Abstract
Aims: Stent placement as treatment for coarctation of the aorta (CoA) has become a more common choice in the last 20 years. Clinical results of CoA stenting are usually reported in small retrospective case series. This systematic review provides an overview of clinical experience with stenting for CoA.
Methods and results: A systematic review of the reports published between January 1990 and December 2014 after stenting a CoA was performed with a focus on relief of obstruction and lowering of blood pressure. Study and patient characteristics were extracted, as well as pre- and post-stenting aortic diameter in mm, systolic pressure gradient (SPG) and pre- and post-stenting systolic blood pressure (mmHg), periprocedural and follow-up complications. Forty-five articles met the inclusion criteria. Three outcomes were extracted from the articles - aortic diameter, systolic pressure gradient and blood pressure. Diameter increased from 6.4 mm (5.6, 7.3) to 15.1 mm (14.5, 15.7), pressure gradients decreased from 40 mmHg (35, 42) to 4 mmHg (3, 5) and systolic blood pressure decreased from 153 mmHg (148, 158) to 132 mmHg (127, 136). Stent migration was the most common periprocedural complication (2.4%), and mortality was low (0.4%).
Conclusions: Stenting is an effective treatment with regard to immediate relief of obstruction and direct lowering effect on blood pressure. However, there is a lack of evidence regarding late effectiveness concerning durable blood pressure lowering, and limited information on periprocedural and late complications. This observation calls for a systematic and longer prospective follow-up of patients after CoA stenting.
Introduction
Coarctation of the aorta (CoA) is a structural defect that accounts for 5-8% of all congenital heart defects. Its natural history is associated with poor outcome1. Experts continue to hold different opinions on the preferred therapy of CoA2. Originally, treatment was limited to medical and surgical therapy. Over the last three decades, balloon angioplasty has become a less invasive alternative, and stent placement has gained acceptance since the first application in 19913.
Given the accumulated worldwide experience with stent placement for CoA in the past 20 years, and the absence of an overview of clinical experience with this procedure in the literature, the current study aims to provide a systematic review of contemporary reports on the effectiveness of stenting for CoA in older children and adults with native or recurrent CoA, with focus on relief of obstruction and lowering of blood pressure.
Methods
On December 10, 2014, a PubMed search of Coarctat*(tw) and stent*(tw), and an Embase search of (coarctat*:de,ab,ti) and (stent*:de,ab,ti) was conducted, limited to publications from 1990 until December 10, 2014, in humans, and written in English. The systematic review was conducted according to the MOOSE guidelines4.
SEARCH STRATEGY
After removing all the duplicates, two reviewers (EMJH and IMG) screened both the titles and the abstracts of all studies. Inclusion criteria were: cohort and RCT studies reporting measurement of diameter or systolic pressure gradient (SPG) or blood pressure before and after stenting, a mean patient age of at least 10 years and a minimum patient age of at least six years. Exclusion criteria were: studies focusing on one specific patient population such as pregnant women, studies focusing only on complications of the stenting procedure, and studies concerning redilation of a previously placed stent. In case of disagreement on inclusion or exclusion, an agreement was negotiated. References of selected articles were cross-checked for other relevant studies. Authors were contacted when a publication could not be obtained or not all the required information could be retrieved from the publication.
DATA EXTRACTION
Microsoft Excel 2008 and Review Manager version 5.1 (The Cochrane Collaboration, 2011) were used for data extraction and statistical analysis. Study design, year of publication and number of patients were extracted.
STUDY CHARACTERISTICS
The extracted patient characteristics included patient age at stenting, native coarctation/recoarctation, proportion of patients with bicuspid aortic valve and the number of patients with other cardiac disorders (congenital/non-congenital). The extracted parameters measured by aortic angiogram were pre- and post-stenting aortic diameter in mm and SPG in mmHg. The pre- and post-stenting systolic blood pressure measurement (mmHg) is the only non-invasive extracted parameter. Procedural complications that were registered included: stent migration, aneurysm formation, aortic dissection, aortic rupture, embolic event and death. Registered complications during follow-up included redilation, aneurysm formation and stent fracture.
