Abstract
Aims: A coronary aneurysm is one of the most frequent complications of Kawasaki disease, and yet there is little information concerning the haemodynamic abnormality influenced by the existence of a coronary aneurysm. When blood flow passes through an aneurysm, the turbulence that then occurs means that part of the initial energy is lost, and that energy loss could cause a drop in pressure, such as when passing through a stenotic lesion. The aim of this study is to prove the hypothesis that a giant aneurysm haemodynamically acts in a manner similar to that of stenosis.
Methods and results: The study population consisted of 47 patients with a simple coronary aneurysm after Kawasaki disease. Fractional flow reserve was measured in 32 coronary aneurysms. The fractional flow reserve in non-giant aneurysms was 0.95±0.03 and 0.90±0.03 in giant aneurysms (p=0.0004).
Conclusions: The present data demonstrated that the coronary aneurysm could give rise to a small decline of pressure along the artery. Since no aneurysm demonstrated a fractional flow reserve under 0.75, a simple aneurysm would not cause coronary ischaemia by itself. However, it could trigger a coronary ischaemia in case of multiple coronary aneurysms and a coronary aneurysm with mild stenosis.
Introduction
A coronary artery aneurysm and stenosis are common late complications of Kawasaki disease1. With regard to coronary stenosis, information concerning ischaemic heart diseases in adult patients are very useful in understanding its haemodynamics. However, there is little data concerning the haemodynamics of an aneurysm. When the blood stream enters an aneurysm, it expands and decelerates. During deceleration, a part of the dynamic pressure (kinetic energy) is converted to static pressure (potential energy). When the blood stream exits an aneurysm, it contracts and accelerates. During acceleration, a portion of the static pressure is reconverted to dynamic pressure. This process is the reverse order of the course of the blood stream passing through a actual stenotic lesion, where the blood stream contracts and accelerates when it enters into an area of stenosis and expands and decelerates after passing through the area of stenosis. The process of passing through a stenosis generates turbulence, which means that a part of the initial energy is lost and that energy loss creates a pressure loss. Similarly, this turbulence occurs when blood flow passes through an aneurysm. The current hypothesis is that the existence of an aneurysm haemodynamically acts in a manner similar to that of “stenosis”, namely the onset of a pressure loss. To prove this hypothesis, the haemodynamics of coronary artery aneurysms were investigated.
Methods
The study population included 47 patients with a simple coronary aneurysm after Kawasaki disease (38 males and nine females, mean age 15.8±6.6 years [range two to 29]). The aneurysm was defined as “simple” when the aneurysm was single and did not involve a stenotic lesion. The coronary arteries were assessed by coronary angiography from at least six different views. No patient demonstrated symptoms nor ECG findings associated with coronary ischaemia. None of the patients had experienced acute myocardial infarction or congestive heart failure. A localised dilatation with ≤4 mm internal diameter (or the internal diameter of a segment measures <1.5 times that of an adjacent segment, in children ≥5 years of age) was defined as a small aneurysm; a localised dilatation with an internal diameter from >4 mm to ≤8 mm (or the internal diameter of a segment measures 1.5 to 4 times that of an adjacent segment, in children ≥5 years of age) was defined as a medium aneurysm; and aneurysms with an internal diameter of >8 mm (or the internal diameter of a segment measures >4 times that of an adjacent segment, in children ≥5 years of age) were defined as giant aneurysms. When the aneurysmal length was >2 times the diameter of the aneurysm, it was defined as a spindle-shaped aneurysm2. All patients received antiplatelet therapy (aspirin administration) and an anticoagulant was administered to the patients with a giant aneurysm. All subjects gave their written informed consent, which was approved by Hokkaido University Hospital.
