Abstract
Aims: This work aimed to investigate a cohort of patients presenting with stent thrombosis (ST) explored by optical coherence tomography (OCT) to identify the underlying mechanical abnormalities in case of bifurcation lesions.
Methods and results: The PESTO study was a prospective national registry involving 29 French catheterisation facilities. Patients with acute coronary syndromes were prospectively screened for presence of definite ST and analysed by OCT after culprit lesion reopening. The cohort involved 120 subjects, including 21 patients (17.5% of the global PESTO group; median age: 62.6 yrs; 76% male) with bifurcation lesions. The clinical presentation was acute or subacute ST in 34%, late ST in 5% and very late ST in 62% of the patients. The main underlying mechanisms were strut malapposition in 33%, stent underexpansion in 19% and isolated strut uncoverage in 19% of the cases. The proximal main branch was involved in 71%, distal main branch in 52% and jailed side branch in 5% of the patients.
Conclusions: In this cohort, bifurcation lesions represented a limited number of all ST cases. Different sections of the bifurcation could be involved. Although the underlying mechanisms were various, strut malapposition was the most frequently observed cause.
Abbreviations
ACS: acute coronary syndrome
AST: acute stent thrombosis
DES: drug-eluting stent
KBI: kissing balloon inflation
LST: late stent thrombosis
MACE: major adverse cardiovascular events
NSTEMI: non-ST-elevation myocardial infarction
OCT: optical coherence tomography
POT: proximal optimisation technique
SAST: subacute stent thrombosis
STEMI: ST-elevation myocardial infarction
VLST: very late stent thrombosis
Introduction
Although its frequency has decreased over recent years, stent thrombosis (ST) remains a serious complication of percutaneous coronary interventions (PCI), with severe consequences including myocardial infarction and death1,2. ST is a multifaceted process that can be triggered by different factors such as a patient’s clinical characteristics, efficiency of antiplatelet therapy or underlying mechanical stent abnormalities3. The latter could be related to different factors, including the natural history of atherosclerosis, initial PCI pitfalls, cytostatic/cytotoxic agents (in the case of drug-eluting stents) or baseline lesion characteristics4. Notably, bifurcation lesions have been suspected to favour the occurrence of early and late stent thrombosis5-8. Several hypotheses have been advanced to explain these observations9: local flow disturbances within the stented bifurcation creating low endothelial shear stress zones, recirculation and blood stagnation10, delayed strut healing11, device overlapping that creates accumulation of metallic strut layers and cytostatic/cytotoxic drugs (in the case of two-stent techniques), inadequate strut apposition in the proximal part of the bifurcation5. However, there are very few data focusing on the features of bifurcation lesion ST and their potential differences with non-bifurcation lesion ST.
The PESTO multicentre national registry was set up to investigate the usefulness of optical coherence tomography (OCT) in assessing the characteristics and mechanisms of ST among a large cohort of patients4. The present analysis focused on the potential mechanical abnormalities associated with bifurcation lesion ST.
Methods
PATIENTS
This work reports the results from a retrospective post hoc sub-analysis of the PESTO data set. The PESTO multicentre prospective observational registry included patients treated at 29 French catheterisation facilities from January 2013 to October 2014. Patients who were referred with acute coronary syndromes (ACS) were prospectively screened for the presence of confirmed ST. The definite diagnosis of ST was made based on the angiogram and classified as acute (AST), subacute (SAST), late (LST) and very late (VLST), in accordance with the Academic Research Consortium ST definitions12.
Patients were included if the following criteria were fulfilled: 1) TIMI 3 flow was obtained in the target vessel after initial treatment, 2) OCT was deemed feasible by the operator, and 3) the patient gave written informed consent. Exclusion criteria included: age <18 years, duration of symptoms >12 hours, OCT judged non-feasible by the operator.
The clinical characteristics that were collected at baseline included medical history, clinical, biological and angiographic parameters. The data were prospectively entered into a predefined standardised case report form.
The study complied with the Declaration of Helsinki. The Ethics Committee of the Gabriel Montpied University Hospital approved the research protocol.
ACS MANAGEMENT
All patients included in the study were routinely treated in accordance with the European Society of Cardiology guidelines for the management of patients with ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI)13. PCI was performed with a 6 Fr guiding catheter in all patients. The decision whether to use a thromboaspiration device and the options for ST management were left to the discretion of the local operators. The timing for OCT imaging (immediately following restoration of TIMI 3 flow, or during a subsequent control angiogram) was not pre-specified by the study protocol and was chosen by the local investigators according to individual experience and patients’ clinical and angiographic characteristics4.
