
Abstract
Aims: The aim of this study is to present our experience with a new type of extra-large stent, namely the AndraStent XL/XXL.
Methods and results: AndraStents were implanted in 46 patients, 38 with native coarctation of the aorta (CoA) and eight with recurrent coarctation of the aorta following previous surgery (ReCoA). All patients had arterial hypertension in the upper limbs, absent or weak femoral pulses, and continuous flow in the abdominal aorta on Doppler examination. The median age of patients was 25 years (range from nine to 65). The stents (cobalt-chromium with semi-open cell design) were manually mounted on balloon catheters and delivered through 10 to 14 Fr Mullins sheaths using a conventional femoral approach. All procedures were successful (no stent migration, proper expansion, no aorta dissection/rupture, major bleeding or major vessel injury). The systolic gradient across the aorta decreased from 40.6 mmHg before the procedure to 11.6 mmHg after the procedure (p<0.001). The mean fluoroscopy time was 5.7 minutes. Imaging examinations were scheduled and performed between six and 12 months after the initial procedure in 40 patients (angiography or angio CT or both). Procedural outcome remained favourable during a mean 2.4 years of follow-up. Neither stent fracture nor dislocation was observed in any patient at follow-up. In two patients, small aneurysm formation was observed six and eight months after the procedure –they were treated successfully with subsequent covered stent implantation. Re-dilatation of the implanted stent was performed between four and 26 months in 14 patients.
Conclusions: Implantation of new large cobalt-chromium stents is a good therapeutic option for the treatment of native and recurrent CoA.
Introduction
Coarctation of the aorta (CoA) includes a wide array of anatomic and pathophysiologic variations. All involve the same form of narrowing of the aorta, resulting in pathologic obstruction of blood flow from the systemic ventricle to the systemic circulation. CoA comprises about 7% of known congenital heart disease, making it the fourth most common lesion requiring surgical or catheter-based intervention1.
Over the past two decades, endovascular stent implantation has become an accepted modality for the treatment of native and recurrent coarctation of the aorta in older children and adults2-4. The main limiting factor for stent implantation in the youngest age category has been the lack of a stent that would be dilatable up to the adult size of large vessels and that could be implanted in patients with a body weight less than 15 kg. Stent fractures in longer follow-up represent another important issue5. These fractures can be trivial, but they can potentially cause disintegration of the entire stent.
Attention has been focused on the development of new types of stent with a smaller delivery sheath and a design that involves high radial forces, flexibility and resistance to fracture. A new type of peripheral vascular stent has been available since 2008 which could offer some additional advantages over the previously available and most commonly implanted stents. The AndraStent XL and XXL (AndraMed GmbH, Reutlingen, Germany) are balloon-expandable, non-premounted, cobalt-chromium stents that belong to the group of extra-large stents. As far as we know, there are a limited number of publications regarding its clinical application6-8. Here we present our experience with the use of the AndraStent XL and XXL for transcatheter dilation of native and recurrent postsurgical CoA. To the best of our knowledge, this paper is the first publication reporting the short to midterm results of such therapy with the use of the AndraStent XL/XXL.
Methods
PATIENTS
From March 2010 until May 2014, 46 patients (17 females) underwent transcatheter implantation of 46 AndraStent XL/XXL at our institution. Table 1 shows some demographic data for the patients. They were consecutive patients, suitable for stent placements. A retrospective review of the medical record charts was performed. There were 38 patients with native CoA and eight with recurrent CoA after previous surgical correction (two after end-to-end anastomosis, four after patch enlargement and two after a Waldhausen operation). The age range of the patients was from nine to 65 years (median 25 years) and the weight range from 25 to 105 kg (median 69.5 kg). There were 13 children and adolescents (<18 years old), 24 adults 19-39 years and nine patients aged more than 40 years. At the same time, balloon angioplasty was performed on 50 patients (15 with CoA and 35 with ReCoA), mainly in small children. Moreover, in nine patients (when special indications were present) covered Cheatham platinum (CP) stents were used. Additionally, in that period of time, 27 patients were treated surgically (23 infants). Nine patients had bicuspid aortic valve disease, one patient had a ventricular septal defect and another patent an arterial duct, two patients had Turner syndrome, and three patients had an aortic valve replaced by a mechanical one (Table 1). Patients with significant hypoplasia of the aortic arch or aortic isthmus distal to the CoA were excluded (only one patient with discrete hypoplasia of the aortic arch operated upon previously was involved in the study). We excluded patients below eight years of age with a body weight below 25 kg. In all patients, blood pressure gradient through the CoA was greater than 20 mmHg on invasive measurements. In all patients arterial hypertension in the upper limbs exceeded the 95th percentile of the limit for BSA. Absent or weak femoral pulses and continuous flow in the abdominal aorta on Doppler examination were observed. The procedure was considered successful when the direct invasive gradient was below 20 mmHg after the intervention. We obtained written informed consent from all patients with regard to the use of the AndraStent XL/XXL. The implantation protocol was approved by our hospital’s medical institutional review board.