After performing coronary angiography, the fractional flow reserve (FFR) was measured in each coronary artery3. A pressure-sensor mounted guidewire (PressureWire, Radi Medical System, Uppsala, Sweden) was positioned distal to the aneurysm. The mean aortic (Pa) and distal (Pd) pressures were recorded simultaneously under hyperaemic condition and the FFR (Pd/Pa) was determined. Adenosine triphosphate was administered to the target artery to induce hyperaemia. The dose of adenosine triphosphate was 1 µg/kg up to 20 µg4,5. It was administered twice into each coronary artery to confirm that its effect was invariable.
To examine the influence of peripheral vasculature, coronary flow reserve was measured in each coronary aneurysm. Coronary flow reserve was calculated by a Doppler guidewire (Flowire; Volcano, San Diego, CA, USA) in response to bolus intracoronary administration of adenosine triphosphate (same dosage in measuring FFR).
To determine the influence of the aneurysmal size, the FFR was compared between non-giant (small and middle size) and giant aneurysms, which meant that the diameter of the aneurysm was over 8 mm6.
All results are shown as the mean value ±SD. The FFR was compared between two groups by using the Mann-Whitney analysis. A p-value less than 0.05 was considered to be statistically significant.
Results
Fifty-three simple aneurysms were detected by coronary angiogram and FFR could be measured in 32 coronary aneurysms. The aneurysms were located in the left main in 15 patients, the left anterior descending artery in six, the left circumflex artery in four and the right coronary artery in seven. Concerning the size of aneurysms, two were small, 20 were middle and 10 were giant. Only one giant aneurysm formed a spindle shape, which meant the length of the aneurysm was over twice as long as its diameter (Figure 1)6. There was no difference in the age between the groups (Table 1).
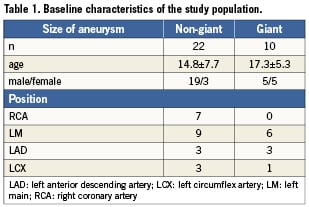

Figure 1. Angiogram of a giant coronary aneurysm with spindle shape.
The mean value of FFR was 0.93±0.04. FFR under 0.75, an indication for coronary ischaemia3, were not observed in any patient. The FFR in the non-giant aneurysms was 0.95±0.03, and in the giant aneurysm was 0.90±0.03 (Figure 2). There was a significant difference in the FFR between the two groups (p=0.0004).
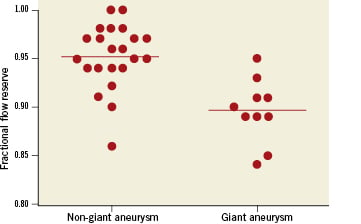
Figure 2. Correlation between the aneurysmal size and fractional flow reserve in patients after Kawasaki disease. There was a significant difference in the fractional flow reserve between non-giant and giant aneurysms (p=0.0004).
The mean value of coronary flow reserve (CFR) was 3.5±1.0. CFR under 2.0, were not observed in any patient. CFR in non-giant aneurysms was 3.6±1.2, and in giant aneurysms was 3.4±0.5. There was no significant difference between the two groups.
Discussion
The present data demonstrated that a coronary aneurysm without stenosis could give rise to a small decline of pressure along the artery. This phenomenon is rheologically possible. In stenosis (Figure 3A), the blood stream accelerates and the pressure is reduced. In dilatation (Figure 3B), the blood stream decelerates and the pressure rises. In an actual vascular stenotic lesion (Figure 3C), however, the blood stream expands after passing through the stenosis. As a result, the loss of energy, which originates from the occurrence of turbulent flow, results in pressure loss. However, the blood stream passing through an aneurysm changes in the reverse order, it expands first and contracts afterwards (Figure 3D). Therefore, real vascular stenosis (Figure 3C) and an aneurysm (Figure 3D) have the same haemodynamic effect.
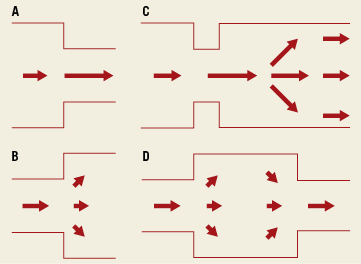
Figure 3. The model of the relationship between the shape of the vessel and blood flow. A) In stenosis, the blood stream accelerates while the pressure is reduced; B) In dilatation, the blood flow decelerates and the pressure rises; C) In a actual vascular stenotic lesion, the blood stream contracts first and expands next; D) In an aneurysmal lesion, the blood flow contracts after expansion.