BIFURCATION LESION CLASSIFICATION AND ANALYSIS
The bifurcation lesions were defined according to the European Bifurcation Club consensus, on the basis of the initial procedure, as follows: a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant side branch (SB)14. The SB was considered clinically relevant if the diameter was ≥2 mm14. The bifurcations were divided into three different sections: proximal main branch (PMB), SB and distal main branch (DMB)14. As part of the protocol, we retrospectively obtained from the local catheterisation facilities the specifications and the dicom files of the initial PCI procedure in the culprit lesion, including the use of the proximal optimisation technique (POT), kissing balloon inflation (KBI) and diameters/lengths of the balloons. Two investigators (M.Y. Bechiri and N. Amabile) centrally analysed the bifurcation lesion Medina classification on the basis of the initial procedure records14.
FD-OCT IMAGE ACQUISITION AND ANALYSIS
Frequency-domain OCT images were acquired using a commercially available system (C7 System; LightLab Imaging Inc./St. Jude Medical, Westford, MA, USA) in all facilities as previously described4. PMB and DMB were analysed by OCT in all patients, but SB-specific analysis was not available in all subjects. The methods used for stent analysis have been extensively described elsewhere4 and are detailed in the Supplementary Appendix. The mechanical abnormalities associated with stent thrombosis were classified as: major stent malapposition, severe stent underexpansion, in-stent ruptured neoatherosclerosis, coronary evaginations, isolated uncovered struts without associated abnormality, edge dissection, edge-related disease progression and intra-stent neointimal hyperplasia with adherent thrombus (Figure 1)4. These abnormalities, as well as the thrombus location within the stent, were localised on the PMB, DMB and SB.
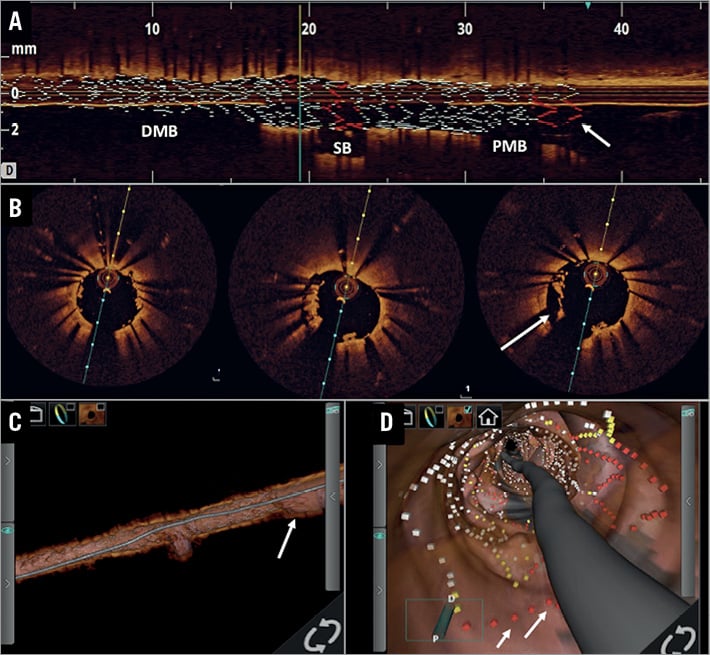
Figure 1. OCT analysis of a subacute stent thrombosis complicating a LAD/1st diagonal branch PCI. The cross-sectional analysis (B) depicts the presence of malapposed struts (arrow) with adherent remnant thrombus in the proximal main branch. These malapposed struts can also be identified in the longitudinal view with stent rendering mode (A), as well as in the 3D reconstruction views (C & D).
CLINICAL FOLLOW-UP
Clinical follow-up was obtained by clinic visits and/or by telephone contact. The incidence of major adverse cardiovascular events (MACE; including cardiovascular death, non-fatal stroke, non-fatal myocardial infarction and the need for urgent target vessel revascularisation) in the 180 days after hospital discharge following ST was prospectively assessed in the cohort.
