Abstract
BACKGROUND: Both surgical aortic valve replacement (SAVR) and transcatheter aortic valve implantation (TAVI) are Class Ia recommended therapies for specific subgroups of severe aortic stenosis (AS) patients in the latest 2021 European guidelines.
AIMS: We aimed to report on the multidisciplinary Heart Team evaluation process and real-world practice of treating severe symptomatic AS in East Denmark in the context of the latest European guideline recommendations.
METHODS: All consecutive patients with severe AS referred for intervention in 2021 (N=672) were discussed in a multidisciplinary Heart Team meeting. All patients (100%) had a cardiac computed tomography (CT) analysis prior to the meeting. Baseline characteristics, Heart Team decision-making, final treatment and 30-day clinical outcomes were prospectively recorded.
RESULTS: The majority of severe AS patients (N=456, 68%) were referred for TAVI following discussion in the Heart Team. Ultimately, 94% of patients (N=632) received the Heart Team-recommended treatment. Patients undergoing TAVI (N=439) were significantly older (78.4±6.7 vs 67.2±8.3 years; p<0.001) and more comorbid than patients undergoing SAVR (N=189). The overall 30-day clinical outcomes were satisfactory for both treatment groups (overall 30-day mortality: 1.1%). The mean index hospitalisation length was markedly longer in the SAVR group (8.6±8.3 days) as compared to the TAVI group (1.8±3.2 days).
CONCLUSIONS: TAVI was routinely performed in low surgical risk patients in 2021 with two-thirds of all severe AS patients undergoing TAVI, thereby applying the latest European guidelines. A dedicated Heart Team meeting, including CT evaluation for all AS patients, is needed to make individualised management decisions in this new era of aortic valve interventions.
Following its inception 20 years ago, transcatheter aortic valve implantation (TAVI) has led to a series of paradigm shifts and has evolved into the standard-of-care treatment for elderly patients with severe, symptomatic aortic stenosis (AS) across all surgical risk categories123456. In the most recent (2021) European Society of Cardiology (ESC) guidelines for the management of valvular heart disease (VHD), both surgical aortic valve replacement (SAVR) and TAVI are considered Class Ia recommended treatments for specific subgroups of severe AS patients, with a requirement for thorough individualised Heart Team evaluation prior to final decision-making7.
Much of the evidence behind the European guideline recommendations has been derived from reports of treatment outcomes in selected patient populations, including from randomised clinical trials123456. The real-world treatment of severe AS patients in the new era of aortic valve interventions is rarely reported. This study sought to evaluate the decision-making process and management of severe symptomatic AS patients in East Denmark in 2021 and to do this in the context of the latest European guideline recommendations.
Methods
STUDY POPULATION
This study was prospective, observational and with an all-comers design and included 918 consecutive patients with severe VHD discussed in the Multidisciplinary Heart Team meeting at Rigshospitalet, Copenhagen, Denmark, between 1 January and 31 December 2021. A unique aspect is that all patients living in East Denmark, Bornholm, the Faroe Islands, and Greenland are exclusively referred to and treated at Rigshospitalet, resulting in a complete representation of all patients with severe VHD requiring intervention in this population of 2.85 million Europeans (Figure 1). Prior to the Heart Team evaluation, all patients with severe symptomatic AS underwent transthoracic echocardiography (TTE) to define the extent of their VHD and had a multidetector contrast-enhanced computed tomography (CT) investigation including comprehensive analysis of aortic root anatomy, the ascending aorta and the iliofemoral system bilaterally – in accordance with local standard operating procedures. Images were analysed using 3mensio Structural Heart software (Pie Medical Imaging BV).
