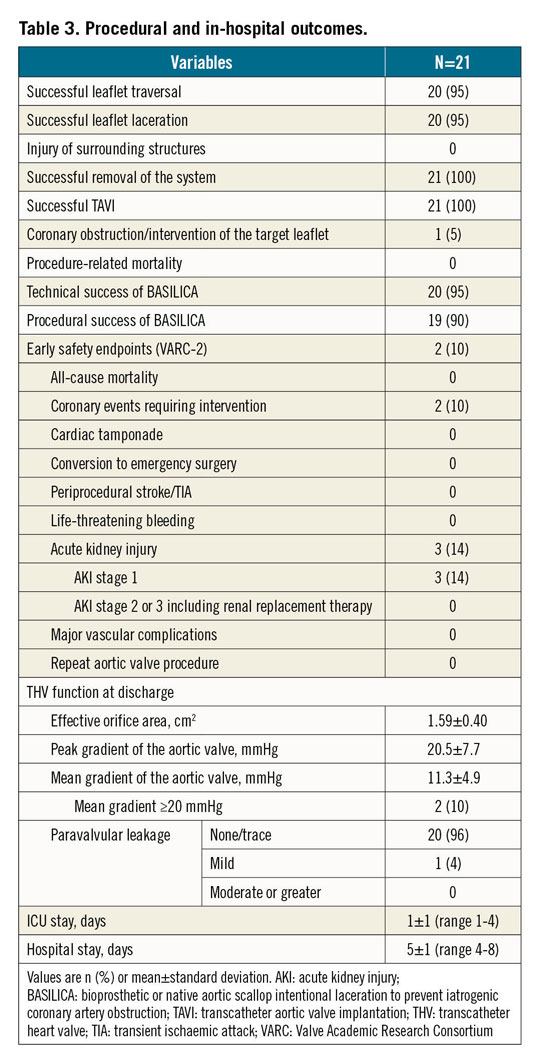
Technical success of leaflet traversal and laceration was achieved in 22 leaflets (96%) of 20 patients (95%), and procedural success was achieved in 19 patients (90%). Details of both endpoints are presented in Table 3. Procedural failure was caused by failed guidewire traversal in one patient as previously described (Figure 4), and by the need for coronary stenting due to partial coronary obstruction in another patient (Supplementary Figure 1).
EARLY SAFETY
Freedom from the VARC-2-defined early safety endpoint was 90%, with one patient (5%) developing coronary obstruction requiring intervention caused by a leaflet not targeted by BASILICA, and one patient (5%) requiring intervention due to partial coronary obstruction, as described above (Supplementary Appendix 1, Supplementary Figure 1, Supplementary Figure 2). There were no other safety endpoints, such as mortality, stroke, major or life-threatening bleeding, acute kidney injury stage 2 or 3, major vascular complications or valve-related dysfunction requiring repeat procedure.
ECHOCARDIOGRAPHIC FINDINGS AT DISCHARGE
At discharge, the effective orifice area was 1.59±0.40 cm2, and the mean transprosthetic gradient was 11.3±4.9 mmHg. Severe patient-prosthesis mismatch without an increased transprosthetic gradient was observed in one patient with a 23 mm self-expanding THV implanted in a 23 mm surgical valve with externally mounted leaflets. An increased transprosthetic gradient of ≥20 mmHg was observed in two patients (10%) (Table 3). No paravalvular leakage greater than mild was observed.
POST-PROCEDURAL CT FINDINGS
Post-procedural CT was available in 15 patients (71%). The actual observed distance between the THV and the coronary artery was 6.0±1.5 mm on the left coronary side (1.7±1.1 mm larger compared to the VTC) and 5.2±2.7 mm on the right coronary side (0.5±1.8 mm larger compared to the VTC). The correlation between VTC and the actual observed distance between the THV and the coronary artery is shown in Figure 5A (r=0.69, p<0.0001).
On the other hand, the actual observed distance between the THV and the STJ was 1.7±1.8 mm on the left coronary side (0.5±1.8 mm smaller compared to the VTSTJ) and 0.9±1.5 mm on the right coronary side (1.5±1.8 mm smaller compared to the VTSTJ). The correlation between the VTSTJ and the actual observed distance between the THV and the STJ is shown in Figure 5B (r=0.24, p=0.23). The intraclass correlation coefficient of the actual THV-to-coronary and STJ distances was 0.92 and 0.76 for the intra-observer comparison, and 0.85 and 0.80 for the inter-observer comparison, respectively (p<0.001 for all comparisons).