INTERVENTIONAL PROCEDURE
Depending on age, procedures were performed under general anaesthesia (children), or local anaesthesia (adults). Cardiac catheterisation was routinely performed from the femoral artery. The AndraStents were delivered through a prepositioned long sheath. All the stents were hand-crimped and dilated with an inflation device. The stents were delivered through 10 to 14 Fr Mullins sheaths (Cook Medical, Bloomington, IN, USA) using a conventional femoral approach. The delivery sheath was selected 2 Fr larger than recommended for the applied balloon. No suture device was applied for haemostasis. The stents were dilated on Opta Pro or Maxi LD balloons (Cordis Endovascular, Warren, NJ, USA), Altos balloons (AndraTec BmbH, Koblenz, Germany) or BIB balloons (NuMED, Hopkinton, NY, USA), with diameters ranging from 10 to 26 mm. The procedure-related complications were evaluated. The aneurysm formation was defined as a >10% expansion of the aorta outside the stent or normal aorta that was not present prior to intervention. The patients were followed up at the outpatient clinic.
CHARACTERISTICS OF THE STENTS
AndraStents XL and XXL are balloon-expandable, non-premounted, cobalt-chromium peripheral stents with a hybrid cell (semi-open) design. The AndraStent XL is dilatable up to extra-large sizes (from 8 to 25 mm) and the XXL is dilatable from 10 to 32 mm. The available stent lengths are 13 (XL only), 17, 21, 26, 30, 39, 43, 48 and 57 mm. According to our experience, the crimping process on small balloons is easier for the AndraStent XL than for the AndraStent XXL. In theory, the properties of the cobalt-chromium alloy in combination with the stent design should cause higher radial force, flexibility and good visibility on angio CT imaging, and easy anchoring in the vessel wall. Details of the physical behaviour of the stents are provided by the manufacturer on every stent cover. According to the manufacturer’s information, the stent shortens: for example, the AndraStent XL 39 mm when dilated to 15 mm shortens to 35 mm and when it is dilated to 25 mm it shortens to 25 mm. Similarly, the AndraStent XXL 39 mm when dilated to 20 mm shortens to 36 mm and when it is dilated to 32 mm it shortens to 26 mm.
FOLLOW-UP
All of the patients were scheduled to have a clinical examination, ECG and transthoracic echocardiography before discharge home, then after one, three, six, 12 months, and thereafter yearly at the outpatient clinic. Imaging examinations were scheduled between six and 12 months post procedure (angiography or angio CT examination). In some patients with tight CoA, re-dilatation was planned as a staged procedure. During follow-up, incidences of all complications were recorded. The mean follow-up ranged, in the native CoA group, from 0.1 to 4.2 years (mean 2.6±1.13), and in the ReCoA group from 0.3 to 2.7 years (mean 1.7±0.92). One patient (number 35) was lost to follow-up in the planned schedule (Table 1).