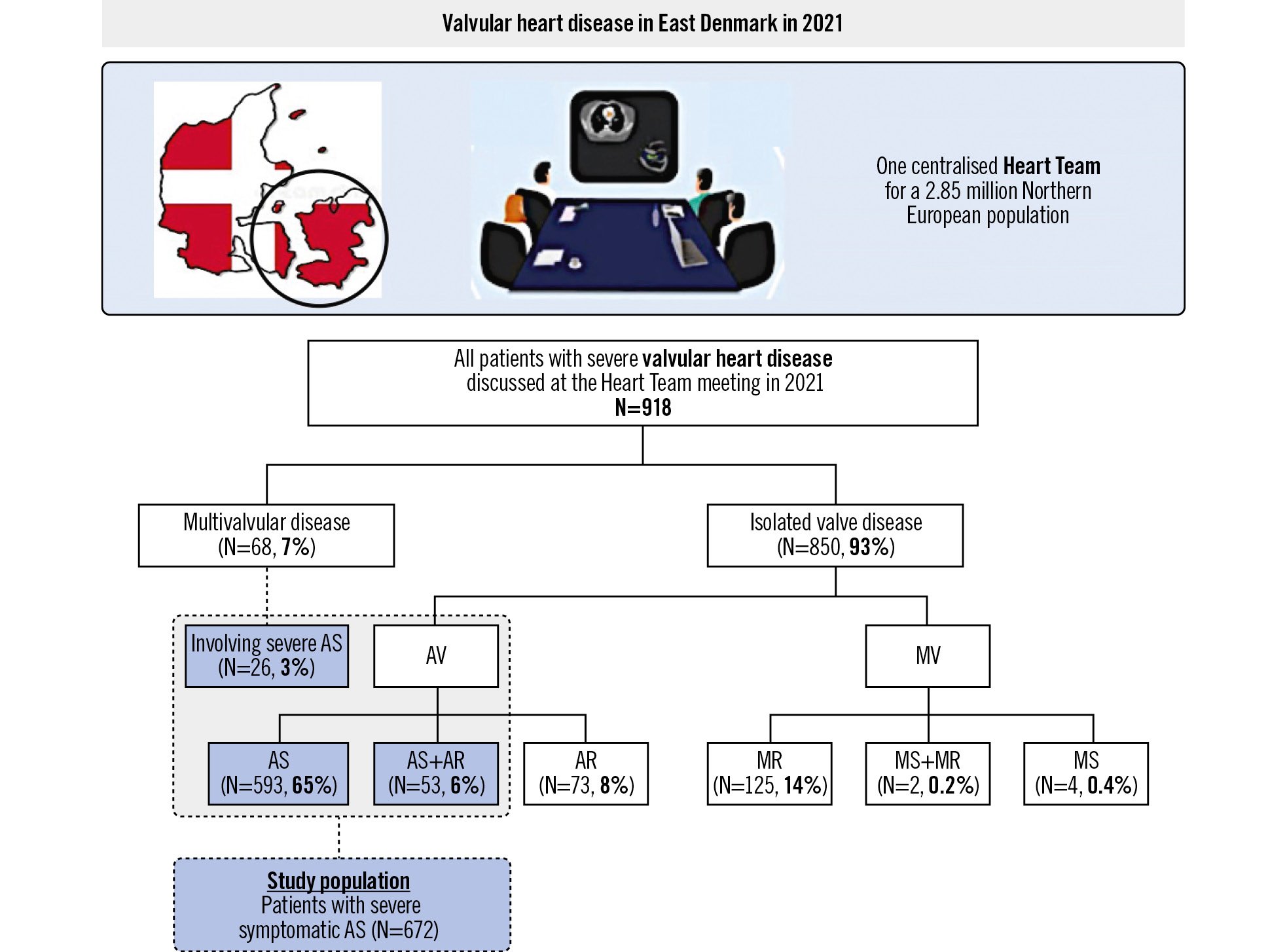
Figure 1. Valvular heart disease in East Denmark in 2021 and defining the study population. AR: aortic regurgitation; AS: aortic stenosis; AV: aortic valve; MR: mitral regurgitation; MS: mitral stenosis; MV: mitral valve
DATA COLLECTION
The baseline characteristics, TTE and CT findings for all patients with severe AS were prospectively collected at the time of the Heart Team meeting. Patients who were subsequently referred for intervention underwent their procedure at Rigshospitalet according to standardised practice, and the nature of the actual intervention was recorded and compared to the previously recommended intervention by the Heart Team. The length of hospital stay and predischarge echocardiography results were obtained from the Danish electronic medical system. The 30-day clinical outcomes, including death, stroke, major bleeding, hospital readmission for heart failure and new permanent pacemaker implantation (PPI), were collected at clinical follow-up and adjudicated in accordance with the updated standardised Valve Academic Research Consortium (VARC)-3 definitions8.
In accordance with local guidelines, all patients provided written informed consent for the use of anonymised data for research. The study received ethics committee approval by VEK-D (VD-2019259-I-6499) in Denmark.
STATISTICAL ANALYSIS
Continuous variables with normal distribution are expressed as mean±standard deviation (SD) and were compared using the Student’s t-test; those without normal distribution are expressed as median (interquartile range [IQR]) and were compared using the Wilcoxon rank-sum test. Categorical data are presented as frequencies with percentages and were analysed using the chi-square or Fisher’s exact test. The comparison between the Heart Team treatment recommendation and the ultimate interventional treatment performed was shown as a Sankey diagram. Statistical analyses were performed using SPSS version 26 (IBM), and a two-tailed p-value<0.05 was considered to indicate statistical significance.
Results
STUDY POPULATION
During the enrolment period, 918 patients with severe VHD were discussed in the Heart Team meeting (Figure 1). Of the total cohort, 850 patients (93%) had single or isolated valve disease, predominantly isolated AS (N=593, 65%) or isolated mitral regurgitation (MR) (N=125, 14%). A total of 68 patients (7%) had multivalvular disease, with the most common combination being AS+MR (N=20). Among all patients, 672 patients had severe symptomatic AS, comprising patients with isolated AS, mixed AS+aortic regurgitation (AR), and multivalvular disease including AS. This population was discussed by the Heart Team during the study period and was selected for further study.
HEART TEAM DECISION-MAKING
For all patients with severe AS, a thoroughly considered Heart Team decision was reached regarding the need and nature of the intervention to be utilised (Figure 2). A total of 456 patients (68%) were referred for TAVI and 199 patients (30%) were referred for SAVR. In 12 patients, a conservative (medical) treatment was recommended, and in 5 patients, continued surveillance was deemed appropriate. TAVI was the chosen treatment option for 357 out of 407 AS patients (88%) aged 75 years or more. The main drivers for the Heart Team recommending TAVI in patients <75 years of age and SAVR in patients >75 years of age are summarised in Figure 2.