STATISTICAL ANALYSIS
The statistical analysis was performed with SPSS software, Version 21.0 (IBM Corp., Armonk, NY, USA). Continuous variables are expressed as median and interquartile range. The differences between patient groups were compared using χ² or Fisher’s exact tests (for categorical variables) and the Kruskal-Wallis test (for continuous variables), as appropriate. The incidence of MACE during follow-up was evaluated according to the Kaplan-Meier method in the different groups and compared with the log-rank test. A p-value of <0.05 was considered statistically significant.
Results
BASELINE CHARACTERISTICS
A total of 229 patients in 17 active centres were treated for stent thrombosis during the inclusion period. One hundred and thirty-four patients were screened, and of these 123 provided informed consent. Three patients (2.4%) were excluded from the analysis because of inadequate OCT image quality. The baseline characteristics of the population are given in Table 1.
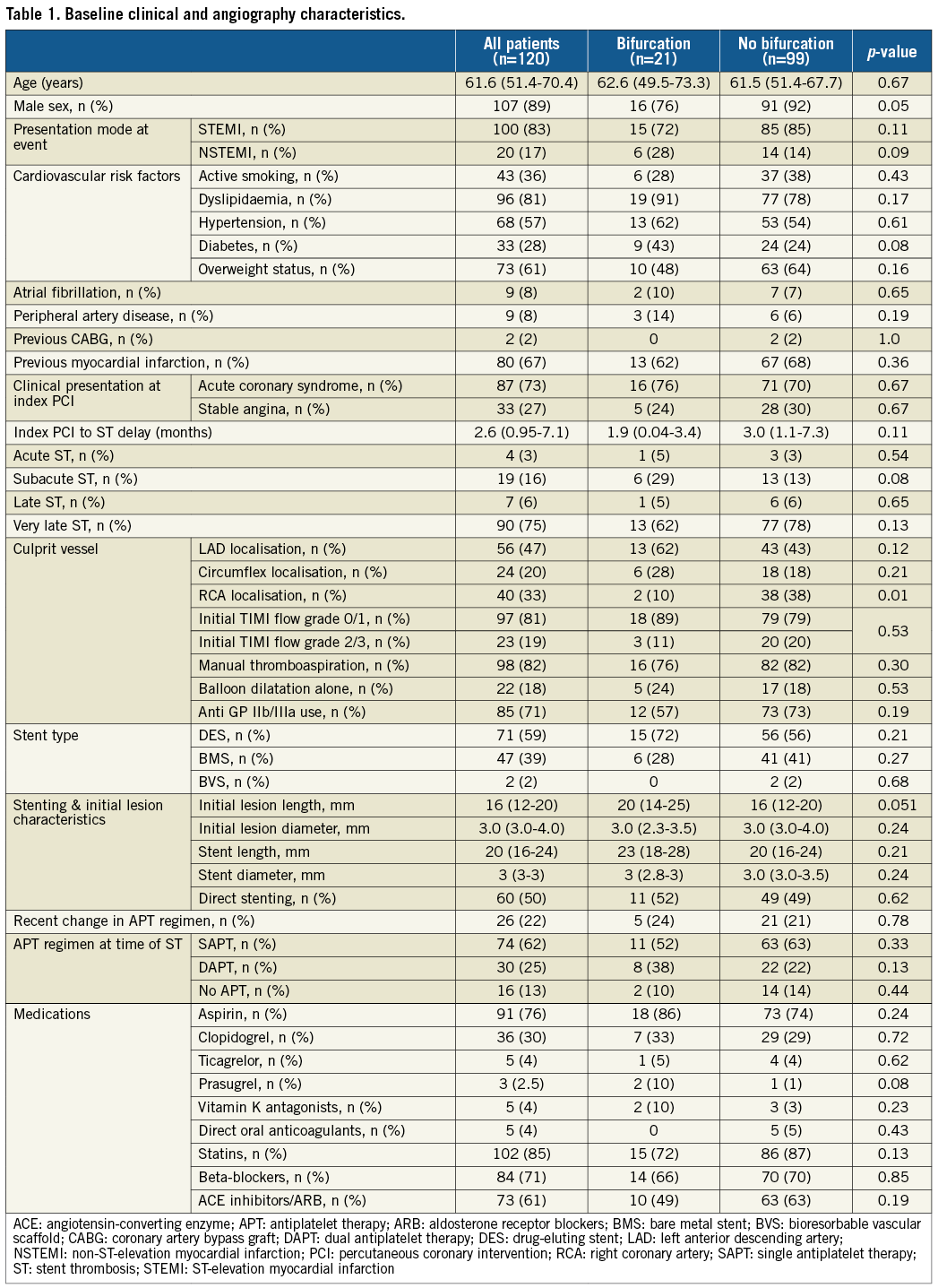
The culprit lesion involved a bifurcation in 21 patients (17.5%). The patients from the bifurcation group were more frequently women compared to the others (Table 1), but there was no significant difference between the two groups regarding the other characteristics. Notably, there was no significant difference in antiplatelet drug regimen between the two groups at the time of the thrombotic event, but we noticed a trend towards a higher incidence of acute/subacute ST in the bifurcated lesions group than in the non-bifurcation lesions group (33% vs. 16.2%, p=0.07).