STATISTICAL ANALYSES
Continuous variables are displayed as means with 95% confidence limits; discrete variables are displayed as absolute numbers and proportions. Inverse variance weighting was used to correct for differences in population size for the following variables: the aortic diameter pre- and post-stenting, the SPG pre- and post-stenting and the systolic blood pressure pre- and post-stenting. In all studies in which the variance of variables was not reported, the mean standard deviation and the sample size were used to impute the standard error. Early complication risks were calculated for each individual study and pooled on a logarithmic scale with the use of the inverse variance method. A random-effect model was used, given the considerable heterogeneity observed among the studies. In case a particular complication was reported as not occurring in an individual study, then for the analyses it was assumed that 0.5 patient experienced the complication. When an included study did not specify a particular complication in the methods section, did not mention it in the results section, or omitted it from both sections, then the study was excluded from analysis of that complication. Heterogeneity was assessed with the use of the I2 test, the Tau2 test and the chi-square test, and risk of publication bias was assessed through a Begg’s funnel plot. All statistical analyses were performed with Review Manager 5.1.
Results
Figure 1 provides an overview of the systematic review. The initial search strategy resulted in 1,071 publications, of which 1,026 studies were excluded for the following reasons: review (72), case report (297), statement (11), overview (51), editorial (46), book (9), guidelines (4), only complications (71), no measurement of diameter/SPG/blood pressure (179), specific patient groups such as pregnant women and Turner’s syndrome (81), redilation of stents (5), not meeting age criteria (96), <6 patients (24), language other than English (2), not available (10), conference abstract (56), incorrect data description (10), and overlap with other studies (2).
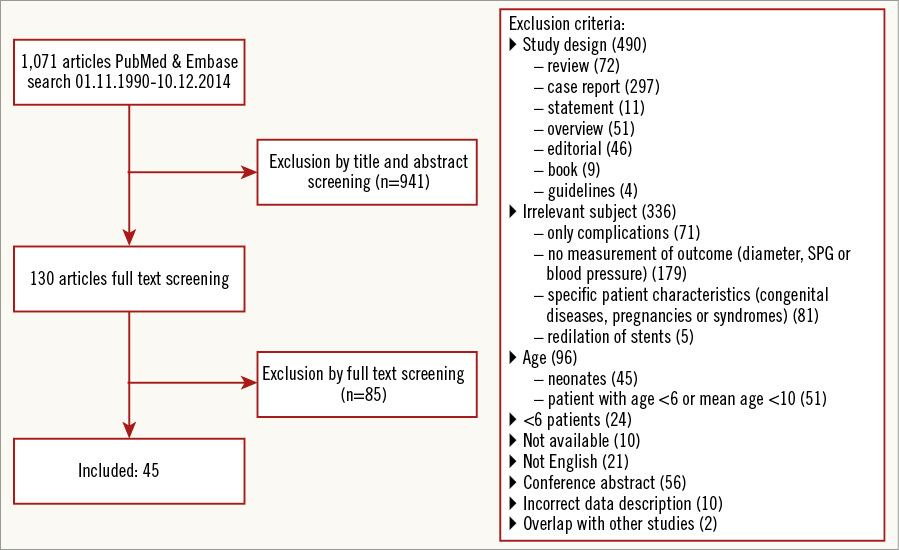
Figure 1. Overview of the systematic review.
The forty-five publications (with a total of 1,612 patients) which were ultimately included reported at least one of the post-stent variables used in the analysis: diameter (28 publications), SPG (40 publications), blood pressure (12 publications)5-49. An overview of the included publications and their characteristics is provided in Table 1.