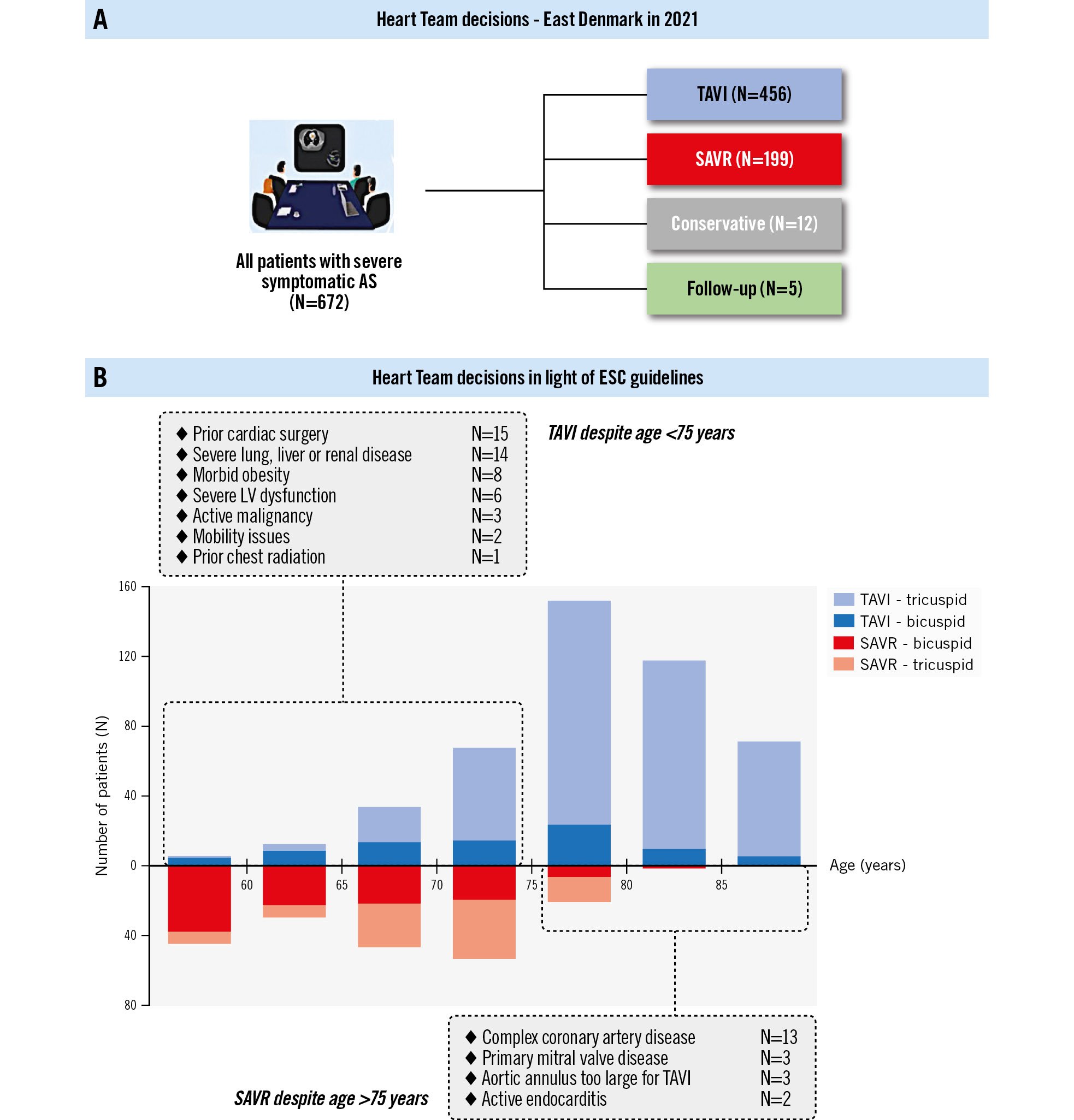
Figure 2. Heart Team decisions in 2021. A) A total of 456 patients (68%) were referred for TAVI after the Heart Team discussion, and 199 patients (30%) were referred for SAVR. B) Referral for TAVI exceeded that for SAVR in the patient cohort >70 years of age. Approximately 60% of all SAVR was performed for bicuspid AS. The main drivers for the Heart Team recommending TAVI in patients <75 years of age and SAVR in patients >75 years of age are listed. AS: aortic stenosis; ESC: European Society of Cardiology; LV: left ventricular; SAVR: surgical aortic valve replacement; TAVI: transcatheter aortic valve implantation
COMPLIANCE WITH HEART TEAM RECOMMENDATION
The Heart Team recommendation was followed and applied in a large majority of AS patients (N=632, 94%). However, deviation from recommended treatment occurred in both the TAVI and SAVR patient cohorts (Figure 3). In the TAVI cohort, 23 patients were transitioned to conservative treatment due to a decline in clinical status, the recognition that TAVI would ultimately be futile or because of patient preference. Overall, the patient’s preference (“shared decision-making”) was already integrated in the Heart Team discussion for nearly all patients.