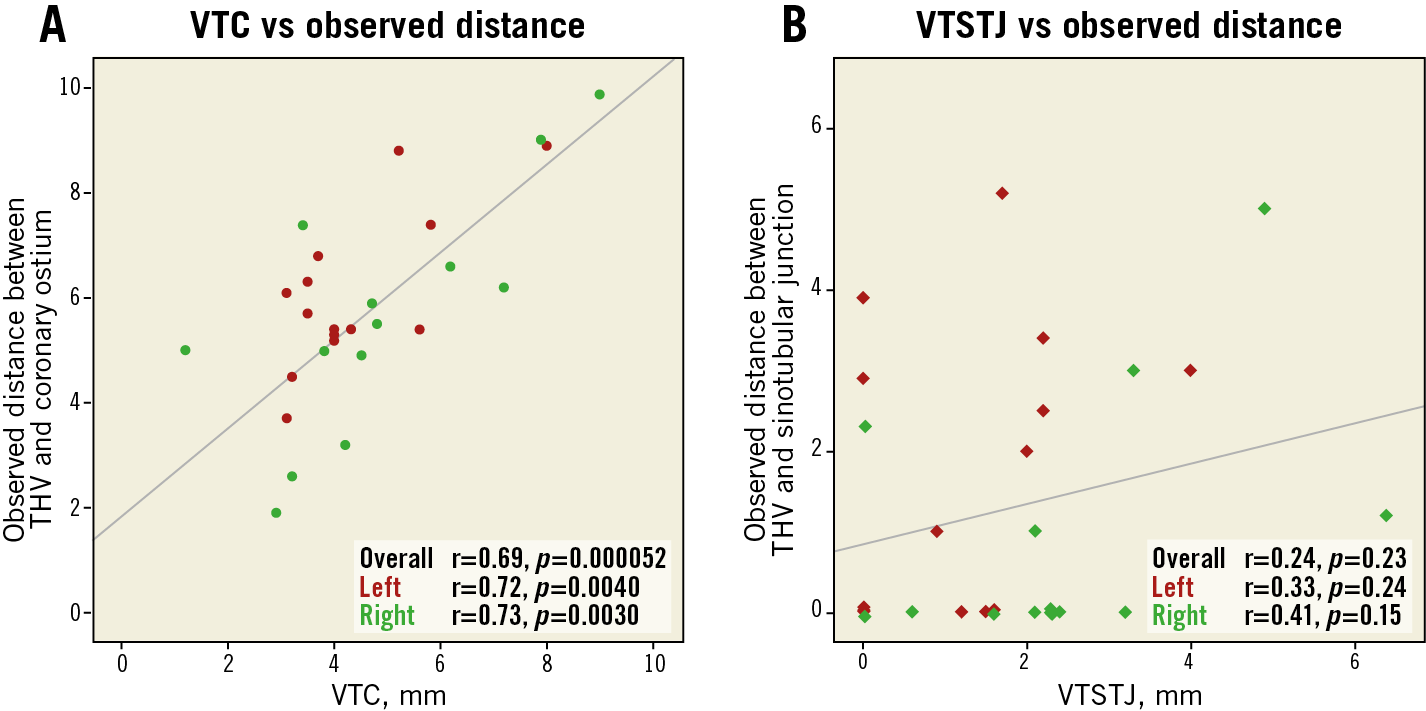
Figure 5. Scatter plot with linear regression analysis. The predicted and observed distances between (A) transcatheter heart valve and coronary ostium and (B) transcatheter heart valve and sinotubular junction are plotted. THV: transcatheter heart valve; VTC: virtual transcatheter valve to coronary distance; VTSTJ: virtual transcatheter valve to sinotubular junction distance
Neither hypoattenuated leaflet thickening nor hypoattenuation affecting motion was observed in the 15 patients who were evaluated by post-procedural CT.
Discussion
BASILICA has recently emerged as an ancillary technique for preventing TAVI-induced coronary obstruction, but its initial application in clinical practice has been limited to selected pioneering centres in the USA. The present study is the first report of a consecutive series of procedures performed outside the USA at a single European centre. The main findings are as follows.
1) Our initial experience demonstrates an excellent technical success rate of 95%, and TAVI was successfully performed in all patients.
2) Additional bail-out coronary ostial stenting for the target leaflet after BASILICA was required in one patient (5%), in which leaflet laceration enabled co-axial coronary re-access after TAVI.
3) Failed guidewire traversal due to severe target leaflet calcification occurred in one patient (5%), and misdirected guidewire traversal into the left atrium was observed in one patient (5%).
FEASIBILITY AND EFFICACY
The technical success rate in our series was comparable to the first reported experience of the BASILICA trial (95% vs 93%)4, whereas procedural time was noticeably shorter. Although the technique was only recently introduced into clinical practice at our institution, all procedures were performed by high-volume operators expert in both TAVI and coronary intervention, with initial supervision by a dedicated BASILICA proctor. Furthermore, there were some differences in the demographic and procedural characteristics in our series compared to the BASILICA trial, with fewer native valves (10% vs 43%), a greater prevalence of aortic regurgitation as the dominant mode of disease (33% vs 3%), more common use of self-expanding THVs (86% vs 47%), and routine use of cerebral embolic protection (95% vs 43%). Native and stentless prosthetic leaflets appear to be more challenging because of the lack of fluoroscopic markers during catheter manipulation. Hence, the study population in our series might have resulted in a high technical success rate and a shorter procedural duration, and the discrepancies might have affected the procedural details and outcomes.
