Coronary bifurcation lesions are frequently encountered in everyday percutaneous coronary intervention (PCI)12 and are associated with a high risk of malapposition and adverse clinical events3. To reduce malapposition in the mother branch, the proximal optimisation technique (POT) remains a standard to improve bifurcation PCI4. To detect malapposition in the mother branch, we used an angiographic sign based on contrast medium progression through the inflated POT balloon to evaluate coronary opacification and flow, named the POT-PUFF sign. We hypothesised that the progression of contrast medium (PUFF) through the inflated POT balloon (defined as a positive POT-PUFF sign), could better detect stent malapposition than optical coherence tomography (OCT). We investigated the malapposition rate in the mother branch and the diagnostic performance of the POT-PUFF sign in an academic multicentre prospective study.
A total of 187 patients with chronic coronary syndrome undergoing non-left main bifurcation PCI were included for post-PCI assessment with POT-PUFF followed by OCT to detect stent malapposition. During the final POT, a contrast medium was injected and its successful progression through the inflated balloon was defined as a positive POT-PUFF sign. We assessed the accuracy of the angiographic sign in identifying stent malapposition as compared to OCT. Strut malapposition was defined as a distance of >200 μm between the strut and the vessel wall, and a distance of >400 μm was defined as severe strut malapposition. Stent malapposition was defined as strut malapposition more than 1 mm in length.
OCT and POT-PUFF signs were successfully assessed in 187 non-left-main bifurcations. Four patients were excluded because of suboptimal OCT quality which prevented a complete analysis of the POT segment (Supplementary Figure 1). In 183 bifurcations, the prevalence of malapposition was 22% for the 200 μm cut-off and 11% for the 400 μm cut-off. The study population, lesion characteristics and PCI strategies are summarised in Supplementary Table 1 and Supplementary Table 2. No adverse events were caused by the POT-PUFF.
From the positive to the negative POT-PUFF sign, the risk of malapposition dropped from 70.5% to 6.5% (Figure 1). When evaluated with the cut-off of 200 μm, the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of the POT-PUFF sign were 78%, 91%, 71%, 94% and 88%, respectively. The positive and negative likelihood ratios were 8.5 (4.9-14.7) and 0.3 (0.1-0.4), respectively. The area under the curve (AUC) was 0.84±0.04. For the 400 μm cut-off, the AUC was 0.64±0.05 (Supplementary Figure 2). Interestingly, malapposition occurred predominantly in the proximal third of the POT region as compared to the mid or distal third, 16%, 8% and 3% respectively. Of note, the POT didn’t completely cover the proximal end of the stent in 55 patients (30%).
Coronary bifurcation PCI is associated with a high rate of complications. The PESTO registry identified strut malapposition as a main cause of stent thrombosis3, thus, supporting the need to actively assess malapposition in bifurcation PCI. The lower cut-off of 200 μm also allowed us to consider the milder malappositions more frequently encountered in our daily practice and that are important in bifurcation PCI due to side branch rewiring. The current malapposition depth (>400 μm) was defined as severe acute stent malapposition5. With systematic OCT analysis, we observed frequent malapposition in the POT segment (22%), with half of these being severely malapposed.
The POT-PUFF sign was successfully assessed in all procedures. The effectiveness of the sign was reduced for severe malapposition, which tended to be associated with an uncovered portion of the stent during the POT as the proximal stented area in the mother branch was frequently uncovered (30%). This highlights the importance of covering all of the stented mother branch during POT. With the specificity and negative predictive values both superior to 90%, the POT-PUFF sign could be relied upon to rule out stent malapposition. In fact, by using the POT-PUFF sign to guide bifurcation PCI, the risk of malapposition in the POT segment drops from 70.5% with a positive POT-PUFF sign to 6.5% with a negative POT-PUFF sign. Of note, few cases of malapposition with negative POT-PUFF signs showed focal malapposition. Thus, focal malappositions may not be detected if the progression of the contrast medium is stopped before or after the malapposed portion. Overall, the POT-PUFF sign is a safe and effective angiographic sign that could be implemented in the current practice to improve detection of stent malapposition in the POT.
We acknowledge several limitations of this study. Firstly, the clinical relevance of the detected stent malapposition can’t be evaluated as there was no clinical follow-up. Secondly, stent underexpansion wasn’t assessed in the present study. Finally, the POT-PUFF sign only detects malapposition in the POT segment and can only be trusted if the stent in the mother branch is completely covered by the POT. Thus, it could not replace stent enhancement and intracoronary imaging.