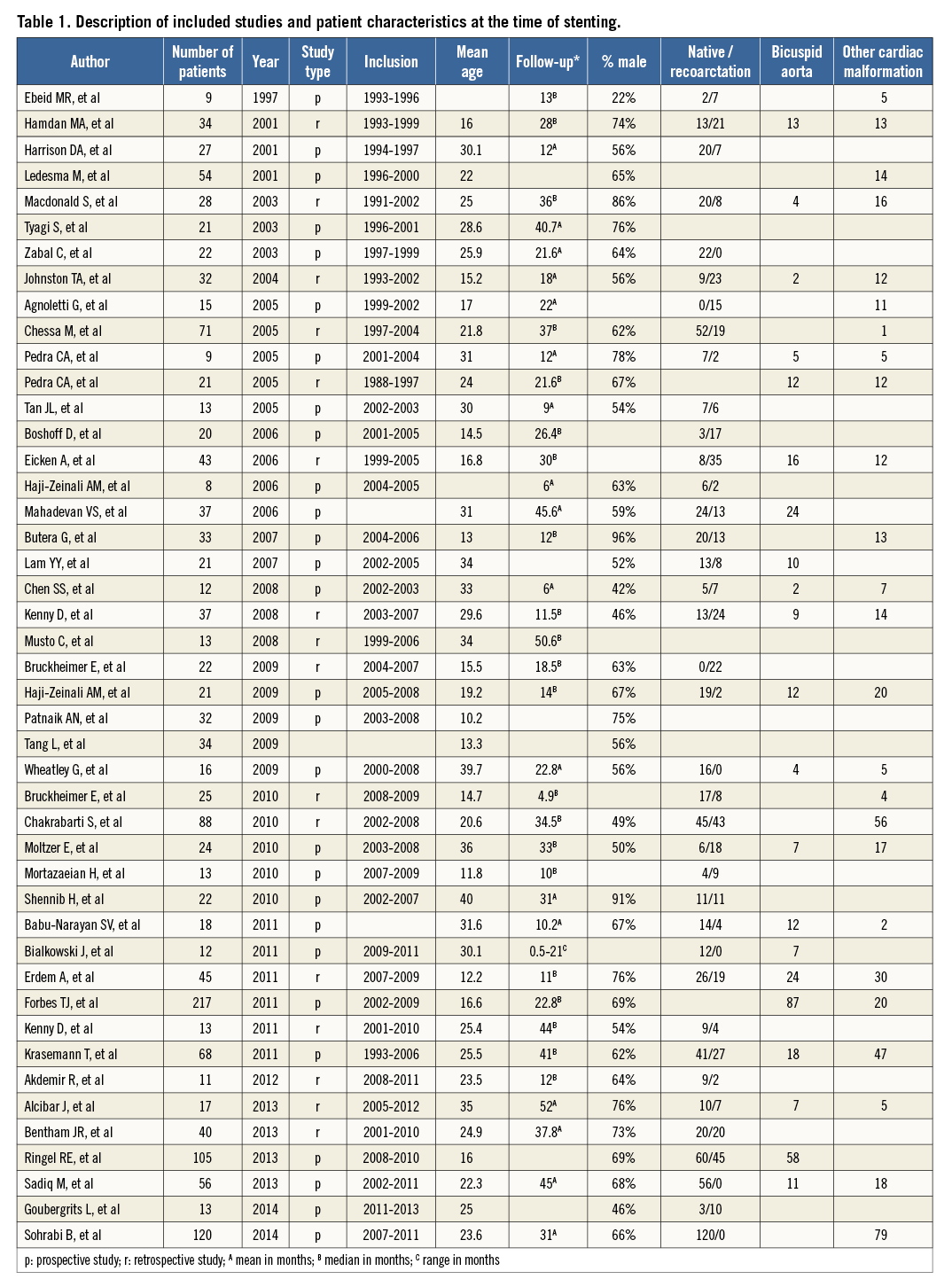
Table 2 displays the individual study measurements and pooled estimates of pre- and early post-procedural aortic diameter, SPG, and mean systolic blood pressure. Figure 2 graphically depicts the changes in aortic diameter (Figure 2A), SPG (Figure 2B), and mean systolic blood pressure (Figure 2C) from pre to early post stenting. Only four studies reported on late post-procedural outcome. Therefore, we did not attempt meta-analysis on late endpoints.