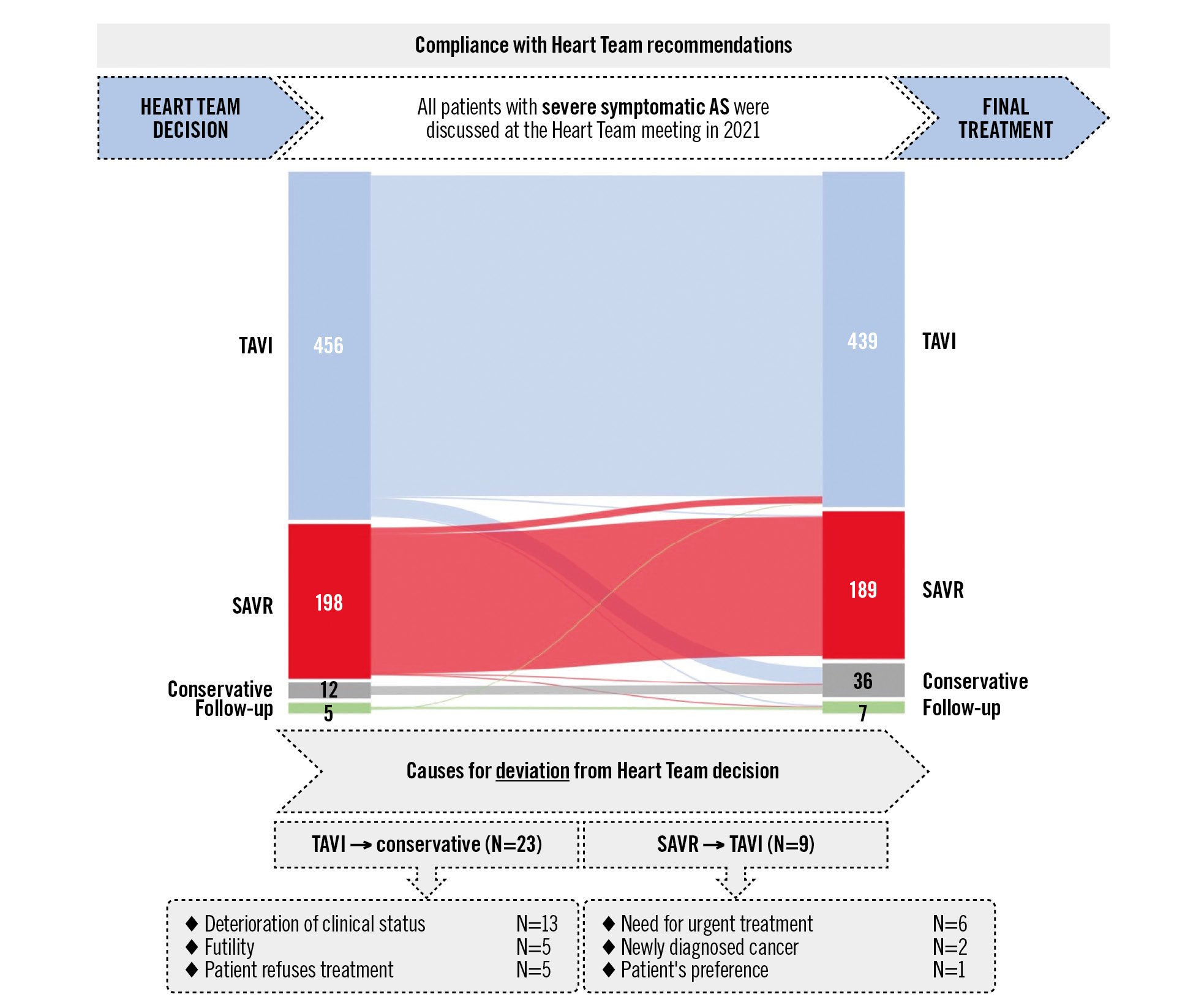
Figure 3. Compliance of final treatment with the Heart Team decision. Ultimately, 439 patients (65%) discussed at the local Heart Team meeting in 2021 underwent TAVI, while 189 patients (28%) underwent SAVR. Deviation from recommended treatment occurred in both the TAVI and SAVR cohorts of patients. Most patients (94%) received the recommended therapy. AS: aortic stenosis; SAVR: surgical aortic valve replacement; TAVI: transcatheter aortic valve implantation
BASELINE CHARACTERISTICS AND 30-DAY OUTCOMES
The baseline characteristics of patients ultimately undergoing SAVR (N=189) and TAVI (N=439) are reported in Table 1. Patients in the TAVI group were significantly older (78.4±6.7 vs 67.2±8.3 years; p<0.001), had more comorbidities, and had a higher mean Society of Thoracic Surgeons (STS) score (2.3%±1.2% vs 1.3%±0.5%; p<0.001) as compared to the SAVR group. In addition, patients treated with TAVI were less likely to have a bicuspid aortic valve and aortopathy (Table 1).
Procedural characteristics and 30-day outcomes are summarised in Figure 4. Besides 8 patients (1.8%) that underwent percutaneous transaxillary TAVI, all other TAVI were performed by the transfemoral approach. General anaesthesia was used in 100% and 4% of SAVR and TAVI patients, respectively. In 420 TAVI patients (96%), only local anaesthesia without conscious sedation was used. Nearly 40% of SAVR patients had a concomitant cardiac intervention, predominantly coronary revascularisation. Most SAVR patients (N=156, 83%) were treated with a stented bioprosthetic valve; 15% of SAVR patients (N=29) received a mechanical valve. TAVI patients were mainly treated with self-expanding transcatheter aortic valves (N=426, 96%) (Figure 4). A list of the valve types used can be found in Supplementary Table 1. Clinical outcomes following TAVI and SAVR were not statistically compared because of the substantially different baseline characteristics of both populations.