Yoshikawa and colleagues reported the haemodynamic effects of a coronary aneurysm in in vitro experiments7. They used a bead-shaped model, which consisted of 20 mm diameter beads connected by 6 mm diameter channels. They concluded that the pressure drops through one bead, two beads and three beads-shaped models were equivalent to those of orifices with a 50%, 55% and 70% area reduction, respectively. Their data precisely demonstrated that a coronary aneurysm present after Kawasaki disease could cause stenosis haemodynamically.
Because energy loss is caused by turbulent flow, the steeper the change of diameter, the larger the energy loss. This means that a steep size change may cause a large pressure loss. Therefore, the haemodynamic analysis of the aneurysms was performed on the basis of their size in this study. As expected, the pressure loss was greater in a giant aneurysm. Moreover, the present FFR data demonstrated that the pressure loss of a single aneurysm was not sufficient to induce coronary ischaemia, which concured with in vitro data7. However, a morphological coronary stenosis after Kawasaki disease frequently occurs distal to an aneurysm, and multiple aneurysm formation is not rare. The haemodynamic effect of aneurysms as stenosis could become significant in such cases. It is necessary to analyse the coronary haemodynamics using FFR in the lesion with multiple aneurysms and a single aneurysm with stenosis.
The turbulent flow in the coronary aneurysm could cause thrombus formation, leading to myocardial ischaemia and future stenosis. The giant aneurysms are known to predispose to acute thrombotic occlusion, which can result in myocardial infarction8,9. In the present data, the giant aneurysm demonstrates a large energy loss, which is reflected in the fact that thrombus formation is frequent in giant aneurysms.
The present data demonstrated that pressure loss did not always occur in all giant aneurysms. Although the size gap between channels is one of the most important determinant factors of energy loss, the shape of stenosis is another important determinant. A steep morphological change causes a heavy turbulent flow. However, a smooth shape change creates minimum pressure loss. In the present study, the FFR of the spindle-shaped giant aneurysm was 0.95. This fact may imply that the form of the aneurysm plays an important role in pressure loss, although only one aneurysm formed a spindle shape in the current patients. The reason why the decrease of FFR between the groups with non-giant and giant aneurysms overlapped may be the shape of the aneurysm. One of the most important complications of a coronary aneurysm after Kawasaki disease is thromboembolism, and a giant aneurysm tends to complicate it. Considering that the turbulent flow can cause thrombus (that is to say, energy loss creates thrombus10), thrombus formation may rarely occur in spindle-shaped aneurysms, even in a giant one. However, the small number of subjects in the current study could not clarify the relationship between the degree of a loss in pressure and the type of aneurysm (the size and the configuration). A large cohort of patients will therefore have to be analysed.
Conclusions
A giant coronary aneurysm could give rise to a small decline of pressure along the artery. Although the pressure loss caused by a single coronary aneurysm is modest, it is possible that the influence becomes significant in multiple aneurysms or a single coronary aneurysm with mild stenosis. It is necessary to accumulate further data concerning the coronary haemodynamics using FFR in the lesions after Kawasaki disease.
Limitations
We evaluated the existence of coronary artery stenosis by coronary angiogram. An intravascular ultrasonography is superior in detecting vessel wall pathology, and therefore might be better in evaluating the structure of the coronary aneurysm. However, in this investigation, we judged that the angiography was sufficient to evaluate the stenosis, because we simply needed the information on whether stenosis existed or not. In the future, the evaluation of stenosis by intravascular ultrasonography will be needed when we evaluate the aneurysmal lesion with stenosis.
Conflict of interest statement
The authors have no conflict of interest to declare.