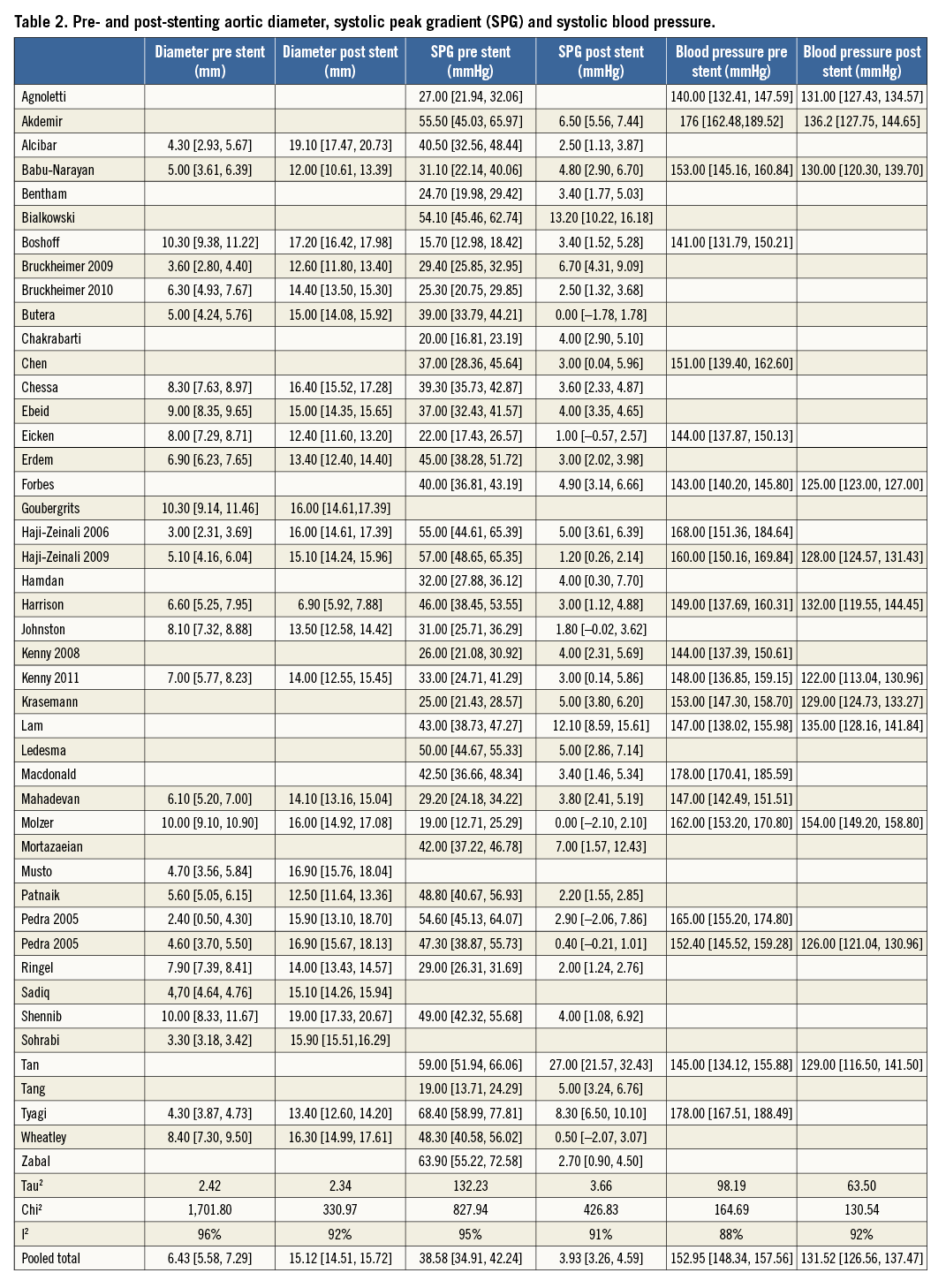
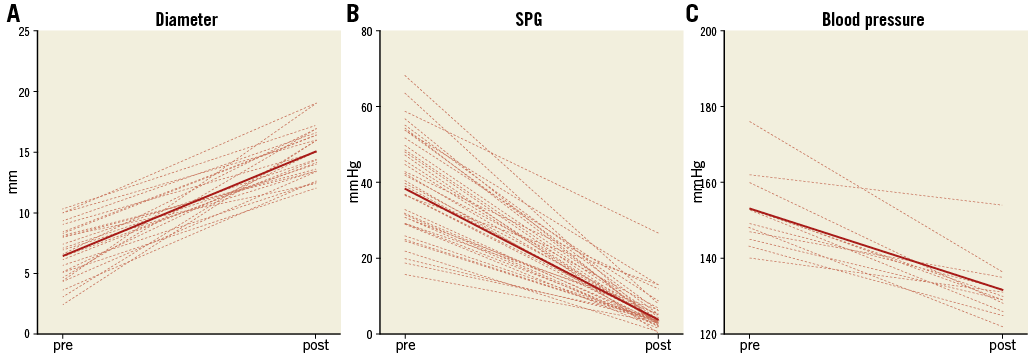
Figure 2. Changes in aortic diameter, systolic peak gradient (SPG) and systolic blood pressure before and early post stenting. A) Aortic diameter. B) SPG. C) Blood pressure.
Considerable heterogeneity was observed, as evidenced by an I2 test for all variables of at least 88%. Therefore, no further analysis of subgroups was attempted. Visual examination of the Begg’s funnel plots suggested no publication bias.
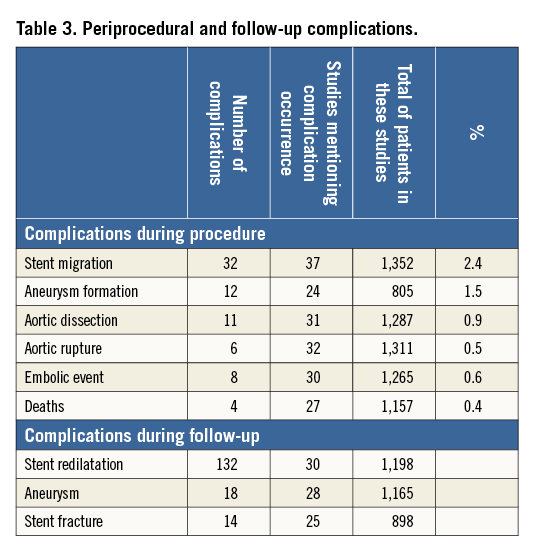
Table 3 shows periprocedural complications and complications during follow-up.
Discussion
This systematic review provides an overview of the effectiveness of CoA stenting in older children and adults in contemporary clinical practice. It illustrates that CoA stenting results in significant relief of aortic obstruction early after the procedure, as evidenced by an increase in CoA diameter, and a decrease in systolic blood pressure and systolic peak gradient. The complication rate is low. In this respect, CoA stenting is indeed effective and safe. Unfortunately, since long-term follow-up data on clinical effectiveness are still lacking, we were unable to provide a systematic review and meta-analysis of the long-term effect of CoA stenting on systolic blood pressure.
FOLLOW-UP BLOOD PRESSURE
The main goal of coarctation stenting is relief of arterial hypertension with a consequent reduction of left ventricular afterload. However, even after successful relief of the obstruction, hypertension may persist. As hypertension is the key determinant of late cardiovascular morbidity and mortality after coarctation repair50,51, it was remarkable that blood pressure after stenting was an underreported variable, being available in only 15 of the 45 studies. Our systematic review shows a significant post-stenting lowering of systolic blood pressure which implies that CoA stenting is a good treatment for immediate blood pressure reduction. However, whether this reduction persists in the long term is more interesting.
