
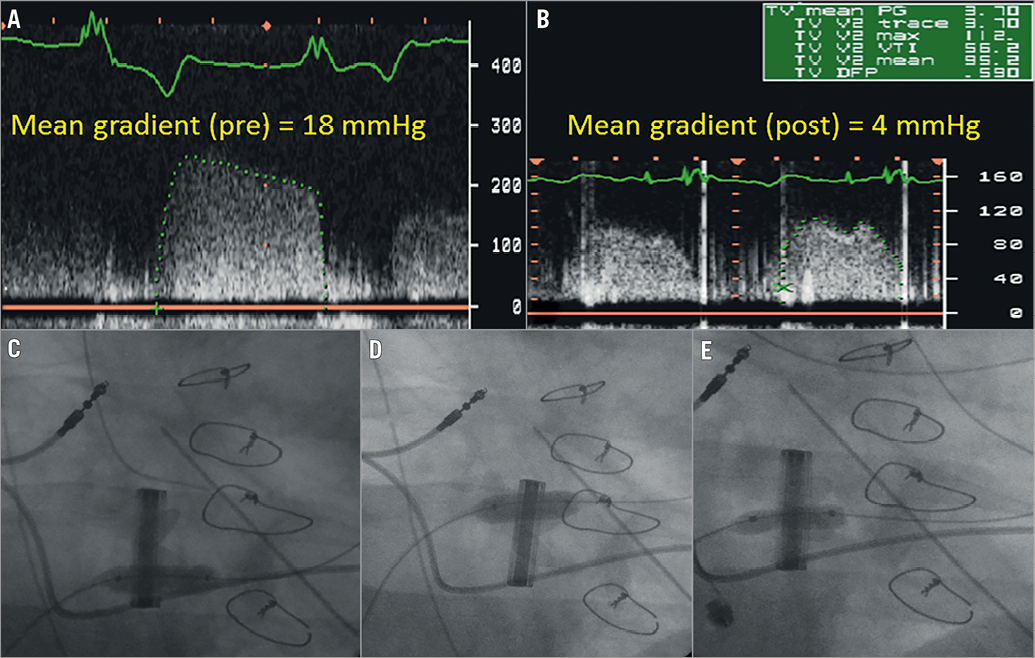
A 62-year-old female, who had a prior history of tricuspid valve (TV) replacement (31 mm mechanical Carbomedics valve) for Ebstein’s anomaly five years earlier, underwent surgical removal of infected spinal hardware followed by reimplantation on the second day. All anticoagulation was withheld for 72 hours. The baseline echocardiogram revealed a normally functioning mechanical TV (mean gradient: 4 mmHg). Two days following the second surgery, the patient became hypotensive, and was noted to have a rising lactate, and worsening renal and liver function. An emergent echocardiogram showed an elevated TV gradient (mean 15 mmHg) suggestive of valve thrombosis. Despite continued infusion of heparin, the patient had worsening haemodynamics and valve gradient (mean 18 mmHg) (Panel A) over the next 12 hours. Thrombolysis was thought to be associated with an unacceptable risk of bleeding complications within 48 hours of two major spinal surgeries. Emergent fluoroscopy revealed fixed mechanical leaflets (Moving image 1). As there were limited therapeutic options, the decision was made to perform balloon valvuloplasty of the thrombosed mechanical valve. We inflated an 8×20 mm Z-MED II™ balloon (B. Braun, Melsungen, Germany) between the valve ring and inferior leaflet to 4 atm (Panel C), and to 6 atm between the valve ring and anterior leaflet (Panel D, Moving image 2). Finally, a 7×20 mm OPTA® Pro balloon (Cordis, Cardinal Health, Milpitas, CA, USA), was inflated at 4 atm in the central orifice (Panel E). Fluoroscopy showed a significant improvement in the motion of the inferior leaflet and a partial improvement in the anterior leaflet motion (Moving image 3). Twelve hours later (i.e., three days post spinal surgery), an intravenous bolus of 50 mg alteplase was given followed by 35 mg two hours later, in an attempt to achieve full haemodynamic response. Repeat transthoracic echocardiography (TTE) revealed a significant improvement in the mean tricuspid valve gradient to 4 mmHg (Panel B). Her clinical haemodynamics improved over the next 24 hours with normalisation of lactate and improvement in aspartate transaminase (AST) and alanine transaminase (ALT) levels. The patient did not develop any clinical or haemodynamic evidence of pulmonary embolism during the hospitalisation. Renal function improved slowly; however, she had a long hospitalisation and was discharged to a skilled care facility for rehabilitation. To the best of our knowledge, this is the first reported case of successful balloon valvuloplasty in a right-sided mechanical valve. This method could be utilised in emergent situations.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Fluoroscopy of the mechanical tricuspid valve. Cine images show fixed leaflets.
Moving image 2. An inflated balloon between the valve ring and anterior leaflet. Improved motion of the inferior leaflet after balloon valvuloplasty compared to Moving image 1.
Moving image 3. Final cine showing significant improvement in the motion of the inferior leaflet and partial improvement in the motion of the anterior leaflet after valvuloplasty.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Fluoroscopy of the mechanical tricuspid valve. Cine images show fixed leaflets.
Moving image 2. An inflated balloon between the valve ring and anterior leaflet. Improved motion of the inferior leaflet after balloon valvuloplasty compared to
Moving image 3. Final cine showing significant improvement in the motion of the inferior leaflet and partial improvement in the motion of the anterior leaflet after valvuloplasty.

