With proven safety and feasibility, percutaneous edge-to-edge mitral valve repair with the MitraClip System (Abbott Vascular, Santa Clara, CA, USA) is currently an option for patients with severe mitral regurgitation (MR) and at high surgical risk1. In about half of patients, more than one clip is needed to achieve a significant reduction of MR and, in up to 12.3% of patients, a regurgitant jet persists between or around the clips1. Implantation of additional clips to treat “inter-clip” regurgitation is not always feasible and, frequently, MR is left untreated, which is associated with poor clinical outcomes during follow-up1,2. Some reports of residual jet closure with the AMPLATZER™ Vascular Plug II (AVP II) device (St. Jude Medical, St. Paul, MN, USA) have shown reasonable results3,4. Herein, we present a case with partial detachment treated with this occluder.
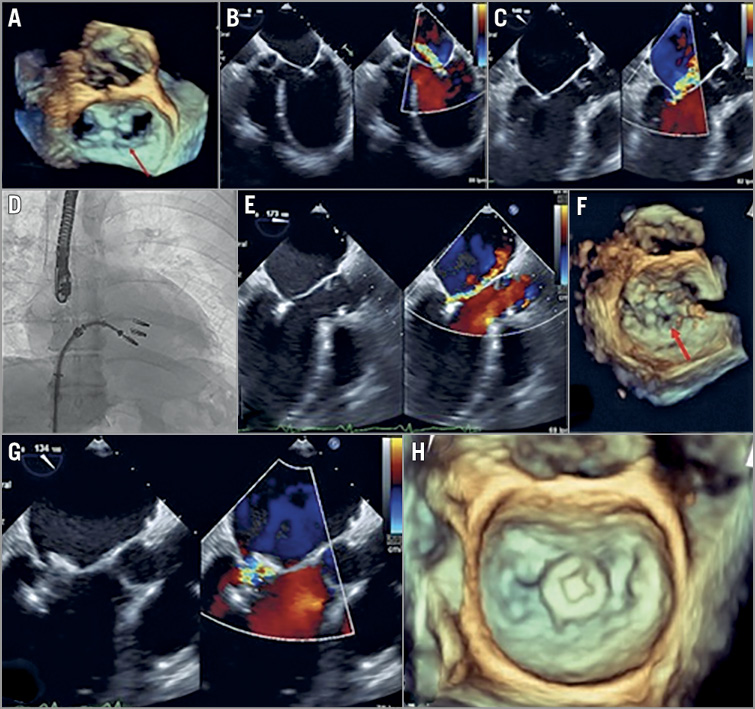
A 61-year-old man, with cardiovascular risk factors (active smoker and type 2 diabetes), was admitted in 2015 with an inferior STEMI undergoing primary PCI. After the procedure, he developed heart failure; inferolateral akinesia was shown on echocardiography, with LVEF 41% and severe functional mitral regurgitation with tenting of the posterior mitral leaflet. The EuroSCORE II estimated risk of operative mortality was 5%. After discussion in the Heart Team, a decision was made to proceed with percutaneous treatment. Mitral valve reparation was performed with implantation of two MitraClip devices in A2-P2 position, with significant improvement of mitral regurgitation. Two years later, the patient was readmitted for heart failure despite optimal medical therapy. Transoesophageal echocardiography revealed reduction of the ejection fraction (LVEF 33%) and a detachment of the posterior leaflet of the medial clip, causing severe mitral regurgitation (Panel A-Panel C, Moving image 1, Moving image 2). We proceeded to implant a third MitraClip device in a medial position (Panel D) but severe mitral regurgitation persisted through the orifice between the central clip (detached) and the posterior leaflet (Panel E, Panel F, Moving image 3, Moving image 4). Due to the impossibility of placing another clip in this position, we proceeded to implant an AVP II 12 mm occluder device (Moving image 5), achieving a significant reduction of mitral regurgitation without significant increase of transmitral gradient (Panel G, Panel H, Moving image 6, Moving image 7). The patient could be discharged seven days after the procedure and, at 30 days of follow-up, he remains in NYHA functional Class II, without new admissions.
Conflict of interest statement
D. Arzamendi and C-H. Li are proctors for Abbott Vascular. The other authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Severe mitral regurgitation on transoesophageal echocardiography with colour Doppler.
Moving image 2. Severe mitral regurgitation on transoesophageal echocardiography 3D view.
Moving image 3. Persistence of severe mitral regurgitation after the third clip implantation.
Moving image 4. 3D view showing the regurgitant orifice between the central clip (detached) and the posterior leaflet.
Moving image 5. AVP II 12 mm occluder device deployment.
Moving image 6. Colour Doppler revealing significant reduction of mitral regurgitation.
Moving image 7. 3D view showing occlusion of the orifice.
To read the full content of this article, please download the PDF.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Severe mitral regurgitation on transoesophageal echocardiography with colour Doppler.
Moving image 2. Severe mitral regurgitation on transoesophageal echocardiography 3D view.
Moving image 3. Persistence of severe mitral regurgitation after the third clip implantation.
Moving image 4. 3D view showing the regurgitant orifice between the central clip (detached) and the posterior leaflet.
Moving image 5. AVP II 12 mm occluder device deployment.
Moving image 6. Colour Doppler revealing significant reduction of mitral regurgitation.
Moving image 7. 3D view showing occlusion of the orifice.