Introduction
In this chapter of Tools & Techniques we discuss key points for choosing and correctly using a guiding catheter. Our aim is not to establish rules but, to develop a step-by-step decision tree, to help operators through the selection process, according to their own personal experience and specific features of the procedures involved.
The following is an introduction and summary for the selection of catheters for the left and right coronaries, arterial and venous grafts, as well as radial and brachial access. Catheter handling and complications related to the guiding catheter will also be discussed. The complete, unabridged e-version with dynamic images can be viewed at www.eurointervention.org.
Guiding catheter selection considerations
The guiding catheter could be the key to a successful or unsuccessful procedure. It must be atraumatic, with appropriate engagement in the coronary ostium and good alignment, and it has to offer adequate backup support. For all these features it is important to analyse the diagnostic angiogram with multiple views, evaluating if the diagnostic catheter fits well the anatomy – taking into consideration the size of the aortic root, the length of the left main, the take-off of the target artery and the location of the lesion. We should then look at the technique that is being planned, studying the required devices that are integrally related to the size of the catheter (6 Fr or ≥7 Fr). It is crucial to anticipate what could happen during the procedure, thinking about the possible solution – the use of new devices or strategies – and consequently the inner lumen and backup support required. For instance, when the planned strategy may require two wires, long or large stents (≥ 3.0 mm), two balloons using the kissing technique, debulking devices with the theoretical risk of a coronary perforation that would need to be sealed with a covered stent, it is better to choose a size ≥7 Fr. Concerning rotational atherectomy, 6 Fr allows the use of 1.5 mm burr, while a 1.75 mm burr needs a 7 Fr catheter, while a 8 Fr catheter is needed for ≥ 2 mm burr. The main differences between the 6 Fr and ≥7 Fr catheters are presented in Figure 1.
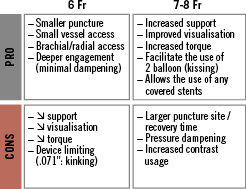
Figure 1. Differences between 6 Fr and ≥7 Fr catheters.
Approaching the left coronary artery from the femoral approach in presence of a normal aorta and a normal length of the left main, Extra backup (EBU) 4 or Judkins left (JL) 4 are good choices, downsizing to 3.5 or upsizing to 4.5, as needed. In the large aorta, it is better to choose EBU 4-4.5 or JL5, turning to the Amplatz left (AL) 2-3 if a better support is needed (Figure 2).
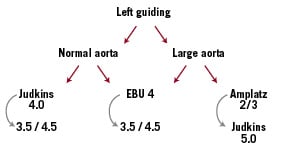
Figure 2. Choice of the guiding catheter for the left coronary artery.
For complex left circumflex (LCX) lesions, the AL catheter assures a deep engagement with the coaxial alignment as well as strong backup support, but it is more aggressive and must be handled very gently in order to avoid vessel dissection. The AL catheter is also particularly useful for the posterior and anterior take-off.
For the right coronary artery (RCA), in the case of a common transverse origin with a normal aorta, Judkins right (JR) 4 allows us to perform most interventions, downsizing to 3.5 or upsizing to 4.5-5, as needed. Another choice is the Amplatz right (AR) 2-3 or Hockey Stick (HS), that are also useful in the large aorta, with AL 1-2 as an alternative, when a strong support is needed (Figure 3).
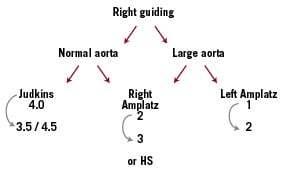
Figure 3. Choice of the guiding catheter for the right coronary artery.
Concerning superior take-off, the choice is oriented toward AL, AR or HS catheters, since their shape warrants good engagement and alignment. For the inferior take-off, good choices are JR, JR short tip, multi-purpose (MP) and the bypass right catheter.
Arterial mammary grafts are usually engaged with the internal mammary catheter (IMC) specifically designed to sit coaxially in the ostium of the internal mammary artery, with contralateral support from the subclavian artery. Percutaneous coronary intervention (PCI) of saphenous vein grafts is often challenging, mostly for grafts to the obtuse marginal. In such cases, when it is not easy to cross the lesion with the filter, AL 1-2 warrant a better backup force, particularly with a 7 Fr catheter. The MP catheter is a good choice for grafts to RCA, and HS could be an alternative for both grafts.
When choosing the radial or brachial access, the EBU catheter is usually a good choice for the left coronary artery, with JL as an alternative. Similarly, for RCA, the JR catheter allows us to face most interventions. Because of the different orientation in the aorta, when using EBU or JL from the right radial artery, the curve should usually be 0.5 cm smaller than that used in the femoral approach with a similar aortic root (i.e., EBU 3.5 or JL 3.5). On the contrary, when engaging the RCA from the right radial approach, it is usually helpful to use a curve that is approximately 1 cm larger (i.e., a JR5 instead of a JR4). When access is achieved from the left radial, conventional curves are usually satisfactory. In case of inadequate support with the previous catheters, the AL catheter may be helpful, mostly for LCX or RCA interventions. A well-balanced trade-off in approaching RCA lesions is the AL 0.75 catheter, which has a less aggressive curve when compared to the AL1, while offering a similar backup support. Concerning grafts, radial access may help to deal with unusual or uneasy origin and take-off of the mammary artery, using IMC or JR catheter.
Good catheter choice must be followed by careful catheter handling. Proper selection of the guiding catheter offers the “passive backup” (that is simply the engagement into the coronary artery), while catheter handling produces the “active backup”. A strong “active backup” is obtained with deep seating of the guiding catheter: deep seating of LAD can be accomplished by counter clockwise rotation and gentle advancing of the catheter over the guidewire, whereas clockwise rotation is required for LCX or RCA.
In patients undergoing PCI, guiding catheter related complications are linked to either embolism or dissection. The JL and MP guiding catheters were associated with the highest amount of aortic debris production. The JR catheters were the least likely to lead to debris production. Embolism can be avoided by allowing sufficient “back bleeding” from the guiding catheter and frequent flushing. The best way to avoid dissection is careful attention to coronary engagement, as well as handling the catheter strictly over the guidewire during insertion or withdrawal.
Finally, the choice of the guiding catheter is a risk-benefit trade-off, where the decision depends on a case-by-case analysis, taking into account the complexity of the lesion, the risk of complications and the familiarity of the operator with the device.