Results
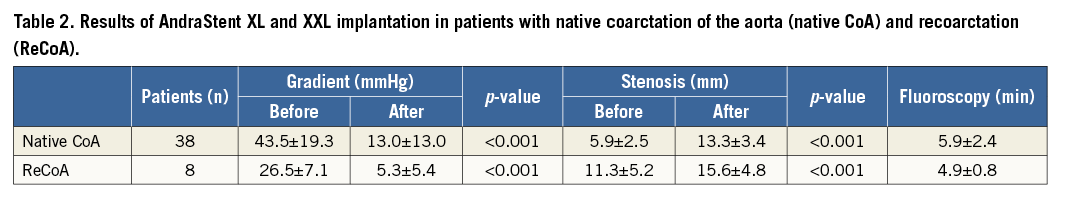
All procedures were performed successfully. Table 1 shows some details of the procedures. The results of the procedures in the CoA and ReCoA group are presented in Table 2 (gradient reduction, enlargement of narrowed segment of CoA and fluoroscopy time). Implantation of the AndraStent XL in the native CoA is shown in Figure 1.
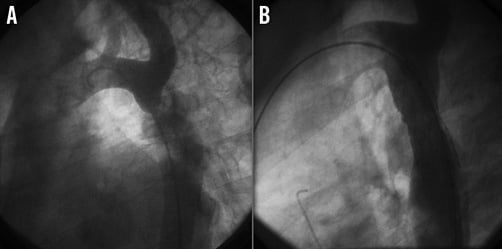
Figure 1. Native coarctation of the aorta in a 14-year-old boy- aortography (LAO 30° projection). Before (A) and after (B) AndraStent XL implantation.
No problems with stent expansion, dissection of the aortic wall or migration were observed during the procedure. The radiopacity and flexibility of the AndraStents during the procedures were sufficient. In one patient (a 49-year-old man) with severe secondary LV failure (EF 15%) the procedure was performed in an urgent manner during cardiogenic shock with a good clinical result (Table 1; patient number 15). During follow-up, control angiography was performed in 15 patients and angio CT in 18 patients. During follow-up, in seven patients both angio CT and angiography were performed before and/or after re-dilatation. Nine procedures were regarded as partially successful (gradient after procedure >20 mmHg) (Table 1; patients numbers 2, 6, 9, 14, 16, 32, 40, 43, 46). Re-dilatation sometime after the initial procedure with a larger balloon diameter was effective in all cases. In general, re-dilatation was performed in 14 patients (13 with native CoA and one with ReCoA), and from this group nine patients had planned stent angioplasty as a staged procedure because of tight stenosis. In the remaining patients, re-dilatation was related mainly to their growth acceleration. During follow-up no stent fracture was observed. In two patients (Table 1; patients numbers 25 and 31) CT examinations were performed six and eight months, respectively, after the procedure and asymptomatic small aneurysm formation was noted. This was treated successfully with subsequent covered stent implantation (Figure 2).
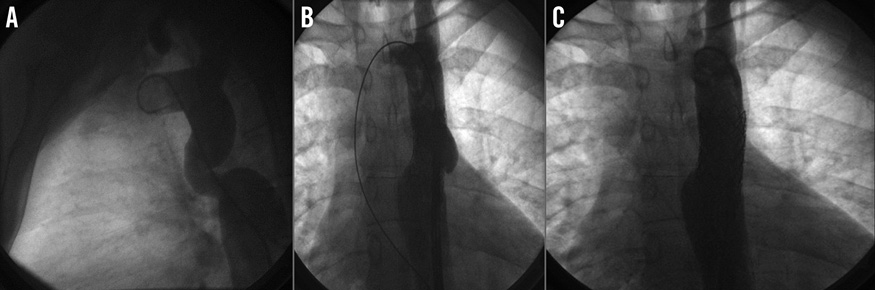
Figure 2. Angiography of a 34-year-old patient with native CoA. A) Before stent implantation (LAO 90° projection). B) Six months after AndraStent XL implantation (visible aneurysm) (PA projection). C) After covered CP stent implantation (PA projection).
In one patient with ReCoA (Table 1; patient number 44) and an aortobronchial fistula (described elsewhere9) treated previously with stengraft, because of huge post-surgical aortic aneurysm, the stengraft was dilated with an AndraStent XXL 43 mm. During follow-up, minor aortic hypertension (140/90 mmHg) persisted in two patients (Table 1; patients numbers 19 and 29). The medication was stopped in six of our patients, and reduced in 14 (in seven patients only single drug therapy of arterial hypertension was needed).