INITIAL LESION CHARACTERISTICS IN THE BIFURCATION GROUP
The Medina classification of the initial lesion at index PCI was 1,1,0 in n=9, 1,1,1 in n=6, 0,1,1 in n=2, 1,0,0 in n=2, 0,1,0 in n=1 and 0,0,1 in n=1 subjects. The patients from the bifurcation lesion group were treated with one stent implantation in 81% (n=17) and the two-stent technique in 19% (n=4). POT was used in two (10%) and final KBI in 10 (48%) patients. Altogether, there was a total of 11 (52%) patients who underwent POT and/or KBI techniques (one patient underwent both procedures) during the initial procedure. The initial PCI was considered successful (TIMI 3 flow in DMB and SB) in all patients.
OCT ANALYSIS
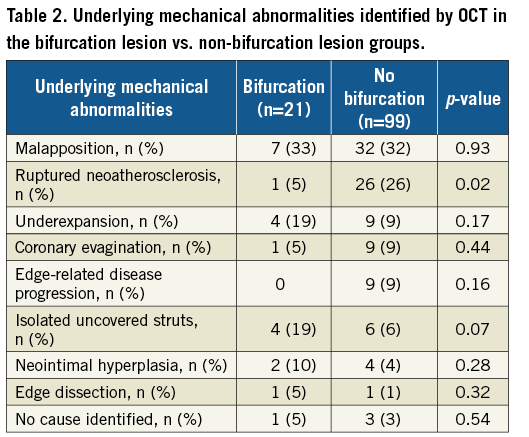
The OCT analysis was performed ad hoc in 30% of the cases and deferred in 70% of the cases. Figure 2 and Table 2 depict results of the OCT analysis. Thrombus was present in all lesion segments but was predominant in the main branch (either PMB or DMB). An underlying mechanical abnormality was observed in 19 patients (91%) from the bifurcated lesion group. These abnormalities were predominantly identified in the PMB (71%), compared to the DMB (52%) and the jailed SB (5%, p<0.001). Strut malapposition (33%), severe stent underexpansion (19%) and isolated uncovered struts (19%) were the most common features in the bifurcation lesions (Table 2). On the other hand, ruptured neoatherosclerotic lesions were significantly less frequent in bifurcated lesions compared to non-bifurcated lesions. The median percentage of stent expansion was, respectively, 76.1% (70.1-92.7) in PMB and 81.5% (72.0-96.7) in DMB (p=ns). The results of OCT analysis within the bifurcated group according to the timing of occurrence are given in Supplementary Table 1.