Table 1. Baseline characteristics.
| SAVR N=189 | TAVI N=439 | p-value | |
|---|---|---|---|
| Clinical characteristics | |||
| Age, years | 67.2±8.3 | 78.4±6.7 | <0.001 |
| Male | 140 (74) | 268 (61) | 0.002 |
| Arterial hypertension | 115 (61) | 311 (71) | 0.012 |
| Diabetes mellitus | 30 (16) | 92 (21) | 0.15 |
| Body mass index, kg/m2 | 27.0±4.5 | 27.0±5.1 | 0.99 |
| Body mass index >40 kg/m2 | 0 | 10 (2) | 0.36 |
| Coronary artery disease | 77 (41) | 198 (45) | 0.37 |
| Prior CABG | 1 (0.5) | 26 (6) | 0.004 |
| Prior valve surgery | 4 (2) | 17 (4) | 0.15 |
| Atrial fibrillation | 26 (14) | 158 (36) | <0.001 |
| Prior stroke | 13 (7) | 57 (13) | 0.03 |
| Peripheral arterial disease | 11 (6) | 17 (4) | 0.48 |
| Chronic renal failure* | 5 (3) | 60 (14) | <0.001 |
| Chronic lung disease | 13 (7) | 70 (16) | 0.005 |
| STS risk score, % | 1.3±0.5 | 2.3±1.2 | <0.001 |
| STS risk score ≥3% | 1 (0.5) | 101 (23) | <0.001 |
| Echocardiography | |||
| LV ejection fraction, % | 53±10 | 52±11 | 0.15 |
| LV ejection fraction <35% | 13 (7) | 40 (9) | 0.56 |
| Mean AV gradient, mmHg | 51±16 | 51±14 | 0.93 |
| Aortic valve area, cm2 | 0.77±0.19 | 0.70±0.17 | <0.001 |
| Aortic regurgitation ≥moderate | 22 (12) | 35 (8) | 0.15 |
| Mitral regurgitation ≥moderate | 5 (3) | 18 (4) | 0.36 |
| Tricuspid regurgitation ≥moderate | 0 | 9 (2) | 0.12 |
| Cardiac computed tomography | |||
| Aortic annulus mean Ø, mm | 26.6±3.1 | 25.2±2.3 | <0.001 |
| Aortic annulus mean Ø ≤23 mm | 20 (11) | 84 (19) | 0.02 |
| Bicuspid aortic valve | 111 (59) | 70 (16) | <0.001 |
| Ascending aorta diameter ≥45 mm | 15 (8) | 9 (2) | <0.001 |
| Porcelain aorta | 0 | 9 (2) | 0.11 |
| Data are reported as mean±standard deviation and n (%). *Chronic renal failure, defined as glomerular filtration rate <45 mL/min/1.73 m2. AV: aortic valve; CABG: coronary artery bypass grafting; LV: left ventricular; SAVR: surgical aortic valve replacement; STS: Society of Thoracic Surgeons; TAVI: transcatheter aortic valve implantation | |||
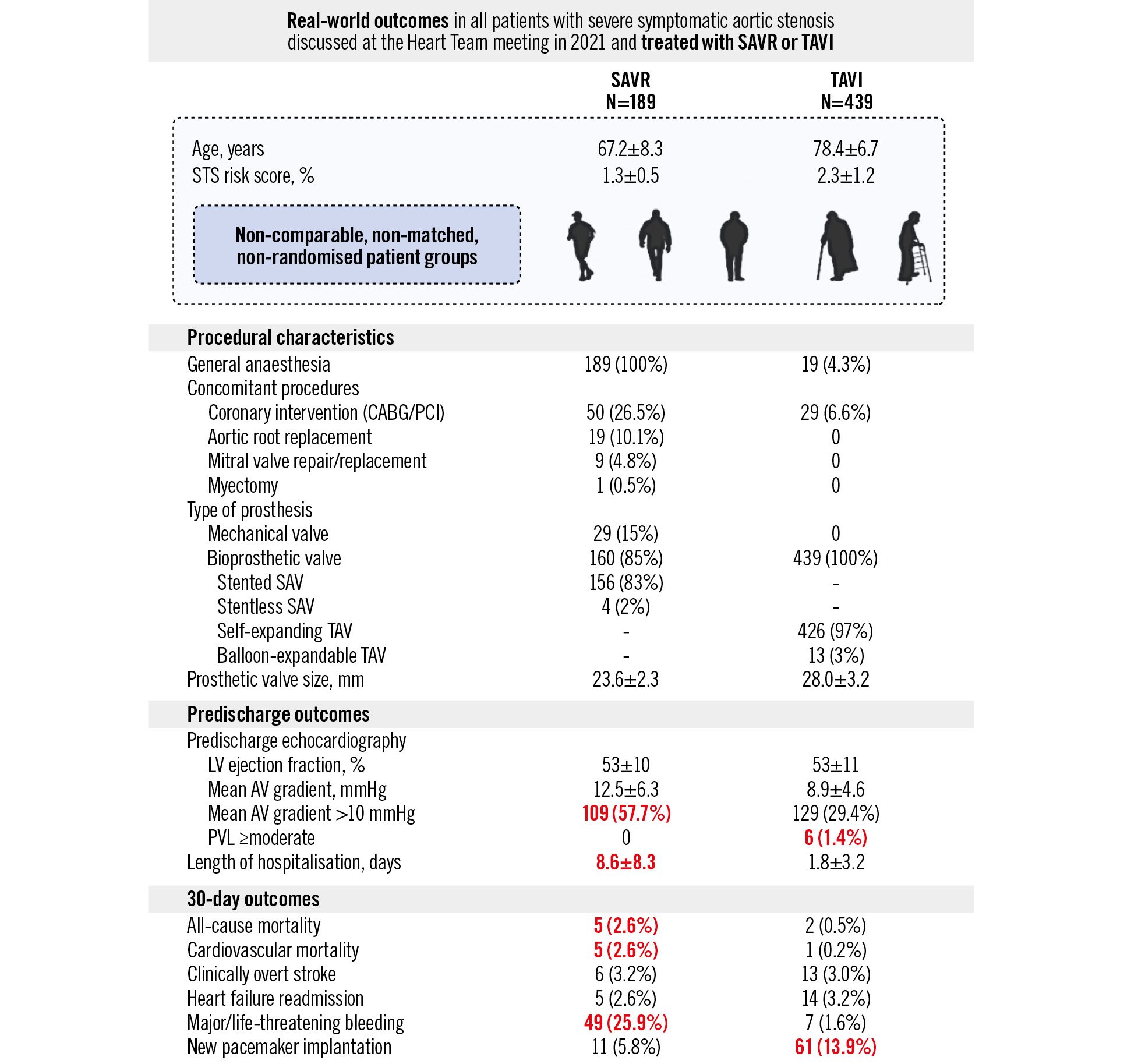
Figure 4. Real-world clinical outcomes of SAVR and TAVI. Side-by-side reporting of the clinical outcomes in all patients with severe symptomatic AS discussed at the Heart Team meeting in 2021 and treated with SAVR and TAVI in Copenhagen. A statistical comparison was not performed considering the substantially different baseline characteristics of both cohorts. Still, noteworthy differences (shown in red) between both groups were recorded for predischarge transvalvular gradient, length of hospitalisation, all-cause or cardiovascular mortality, and major/life-threatening bleeding, which favour TAVI, and predischarge significant PVL, and new pacemaker implantation, which favour SAVR. AV: aortic valve; CABG: coronary artery bypass graft; LV: left ventricular; PCI: percutaneous coronary intervention; PVL: paravalvular leak; SAV: surgical aortic valve; SAVR: surgical aortic valve replacement; STS: Society of Thoracic Surgeons; TAV: transcatheter aortic valve; TAVI: transcatheter aortic valve implantation
Discussion
This prospective, observational, all-comers study describes the real-world management of patients with severe symptomatic AS in a population of nearly 3 million Northern Europeans in the context of the latest European guidelines for the treatment of VHD.