Discussion
In patients with coarctation of the aorta stent implantation is becoming the standard therapeutic option. In most patients, satisfactory relief of the aortic arch gradient was achieved after stent implantation and this benefit persisted during follow-up. Our data concerning the immediate and midterm results of application of AndraStents for CoA confirmed this. The necessity of a longer follow-up in a larger group of patients treated with AndraStents was recently postulated by Venczelova et al8, especially to evaluate the resistance of AndraStents to fractures. There are several stents on the market belonging to the group of large and extra-large stents, and each type has certain advantages and disadvantages. The previously popular Palmaz stent (Cordis, Johnson & Johnson, New Brunswick, NJ, USA) had many disadvantages: they were stiff and difficult to implant into tortuous vessels. They had sharp edges, which caused frequent balloon ruptures and significant stent foreshortening10. Cheatham platinum (CP) stents (CP™ Stent™; NuMED, Cornwall, Ontario, Canada) also belong to the group of large and extra-large stents and are nowadays most frequently used. CP stents are dilatable up to 25 mm and have lengths from 16 to 45 mm. CP stents have less radial strength than Palmaz stents. Their advantages are that they have rounded edges and are less prone to balloon rupture during stent implantation (similar to the AndraStents XL/XXL). Stent fracture can occur after CP stent implantation4,11-14, unlike the AndraStents used to dilate CoA shown by our data. Before 2010 we used bare metal CP stents for the treatment of CoA, but, because we have found AndraStents to be more useful (and also cheaper), we later changed our policy. AndraStents XL and XXL are not covered, and therefore their use may be somewhat risky in subjects with extremely tight aortic coarctation because of the probability of aortic wall aneurysm occurring after implantation. In our patient group there were four cases (Table 1; patients numbers 8, 9, 19 and 40) with a stenosed segment of the aorta of 2-3 mm: in none of them was aneurysm formation observed at follow-up. The pooled reported risk of aneurysm formation immediately after stent treatment is around 3%15. It was not present in any of our patients immediately after the procedure. However, it occurred in two patients in later follow-up (both were treated successfully with subsequent implantation of covered CP stents). Aortic rupture/dissection can also occur when a covered stent is used for coarctation treatment14,15. Therefore, it is very difficult to predict which patients treated with stent implantation will develop this serious complication16. Continuous follow-up of all patients treated with stents for coarctation of the aorta is obligatory (including imaging examination - angio, angio CT or MR)17. Application of an AndraStent in critical CoA was also effective in the urgent treatment of adult patients with cardiogenic shock (described in another paper7). AndraStents XL and XXL present a new type of stent available for the interventional cardiologist in Europe (it is not registered in the USA). The special hybrid design (semi-open cells) facilitates future interventions in the locality of the stent (for example, opening of covered subclavian artery origin). The question as to which stent is better for the treatment of coarctation of the aorta –bare metal or covered?– remains open.
Limitation of the study
This is a retrospective analysis, with a relatively small number of patients treated and only short to midterm follow-up. To confirm the good results presented here, a larger group of patients with coarctation of the aorta treated with the AndraStent with longer follow-up is needed. A randomised, prospective trial with other types of stent should clarify whether this stent is superior to others.
Conclusions
Implantation of the AndraStent XL/XXL is a good therapeutic option for the treatment of native and recurrent coarctation of the aorta.
| Impact on daily practice The application of a bare metal, cobalt-chromium stent with semi-open cell design (namely AndraStent XL/XXL) is a new therapeutic method for treatment of coarctation and recoarctation of the aorta in children and adults. This stent provides high radial strength, is flexible, shortens slightly and anchors well in the aortic wall (no stent migration during and after implantation in our material). It provides satisfactory relief of the aortic arch gradient and this benefit persisted during follow-up. In view of this feature, Andra-Stent is a good therapeutic tool for treatment of aortic coarctation. In follow-up we observed only two small aneurysm formations (treated successfully with covered stents) and there were no strut fractures. It is also a less expensive option than other currently available stents. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

