Abstract
Aims: Leaflet perforations are usually not treated by interventional therapy. In our case we describe a clinical scenario after previous surgical repair of mitral regurgitation combining several treatment strategies for correction.
Methods and results: Under general anaesthesia, and using echocardiographic as well as fluoroscopic guidance, a transseptal approach was carried out and two MitraClips were implanted at the level of A2/P2. At completion echocardiography, a new large regurgitation jet was observed in the centre of the anterior mitral leaflet. We decided to proceed with the implantation of an 8 mm AMPLATZER ASD septal occluder device (AMPLATZER™ Septal Occluder; St. Jude Medical, St. Paul, MN, USA) to seal the defect. This was accomplished and final echo showed remaining trivial regurgitation from the coaptation area, while the perforation was completely sealed. The patient was discharged in a clinically improved condition. Pre-discharge transthoracic echocardiography showed the two MitraClips as well as the Amplatzer device in a stable correct position with trivial residual mitral regurgitation.
Conclusions: The harmonisation of two diametral techniques for the treatment of recurring mitral regurgitation was effective in correcting the underlying problem. This approach may serve as an addition to the armamentarium of physicians treating patients with structural heart valve defects.
Introduction
A 68-year-old male was admitted to our department with recurrent severe mitral regurgitation (vena contracta 9 mm; regurgitant volume 90 ml/beat) seven years after surgical correction of a P2 prolapse (neochordae implantation, P1/P2 cleft closure and semi-rigid annuloplasty). The clinical history of the patient was positive for bacterial endocarditis. The leading symptom was dyspnoea on exertion, NYHA Class II. The mechanism of recurrent mitral regurgitation was determined by transoesophageal echocardiography showing recurrent P2 prolapse with flail, most likely on the basis of neochordae rupture. After formal Heart Team discussion, mainly based on the frail status of the patient, a MitraClip (Abbott Vascular, Santa Clara, CA, USA) implantation was planned1.
Under general anaesthesia, echocardiographic as well as fluoroscopic guidance, a transseptal approach was used and two MitraClips were implanted at the level of A2/P2. At completion echocardiography, a new large regurgitant jet was observed in the centre of the anterior mitral leaflet. Initially, an iatrogenic lesion was postulated, but the morphology and location of the lesion were highly unlikely to be iatrogenic (Figure 1). This defect was probably masked by the initial dominant eccentric regurgitation. Therefore, correction of the flail unmasked the lesion. We decided to proceed with the implantation of an 8 mm AMPLATZER™ ASD Septal Occluder device (St. Jude Medical, St. Paul, MN, USA) to seal the defect. This was carried out, with final echo showing remaining trivial regurgitation from the coaptation area, while the perforation was completely sealed (Figure 2). The patient was discharged in a clinically improved condition. Pre-discharge transthoracic echocardiography showed the two MitraClips as well as the Amplatzer device in a stable, correct position with trivial residual mitral regurgitation.
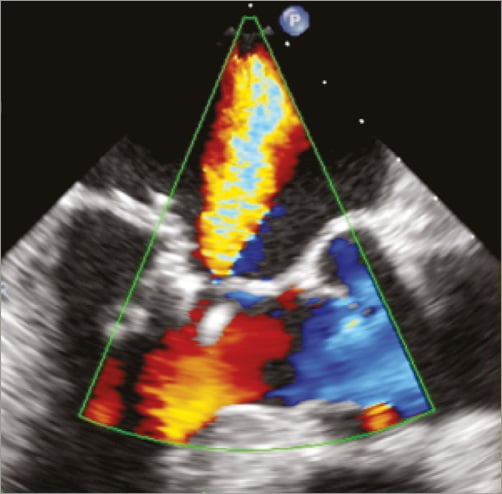
Figure 1. TEE LVOT view showing severe mitral regurgitation due to anterior leaflet perforation in the mid part of the leaflet, after the implantation of the second MitraClip. This central jet became visible only after the treatment of the P2 prolapse.
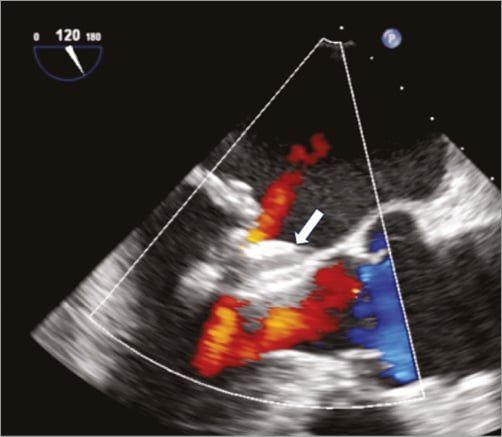
Figure 2. Post-procedural TEE LVOT view showing the final result, with stable position of the two MitraClips and of the Amplatzer device (white arrow). Only residual trivial mitral regurgitation is present.
Discussion
Rare clinical scenarios represent ideal grounds for implementing creative strategies to solve a particular challenge, as in this case. Recurrent mitral regurgitation with the underlying pathology of recurring prolapse offers an ideal scenario for MitraClip implantation, as the edge-to-edge concept in the presence of annular support already in place has proven durability2.
The additional pathophysiological component of anterior leaflet perforation was unexpected and prompted us to consider an alternative. Amplatzer occluder implantation is effective in a variety of structural defects of the heart and the great vessels3,4. To our knowledge there is no report on the application of vascular plugs to treat leaflet perforation. Regarding the aetiology of the perforation, an iatrogenic lesion was excluded as it was too far from the leaflet edges to induce leaflet tear secondary to manipulation, while the location corresponding to the jet direction could be a consequence of previous endocarditis which had healed.
As usual, discovery comes by chance. We would never have attempted such an approach if we had known about the anterior leaflet perforation. However, as the transcatheter procedure was progressing, the finding came unexpectedly. The alternative of converting the procedure into a surgical one was considered. However, vascular plug implantation in valve disease has already been reported to be effective in patients with paravalvular leaks5. The area where the plug was implanted does not contribute to coaptation and is also pretty immobile during the cardiac cycle. We therefore expect this repair to remain durable over time.
Conclusion
In summary, the harmonisation of two diametral techniques for the treatment of recurring mitral regurgitation was effective in correcting the underlying problem. This approach may serve as an addition to the armamentarium of physicians treating patients with structural heart valve defects.
| Impact on daily practice This approach may serve as an addition to the armamentarium of physicians treating patients with structural heart valve defects. |
Conflict of interest statement
The authors have no conflicts of interest to declare.