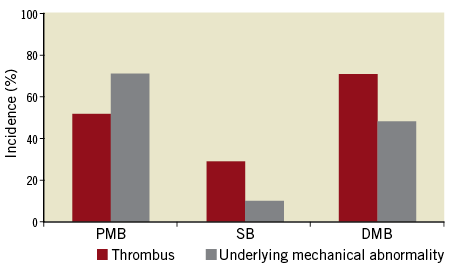
Figure 2. Distribution of thrombus and underlying mechanical abnormalities within bifurcation lesions in the cohort. DMB: distal main branch; PMB: proximal main branch; SB: side branch
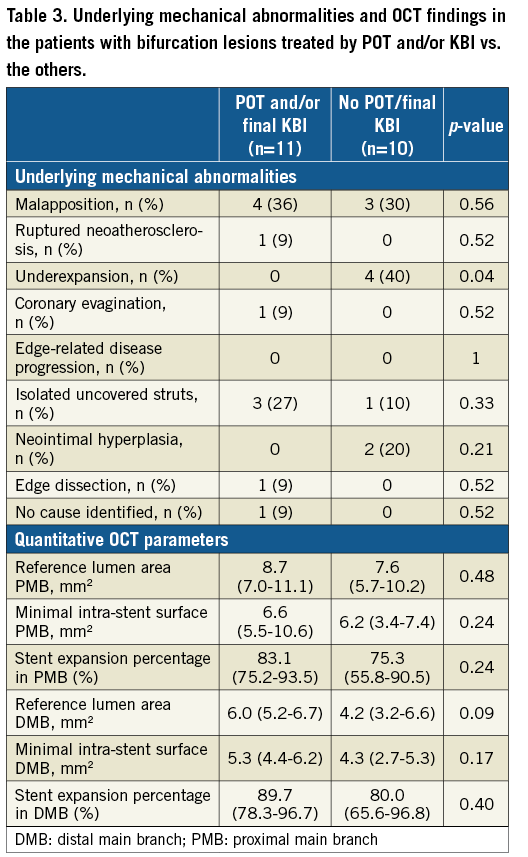
Finally, we analysed the OCT findings according to the use of POT and/or KBI during index PCI (Table 3). We identified that severe stent underexpansion was significantly more frequent in lesions that were not treated by POT/KBI compared to those that were, whereas no other difference was observed for other mechanical abnormalities.
TREATMENT AND CLINICAL FOLLOW-UP
The patients from the bifurcated lesions group were treated by redo PCI in 154 (66%) cases (redo stenting with drug-eluting stent [DES] implantation: n=5, plain old balloon angioplasty [POBA]: n=9) and optimal medical therapy alone (dual antiplatelet therapy+short-term anticoagulation) in seven (33%) cases at the discretion of the local operators on the basis of the OCT findings. The correlations between OCT findings and applied strategies are presented in Supplementary Table 2.
Follow-up data were obtained in 117 (99%) patients. The actuarial freedoms from MACE at six months in patients from the bifurcation and non-bifurcation lesion groups did not differ, being 90.0% (95% CI: 83.3-96.7) and 91.6% (95% CI: 88.8-94.4), respectively (log-rank p=0.81). Furthermore, there was no significant difference regarding actuarial survival from death (bifurcated lesions 95.0% [95% CI: 90.1-99.9] vs. non-bifurcated lesions 97.9% [95% CI: 96.4-99.4], p=0.45) and recurrent stent thrombosis rates (no recurrent ST in either group).
Discussion
The main findings of this analysis from the PESTO cohort are: 1) bifurcation lesions were involved in 17.5% of ST in this series; 2) there was no significant difference between underlying mechanical abnormalities in bifurcated vs. non-bifurcated lesion ST, except for neoatherosclerosis; 3) stent underexpansion was less frequently observed in cases where POT and/or final KBI were applied during index PCI.
Coronary bifurcation treatment is a true challenge for interventional cardiologists in terms of procedural success rates as well as long-term cardiac events5. The optimal management of these lesions remains the subject of considerable debate. Notably, the potentially increased risk for stent thrombosis associated with treatment complexity remains a concern5,9. Hence, the incidence of coronary bifurcation among culprit lesions in ST series ranges from 8% to 62% in the literature1,2,6-8,15-17. In the PESTO cohort, bifurcation lesions were involved in 17.5% of the patients, which is in line with these data. Different studies previously identified coronary bifurcations as an independent risk factor for stent thrombosis6-8. Several reasons could explain these findings. First, the presence of a stent within a bifurcation modifies the local haemodynamics and creates low endothelial shear stress and stagnation areas that could enhance local thrombogenicity10. Moreover, pathology studies have also reported that the flow divider zone displays a high percentage of uncovered struts and fibrin deposition several months after DES implantation, that could represent a substrate for ST11. Furthermore, treatment of coronary bifurcation with two-stent implantation strategies has been suspected of inducing overlapping device segments that could favour drug accumulation (in the case of DES) and multiple metallic strut layers, which could in turn enhance local thrombogenicity18. Finally, stent placement within a bifurcation could also induce inadequate strut apposition (especially in the PMB in cases where the POT or final KBI technique is not used) due to vessel dimension variation along the different segments and promote future thrombotic events5. However, the most recent series did not identify bifurcation lesions as an independent risk factor for ST15,17,19, which could be explained by improvement in PCI techniques and DES design3,9. Hence, although our study was not designed to test this hypothesis, we observed that the percentage of bifurcation lesions in this series was comparable to the percentage reported in all PCI (15-20%)5, which could suggest that no additional extra risk is carried by these lesions.