Over 900 patients with VHD were discussed by the Copenhagen Heart Team during 2021, including 672 patients with severe AS, who were the focus of this study. In comparison, 487 patients with severe AS were discussed by the Heart Team in 2011, indicating an increase of 38% in this 10-year period9. This likely reflects increased referrer recognition that TAVI may be a valuable treatment option for patients who would not have been considered suitable for SAVR 10 years ago as well as the overall ageing of the Danish population. The utilisation of TAVI as a treatment modality for severe symptomatic AS has increased in East Denmark over this same 10-year time period from 12% to 65%, in 2011 and 2021, respectively9. Thereby, it is important to recognise that all consecutive patients with severe AS referred for intervention were included, whereas patients with isolated severe AR were excluded from this analysis and predominantly underwent SAVR.
Overall, the data presented in this study demonstrate that East Danish practice with regards to the treatment of severe symptomatic AS has been consistent with the ESC guidelines7. In our 2021 patient cohort, we documented that the age bracket at which the use of TAVI exceeded SAVR was between 70 and 75 years of age. The individual patient factors that the Heart Team took into consideration when recommending TAVI despite age <75 years and SAVR despite age >75 years were consistent with the ESC guidelines (Figure 2). In comparison, in the USA, TAVI was the chosen treatment modality for 87.5% of all patients with severe isolated AS aged 65 to 80 years in 2021, as recently reported by Sharma et al10.
It is also worth noticing that 84% of all patients with symptomatic severe AS referred for aortic valve interventions had an STS score <3% and would be classified as low surgical risk. However, as reported earlier by our group11, STS scores are rarely calculated or used at our centre when discussing patients at the Heart Team meeting. Following the publication of the low-risk TAVI trials, PARTNER 3 and Evolut Low Risk, the guidelines have also (correctly) given less weight to these calculated risk scores. A calculated STS score can be a useful parameter when designing and conducting clinical studies. However, when discussing an individual patient at the Heart Team meeting, anatomical eligibility, age and the patient’s lifetime management options are considered more important criteria in contemporary decision-making.
Importantly, this real-world study also demonstrates that the implementation of a Heart Team model and discussion, which follows the ESC guidelines, resulted in a treated cohort with limited “crossover” (Figure 3). Very few patients transitioned from SAVR to TAVI or from TAVI to conservative treatment. This emphasises the value of Heart Team decision-making following thorough preassessment, including CT analysis of the aortic valve complex, ascending aorta and access vessels. The preprocedural CT not only determines the anatomical suitability for TAVI but also documents important coexistent pathologies, such as aortopathy or a porcelain aorta, that may influence the final decision-making. The ESC and American College of Cardiology/American Heart Association (ACC/AHA) guidelines also mention the importance of “shared decision-making”, which has readily been adopted in the Northern European setting. Having an open conversation with the patient about the treatment options and their implications before, rather than after, the Heart Team meeting further helps to keep this “crossover” to an absolute minimum (Central illustration).