Leaflet traversal is probably the rate-limiting procedural step. Almost one third of target leaflets required three or more attempts at guidewire traversal. One potential explanation could be that calcified leaflets impair successful traversal, and relevant leaflet calcification was prevalent in 76% of target leaflets. Nevertheless, there was only one technical failure of leaflet traversal due to target leaflet calcification. With increasing experience, fine adjustment of catheter position appeared to enhance the possibility of successful traversal by directing the traversal wire in a correct angulation to a calcium-free area. However, as stenotic aortic valves are commonly calcified, further evaluation is required to address which calcification type cannot be traversed using BASILICA. In addition, guidewire traversal could be misdirected into a non-target chamber. If the guidewire is then captured by a snare catheter, further procedural steps may injure bystanding cardiac structures, such as the left atrium, the mitral apparatus, the interventricular septum and the aortic root. Therefore, the snare should be placed immediately under the aortic annulus. Furthermore, intraprocedural TOE is helpful to identify the misdirected guidewire traversal at an early stage of the procedure in addition to fluoroscopic imaging.
EARLY SAFETY
Some specific complications of the BASILICA technique have been a concern. These include vascular access-site complications, periprocedural stroke and injury of non-target structures, as the technique requires frequent exchange of catheters and sometimes extensive manipulation of highly degenerated leaflets. In addition, haemodynamic collapse due to ventricular fibrillation induced by electrical current transmission or delayed THV implantation following iatrogenic aortic regurgitation after leaflet laceration may occur. In our series, neither significant haemodynamic deterioration nor TAVI-related complications according to the VARC-2 safety criteria were observed, except for the additional coronary interventions previously described. There are some potential explanations. First, we selected large-sized sheaths and preferred to implant self-expanding THVs, which avoids sheath exchange for TAVI implantation and may have shortened the time of haemodynamic compromise. Second, it appears helpful to maintain baseline systolic blood pressure above 120 mmHg prior to leaflet laceration. Third, all procedures were monitored with intraprocedural TOE by an expert anaesthesiologist, providing further information about catheter and guidewire position. Fourth, we routinely used cerebral embolic protection, which might have avoided potential strokes. In addition, the relatively short procedure time might have reduced the overall risk of periprocedural complications.
FUTURE CONSIDERATIONS FOR REDO TAVI
Theoretically, leaflets implanted in a supra-annular position may increase the risk of coronary obstruction during redo procedures. If the STJ is enclosed by the THV stent, the deflected leaflet may lead to sinus sequestration (Figure 3B). Furthermore, leaflet deflection by a further transcatheter implant could impair or prevent coronary access. Based on these considerations, leaflet splitting by BASILICA may be required before redo TAVI procedures. Our experience in this context is limited to one single case8; further bench-top and in vivo experience is required to define the feasibility and efficacy of BASILICA for failed THVs.
Study limitations
Our study has several limitations. First, all procedures were performed at a single high-volume centre by operators experienced in both TAVI and coronary interventions; therefore, the results may not be generalisable. Second, although CT pre-evaluation was essential for the indication and planning of BASILICA, the optimal thresholds for prediction of coronary obstruction remain to be established; thus, the patient selection might not have been optimal. Finally, although our institution has a high volume of TAVI (>900 procedures annually), the size of the study population remains relatively small. Further evaluation in larger multicentre cohorts is therefore required.
Conclusions
In this single-centre early experience with consecutive BASILICA in patients at high risk for TAVI-induced coronary obstruction, the technique was associated with a high success rate and no major safety events. The widespread use of cerebral embolic protection devices during BASILICA may prevent cerebral thromboembolic events. Larger multicentre studies with longer follow-up are necessary to clarify the reproducibility of these results further and to elucidate the long-term outcomes of this emerging technique.
|
Impact on daily practice In this early European experience, technical success and procedural outcomes of the recently introduced BASILICA technique seem to be consistent with the initial proof-of-concept studies in the USA. The technique requires demanding catheter manipulation using a percutaneous electrosurgery system on the background of a three-dimensional understanding of the aortic root and coronary anatomy; however, it remains effective in preventing TAVI-induced coronary obstruction in the vast majority of patients. Certain procedural aspects as well as optimal patient and leaflet selection remain to be clarified. |
Conflict of interest statement
D. Dvir is a consultant to Edwards Lifesciences, Medtronic and Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.