This sub-analysis of the PESTO cohort is, to the best of our knowledge, the first attempt to focus specifically on the mechanical abnormalities underlying bifurcation ST, identifying such a potential cause in 91% of the cases. In this cohort, malapposition, underexpansion and isolated uncovered struts were the main potential causes of bifurcation ST, whereas ruptured neoatherosclerosis lesions were less frequently identified than in the other group. These observations could be partially explained by the differences in stent age between the two groups. Hence, there was a neat trend towards more frequent AST/SAST and a shorter delay between index PCI and ST in bifurcated lesions. Moreover, we noticed that the mechanical abnormalities were more frequently observed in the PMB compared to the DMB and jailed SB. Based on the current data, it is not possible to establish that the proximal sections of the bifurcation are more prone to mechanical abnormalities because of their anatomical features or because of inadequate PCI technique. Previous studies reported that the proximal sections of bifurcations displayed low endothelial shear stress areas after stenting10, which may affect local homeostasis, vessel dynamics and the healing process20. Interestingly, we also observed that the incidence of underexpansion as the putative ST mechanism was significantly lower in the patients treated with POT and/or final KBI, suggesting a protective effect of these techniques against underexpansion (a major contributor to acute/subacute ST21). We also observed a comparable incidence of malapposition in the two groups, also suggesting that POT and KBI might not fully protect against the risk of malapposition. This finding is not surprising, as positive arterial remodelling is an established contributor to late-acquired malapposition22 that could represent a potential trigger for future ST4. Another explanation for this observation could be that POT/KBI techniques cannot correct all malappositions during initial PCI, especially in case of calcified lesions leading to asymmetrical stent expansion.
Limitations
Several limitations deserve consideration. ST is a multifactorial process that potentially involves stent architecture abnormality and clinical factors, including compliance with antiplatelet drug treatment, and degree of platelet inhibition under therapy. This latter point was not evaluated in this work. Moreover, a substantial number of patients presenting with ST were not screened for inclusion in the study because of an inadequate clinical presentation or the impossibility of restoring TIMI 3 flow without PCI before OCT image acquisition. Hence, although being the largest group of bifurcation ST studied by OCT so far, our sub-analysis might be limited by the small sample size. Thus, definitive conclusions regarding the incidences of the different mechanical abnormalities between bifurcated and non-bifurcated lesions can hardly be drawn. Furthermore, only a limited number of patients (n=3) had a side branch OCT analysis, because of the technical challenge of delivering the OCT catheter to the jailed branch and its potential complications in the setting of ACS, which might have affected the results. Finally, most of the OCT data in the present study were acquired during a deferred procedure. This strategy might have positively influenced the image quality, as the thrombus load decreases over time under these conditions. However, our data might differ from series in which the intracoronary imaging analysis was not deferred23 and thus make generalisation of our conclusions more difficult.
Conclusions
In this prospective ST registry, bifurcation lesions were involved in 17.5% of the cases. OCT analysis identified an underlying mechanical abnormality in 91% of the cases that mostly involved PMB. Malapposition was the leading potential cause of ST. Whether the recent technical improvement in bifurcated lesion stenting could decrease the incidence of thrombotic complications in the future remains to be evaluated.
| Impact on daily practice In patients with bifurcation lesion stent thrombosis, OCT imaging is useful to identify the underlying mechanical abnormality in most of the cases (>90%). This analysis could eventually lead to the most appropriate and tailored ST management strategy on the basis of the imaging findings. |
Funding
This work was funded by an educational grant from Medtronic and St. Jude Medical.
Conflict of interest statement
N. Amabile, C. Caussin, G. Souteyrand, P. Motreff and N. Meneveau have received consulting fees from St. Jude Medical. G. Souteyrand and P. Motreff have received consulting fees from Terumo. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix. Methods.
Supplementary Table 1. Underlying mechanical abnormalities identified by OCT in the bifurcation lesions according to the timing of event (acute/subacute ST vs. late/very late ST).
Supplementary Table 2. Correlations between management strategies and OCT findings in the bifurcation lesions group.
To read the full content of this article, please download the PDF.