Still, a potential contributor to patients moving both from TAVI to conservative therapy and from SAVR to TAVI includes increased waiting list times due to limited resources. Patients awaiting TAVI can become increasingly frail and ultimately become unsuitable candidates for intervention. Similarly, prolonged surgical waiting times or the need for a shorter recovery period prior to pending urgent non-cardiac surgery can result in a patient transitioning from SAVR to TAVI.
When comparing baseline characteristics of the SAVR- and TAVI-treated cohorts, there are several important and expected differences. Patients with severe AS undergoing TAVI are older and more comorbid than SAVR patients, in part reflected by a higher mean STS surgical risk score (Table 1). Particularly noteworthy is the low number of patients with prior cardiac surgery undergoing SAVR (N=4) in our overall SAVR/TAVI-treated population. Prior cardiac surgery was also the most common cause for younger patients <75 years being referred to TAVI. Whilst not driven by peer-reviewed data, there is a clear shift away from resternotomy, and, in recognition of this, it becomes increasingly important for cardiac surgeons to more carefully consider the index SAVR procedure (valve type and size) as we move into lifetime management of AS patients and the potential need for future transcatheter valve-in-valve procedures.
This observational study also shows that TAVI was more frequently used to treat AS patients with a small aortic annulus dimension (diameter ≤23 mm). This may partially be explained by the higher representation of women in the elderly TAVI population but is mainly a result of TAVI being the preferred treatment option for patients with a small aortic annulus. Clearly, this is only possible when the cardiac CT is analysed before the Heart Team meeting, as it has been systematically done in East Denmark since 2020. As reported earlier by Deeb et al, aortic annulus size has a significant effect on haemodynamics and the incidence of patient-prosthesis mismatch (PPM) in SAVR patients, an outcome not observed in TAVI patients. With respect to aortic annulus size, TAVI results in better haemodynamics and less PPM for annuli less than 26 mm and should be strongly considered when choosing a tissue valve for small and medium size annuli12.
Another important observation is that approximately 60% of all SAVR was performed for bicuspid AS. This implicates that more bicuspid aortic valves should be treated by TAVI, in which case TAVI would further expand into treating even younger patients (Central illustration). Recently, we have seen increased utilisation of TAVI in this cohort of patients despite the absence of large randomised controlled data demonstrating non-inferiority to SAVR or robust long-term data on TAV durability13. It is incumbent on Heart Team clinicians to ensure this is discussed with the patient prior to TAVI if this is the recommended treatment modality for severe bicuspid AS.
Given that this study involved non-matched cohorts, we did not perform a statistical comparison of clinical outcomes. Still, there were some noteworthy findings. Not surprisingly, the hospital length of stay was significantly shorter in the TAVI cohort − 1.8 days versus 8.6 days in the SAVR cohort. In times where not only clinical outcomes but also logistical and economic impact play an increasingly important role, this information should also be considered when discussing the best treatment option(s) on a patient population level. The overall safety profile of both treatment groups was good with a 30-day mortality rate of 1.1%. However, the 30-day all-cause and cardiovascular mortality rate was higher in the SAVR cohort (Figure 4), potentially reflecting the need for concomitant coronary artery grafting or a second valve procedure but also reflecting the more invasive character of SAVR with a 25.9% major bleeding incidence. Despite the significantly older and more comorbid patient profile in the TAVI cohort, a 30-day mortality rate of 0.5% only confirms the minimally invasive character and good safety profile of TAVI. Another well-established finding was that the PPI rate was higher in the TAVI cohort (13.9%); however, 5.8% of SAVR patients also required PPI. Finally, there was also a difference in the predischarge mean transvalvular gradient between surgical and transcatheter aortic valves; whether this will translate into a difference in valve durability in the longer-term has yet to be seen (Figure 4).