The POT-PUFF sign is a cost-free, safe and effective angiographic sign to identify stent malapposition in the POT segment, which occurs in more than 20% of cases.
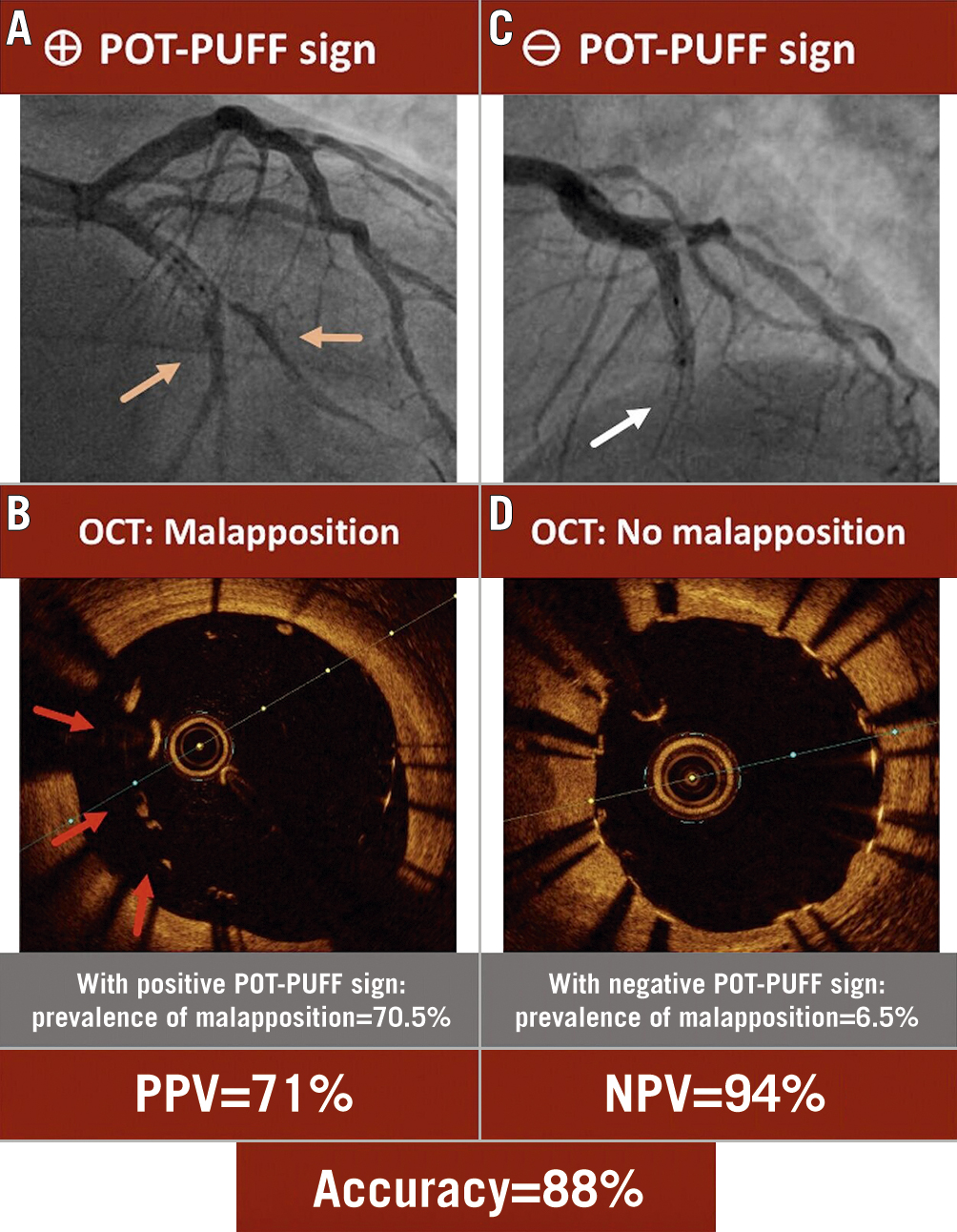
Figure 1. The POT-PUFF sign compared to OCT for identification of stent malapposition. A) The progression of the contrast medium through the inflated POT balloon (orange arrows) defines a positive POT-PUFF sign, suggesting malapposition in the POT segment, as confirmed by OCT (B; red arrows). C) The negative POT-PUFF sign shows no progression of contrast medium through the inflated POT balloon (white arrow) and indicates good apposition in the POT segment (D). NPV: negative predictive value; PPV: positive predictive value
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.