An important finding of this systematic review is that there is limited evidence on long-term effectiveness. A few studies have shown that the blood pressure reduction is maintained in the longer term, but significant hypertension may persist in a substantial number of patients, ranging from 25-51%9,30,44,52. As the main goal of coarctation treatment is a durable relief of hypertension, there is a need for more evidence on the course of blood pressure over time after CoA stenting.
EARLY AND LATE COMPLICATIONS
This review shows that periprocedural complications are limited, with stent migration being most frequent (2.4%). Death was uncommon (0.4%), despite the occurrence of aortic dissection (0.9%) and rupture (0.4%).
This review also illustrates the lack of information on longer-term complications such as stent redilation, aneurysm formation and stent fracture. Stent redilation was the most common late complication and was reported to occur in 132 out of 1,198 patients. However, since no data were available on follow-up duration, it was not possible to calculate annual occurrence rates. In addition, stent redilation may have been an elective approach in staged coarctation stenting, so not all redilations should be counted as complications.
Early or delayed aneurysm formation remains a concern after coarctation stenting, but this review does not provide data on the real occurrence in the longer term. A few longer-term studies have reported an incidence of dissection or pseudoaneurysm formation of 1-2%9,30,52. The use of a covered stent does not preclude its occurrence44.
Limitations
All studies in this systematic review were observational and of a retrospective nature. Additionally, most included studies were small, with an average of 34 patients per study. Considerable heterogeneity was found for all endpoints, and therefore we did not attempt any subgroup analyses. The observed heterogeneity can be partly explained by the wide variation among the included studies in patients’ characteristics and age range. A minimum patient age of six years was chosen as an inclusion criterion to prevent the specific issues related to stenting in the very young.
No distinction was made between native coarctation and a recurrent coarctation, since only a few studies allowed for a subdivision. The few studies which made this distinction20 did not find any significant difference in outcomes between stenting for native and stenting for recurrent coarctation.
Importantly, only limited information was available on short-term and longer-term complications of stenting in a subset of the studies. In addition, due to incomplete reporting on complications during follow-up, we were unable to estimate late occurrence rates for these complications. Also, long-term blood pressure was an underreported effect, and the continuing need for antihypertensive medication could not be deduced from the included studies.
Some coarctation patients may have been selected for surgical treatment based on morphology or institutional preference. No information on the number of cases selected for surgery was available.
Conclusions and recommendations
This systematic review of observational studies concerning CoA stenting shows that coarctation stenting in older children and adults is effective with regard to immediate relief of obstruction and the direct lowering effect on blood pressure. However, it also illustrates the lack of evidence regarding safety and late effectiveness concerning durable blood pressure lowering and its potential determinants. Although the immediate effect of CoA stenting is excellent, it is uncertain what can be expected in the longer term. A careful and prospective follow-up of all CoA patients, including systematic periodical assessment of blood pressure, is warranted until better long-term evidence on outcome becomes available. An international multicentre registry of the characteristics and outcome of CoA stenting seems the most logical approach to improve insight into the durability and outcome of CoA stenting. If combined with standard MRI or CT imaging follow-up, information on the occurrence of aneurysm formation or other complications related to stent placement can be obtained.
| Impact on daily practice Coarctation stenting is an effective way to relieve the obstruction and to lower the blood pressure in the short term, with an acceptable complication rate. However, long-term data on its effect on blood pressure and on the occurrence of late complications are lacking. A prospective multicentre follow-up study including MRI or CT imaging may provide these clinically important data. |
Guest Editor
This paper was guest edited by Ran Kornowski, MD, Department of Cardiology, Rabin Medical Center, Petach-Tikva, Israel.
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.