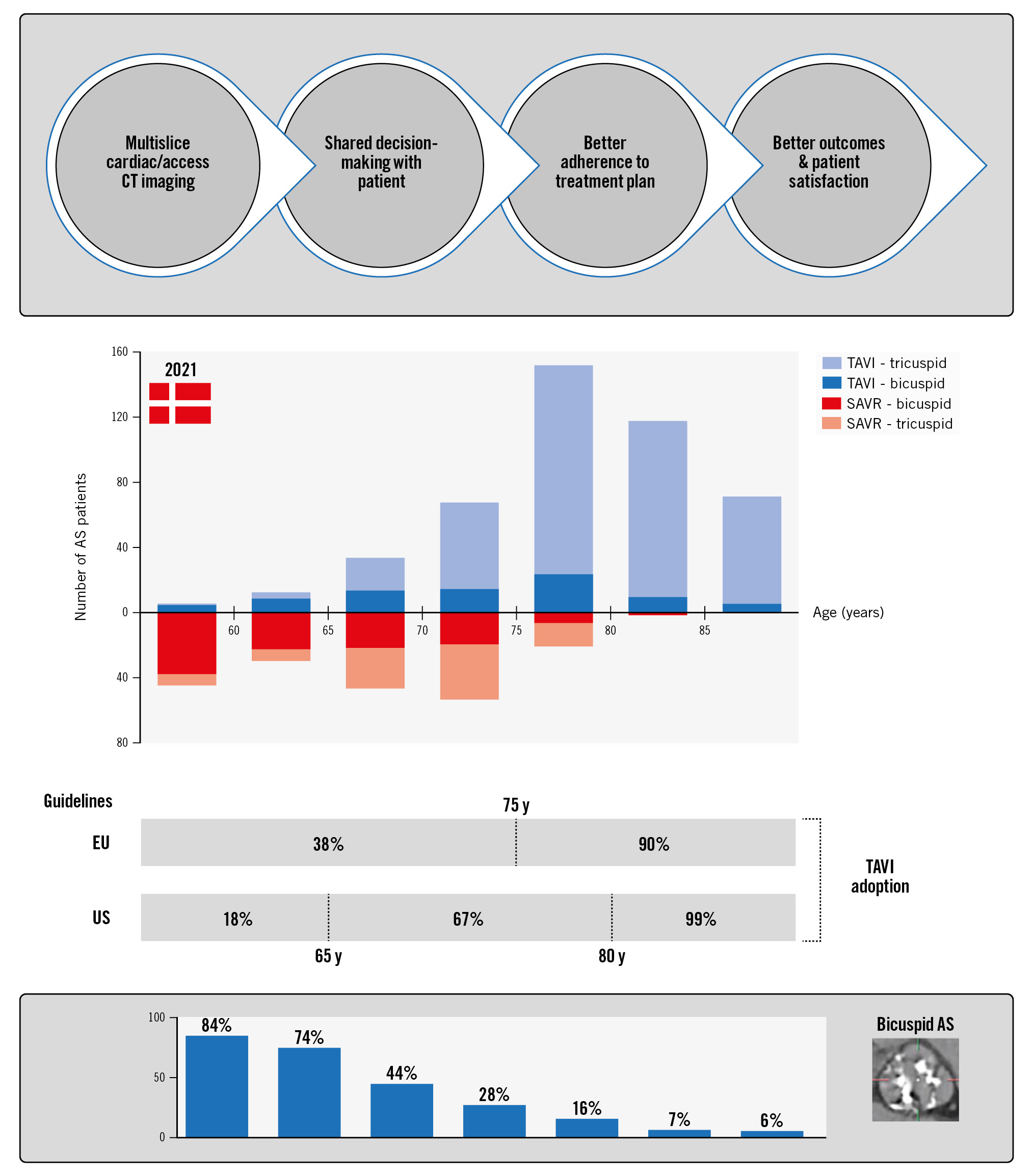
Central illustration. Central role of the Heart Team in the management of severe symptomatic aortic stenosis. This Central illustration highlights the adoption of TAVI in East Denmark in 2021 from the perspective of the European and American guidelines for the management of VHD. Furthermore, it indicates which proportion of TAVI and SAVR patients had a bicuspid anatomy in the different age categories. AS: aortic stenosis; CT: computed tomography; SAVR: surgical aortic valve replacement; TAVI: transcatheter aortic valve implantation; VHD: valvular heart disease
Limitations
This study only reports on the real-world management of severe AS in East Denmark; observations from other European countries are warranted in order to report on a more pan-European approach. Moreover, this observational study only reports 30-day clinical outcomes; longer-term follow-up is needed in order to report on lifetime management of severe AS in real-world practice. Importantly, however, this study comprises all severe symptomatic AS patients that were referred for SAVR or TAVI in the study period. No patient with severe AS underwent SAVR or TAVI without prior Heart Team discussion. Moreover, as a testimony to the rigour with which this study was conducted, none of the patients included in this study were lost to follow-up.
Conclusions
This real-world study highlights that TAVI is now routinely performed in low surgical risk patients in East Denmark, with two-thirds of all severe symptomatic AS patients undergoing TAVI, thereby demonstrating application of the latest 2021 European guidelines. A dedicated Heart Team meeting, including cardiac CT evaluation for all AS patients, is needed in order to make individualised management decisions in this new era of aortic valve interventions.
Impact on daily practice
Both the latest guideline recommendations and real-world practice reflect the paradigm shift in the management of patients with severe symptomatic AS, with TAVI having become the first-choice treatment for elderly AS patients, regardless of their estimated surgical risk. A dedicated Heart Team meeting, including cardiac CT analysis, is needed to make an individualised management decision in the new era of aortic valve interventions.
Acknowledgements
The authors thank the Chinese Scholarship Council for the scholarship given to Dr Xi Wang for her research training at Rigshospitalet, Copenhagen University Hospital, Denmark.
Conflict of interest statement
K. Arslani has received research grants from the Swiss Academy of Medical Sciences, the Gottfried and Julia Bangerter-Rhyner-Foundation, and the Swiss National Science Foundation (P500PM_202963), Switzerland, outside the submitted work. G. Bieliauskas has received consulting fees from Abbott, Boston Scientific, and Medtronic. L. Sondergaard is Chief Medical Officer at Abbott Structural Heart; and has received institutional research grants and/or consulting fees from Abbott, Boston Scientific, Medtronic, and SMT. O. De Backer has received institutional research grants and consulting fees from Abbott and Boston Scientific. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.